To compare clinical characteristics, medical activity, and family and social characteristics of individuals with controlled and uncontrolled hypertension.
MethodsThis was an observational study on an alphabetically organized randomized sample of individuals suffering from hypertension in a primary care setting followed by 25 general practitioners at three clinics in the Central region of Portugal in mid-2018. Electronic medical records of individuals with an ICPC-2 classification of hypertension were analyzed. Epidemiologic, family, social and therapeutic data were gathered for descriptive and inferential analysis.
ResultsFrom a total population of 8750 patients classified as having hypertension, a representative sample of 387 individuals (n=369 required for a 95% confidence interval and 5% error margin) was studied. The incidence of uncontrolled hypertension was 56.1%, significantly higher among those living alone (p=00.24) or in a nuclear family (p=0.011), in lower socioeconomic classes (p=0.018), and prescribed anti-inflammatory drugs (p=0.018). The calculated cardiovascular risk was no higher for uncontrolled hypertension (p=0.116). Therapeutic inertia was not found either in number of medicines or in their association (p=0.274). No other studied variables showed a significant difference. Binary logistic regression revealed that living alone or in a nuclear family, and in a family with low socioeconomic level, were associated with uncontrolled hypertension, this model representing 9.6% of the likelihood of having uncontrolled hypertension.
ConclusionsMedical activity in general practice and other settings should, in the light of these findings, ally therapeutic competencies with knowledge gained from studying individual, family and social characteristics in order to improve blood pressure control.
Comparar características clínicas, de atividade médica e de caracterização familiar e social entre populações sofrendo de hipertensão arterial segundo estejam ou não controladas.
MetodologiaEstudo observacional em amostra aleatória por ordem alfabética e representativa com reposição em população de cuidados de saúde primários de vinte e cinco médicos Especialistas em Medicina Geral e Familiar de três unidades de cuidados de saúde primários no centro de Portugal, em 2018 pela análise dos registos clínicos informáticos das pessoas com a classificação ICPC-2 de hipertensão arterial. Estudaram-se variáveis epidemiológicas, clínicas, familiares, sociais e de atividade médica terapêutica. Realizou-se estatística descritiva e inferencial.
ResultadosNum universo de 8750 pessoas com a classificação Hipertensão arterial estudou-se uma amostra de n=387 (tamanho calculado para ic 95% e margem de erro de 5% em n=369). Hipertensão arterial não controlada em 56,1% da amostra, significativamente mais frequente em quem vive só (p=0,024), vive em família nuclear (p=0,011), em situação de mais baixa classificação social (p=0,018), com prescrição concomitante de AINE (p=0,018). O risco cardiovascular calculado é não significativamente mais elevado no não controlo (p=0,116). A inércia terapêutica não se verifica em número de associações e em número médio de medicamentos (p=0,274) não se verificando igualmente diferença para as restantes variáveis estudadas. Viver só, pertencer a famílias com mais baixa classificação social e viver em família nuclear representam 9,6% da responsabilidade de não haver control.
ConclusõesA atividade médica no ambiente de Medicina Geral e Familiar e não só, deve assim aliar as competências terapêuticas com as habilidades de estudo individual e social para a melhoria do controlo da HTA em Portugal.
Cardiovascular disease is the leading cause of death worldwide, accounting for 17.7 million (31%) of total deaths.1–3 The main cause of cardiovascular disease is hypertension, which is thus the major global mortality risk factor.1–3
Treatment of hypertension, even stage one hypertension, reduces the incidence of associated complications, especially myocardial infarction (MI), stroke, heart failure and renal failure.4,5 Most of the international guidelines accordingly recommend a target blood pressure (BP) of <140/90mmHg.6,7 A recent systematic review and meta-analysis confirmed that this target level results in reductions in cardiovascular events and mortality, while adding that systolic BP targets below 140mmHg do not further reduce cardiovascular events and mortality in primary prevention. Levels below 140mmHg only reduce the risk of coronary artery disease in secondary prevention, and even then do not reduce mortality.8
Systolic BP levels have fallen in western Europe, although they remain higher than in North America.9 As a reference, in Canada, 68% of hypertensive individuals had their hypertension controlled (BP<140/90mmHg) in 2013, leading to a significant reduction in mortality and hospitalization due to cardiovascular disease.10 In Portugal, recent studies indicate that the hypertension prevalence ranges between 29.1% and 42.2%, and that the proportions of hypertensives who are aware of their condition, are treated and are controlled rose from 2003 to 2012, although levels of control remain unsatisfactory (estimates ranging from 33.9% to 42.5%).11–13
Various factors influence hypertension control, particularly pathophysiological factors, differences in pharmacological therapy, levels of adherence to therapy, and therapeutic inertia. These factors in turn are influenced by multiple personal and clinical characteristics, including sociodemographic factors, obesity, a history of depression, therapeutic profile and chronology, and the presence of target organ damage and comorbidities. Factors associated with worse control include male gender (linked to earlier development of hypertension), lower literacy,14,15 single civil status,14,16 childlessness,17 and low or intermediate socioeconomic status according to the Graffar scale.14,15,17,18 Obesity, defined as body mass index (BMI) of over 30kg/m2, is also associated with poor control.12,14,19,20 This is attributed to its association with obstructive sleep apnea syndrome and the fact that plasma aldosterone levels increase in proportion to increased BMI.21 Central or visceral obesity correlates with levels of S100 calcium-binding protein B, which is independently associated with the development of hypertension, an effect which is not seen with subcutaneous adiposity.22,23 Central obesity is assessed empirically by measuring waist circumference (WC).6
Uncontrolled hypertension is associated with higher cardiovascular risk, as is target organ damage, although a recent study on the Portuguese hypertensive population found the opposite effect, with higher target organ damage rates in controlled individuals. This can be attributed to increased awareness of the condition and adherence to therapy among patients, and to greater therapeutic vigilance by physicians.24
Elevated plasma creatinine and reduced glomerular filtration rate (GFR) are associated with poor BP control and resistant hypertension.19,25,26 Uncontrolled hypertension can lead to both kidney injury and lower GFR, due to volume expansion and increased systemic vascular resistance.
Multimorbidity, a high number of chronic medical conditions, is associated with less therapeutic inertia and better hypertension control,14,27 while psychological depression has been linked to poor BP control in several studies.14,28,29 Some antidepressants may actually cause hypertension.30
Prescription of a higher number of antihypertensive drugs increases efficacy, is an indicator of less therapeutic inertia, and is associated with better hypertension control.12,14,27 A recent systematic review and meta-analysis revealed no significant differences in effectiveness between the major antihypertensive drug classes, with the exception of alpha- and beta-blockers, which are less effective.31
Treatment-resistant hypertension is an important problem, to avoid which care must be taken to determine therapeutic burden and quality. Antihypertensive therapy should include at least three drugs, of which one should be a diuretic.6
There is growing evidence that chronotherapy, with at least one antihypertensive drug being taken at night, improves hypertension control and reduces long-term morbidity and mortality.24,32
Non-steroidal anti-inflammatory drugs (NSAIDs) are known to interact with antihypertensive medication and to reduce its effect. Concomitant medication with NSAIDs is thus a risk factor for poor hypertension control.21,24
Although much evidence has been obtained, almost all of the above studies call for more robust research into better ways to intervene in the hypertensive population. There is a need to acquire further knowledge of the distribution of relevant variables in Portugal in order to improve hypertension control, since specific national, social and political characteristics could have significant effects on the uncontrolled hypertensive population.
The aim of this work is to determine how the above factors apply to the Portuguese population and to identify priorities for intervention in patients with uncontrolled hypertension. This will improve our understanding of the condition and enable the development of strategies, if possible personalized, to increase hypertension control.
MethodsThis was a cross-sectional observational study on an alphabetically organized randomized representative sample with replacement. When data on BP were missing, the cases immediately before and immediately after were included in the listing for hypertension in the SClínico clinical information system of the Portuguese national health system. The study population consisted of patients followed in primary health care by 25 general practitioners at three Family Health Unit (FHU) clinics of the Baixo Mondego Health Center Group, each in a different municipality: Topázio, Coimbra; Fernando Namora, Condeixa; and Penacova, Penacova. Following approval from the Executive Board and ethics committee of the Regional Health Authority of the Central region and the head of each FHU, the data were collected in July and August 2018 from electronic medical records of the second half of 2017 and the first half of 2018. This task was performed by a suitably trained and qualified medical researcher working in each center.
Patients were included whose records contained codes for hypertension (K85, K86 and K87) of the International Classification of Primary Care, Second Edition (ICPC-2),33 were aged over 18 years, and were not pregnant or diagnosed with diabetes during the study period. The listings were selected by consulting the MIMUF clinical information system by alphabetical order and the sample size was calculated as that required for a 95% confidence interval and 5% error margin. The proportion of this sample to be studied in each FHU was then calculated.
The following data were collected from SClínico:
- •
mean systolic and diastolic BP at the last two office BP assessments in 2017 and the last two in the first half of 2018, on the basis of which control was defined as BP<140/90mmHg and absence of control as higher values or, for systolic hypertension, as systolic BP>140mmHg. The measurements were performed by nurses or physicians, using devices on which information was not recorded;
- •
gender;
- •
age in years, divided into age-groups: 18–49 years, 50–64 years, and ≥65 years;
- •
educational level, classified as low (illiterate or primary/basic education only) or high (secondary or higher education);
- •
civil status: couples (married or civil partnership) or single (unmarried, divorced or widowed);
- •
family unit: nuclear family, extended family, or stepfamily;
- •
socioeconomic level according to the Graffar scale,34 a summary classification based on five criteria (parental occupation, parental educational level, household income, living conditions in the home and state of the neighborhood of residence). The results are divided into five classes based on the total score: class I (score 5–9); class II (10–13); class III (14–17); class IV (18–21); and class V, corresponding to the lowest socioeconomic level (22–25). In our analysis we used three levels: low (classes I and II), intermediate (class III) and high (classes IV and V);
- •
BMI and WC, with obesity defined as BMI>30kg/m2 and central obesity defined as WC>94cm in men and >80cm in women, six in accordance with the measurements recorded in the hypertension listing of SClínico;
- •
cardiovascular risk, calculated by the SClínico software on the basis of BP, total cholesterol, high-density lipoprotein cholesterol, gender, age, and smoking habits, with a 10-year mortality risk of >5% defined as high risk6;
- •
presence of target organ damage (stroke/transient ischemic attack, kidney injury or atherosclerosis) as recorded in the hypertension listing of SClínico;
- •
presence of associated disease in the hypertension listing of SClínico (MI, coronary artery disease, peripheral arterial disease or kidney disease);
- •
GFR in ml/min/1.73m2, calculated using the patient’s weight, age and serum creatinine according to the Cockcroft-Gault formula, to assess renal function. Two groups were defined (GFR≤60 and >60ml/min/1.73m2);
- •
number of comorbidities recorded by the attending physician according to the ICPC-2 classification;
- •
current or previous diagnosis of depression according to the ICPC-2 classification;
- •
antihypertensive medications, identified by their international nonproprietary name: number and pharmacological classes according to the Portuguese pharmacotherapeutic classification (diuretics, beta-blockers, calcium channel blockers [CCBs], angiotensin-converting enzyme inhibitors [ACEIs], angiotensin receptor blockers [ARBs], and others);
- •
night-time chronotherapy as determined from electronic prescriptions;
- •
concomitant prescription of NSAIDs at least twice (excepting aspirin 100 or 150mg).
A descriptive and inferential analysis was performed using chi-square tests for nominal variables, the Mann–Whitney and Kruskal–Wallis tests for ordinal and nominal variables with normal distribution, and binary logistic regression using the enter method for variables that showed a significant difference between controlled and uncontrolled hypertension. A p-value <0.05 was taken to indicate statistical significance.
ResultsOf the total population of 8750 patients classified as having hypertension according to the ICPC-2, 1283 were followed at the FHU Topázio, Coimbra, 2063 in the FHU Fernando Namora in Condeixa-a-Nova, and 4409 at the FHU in Penacova. The sample size calculated for a 95% confidence interval and 5% error margin was 369, distributed proportionally between the three FHUs, which were allocated 80, 90 and 217, respectively.
Table 1 shows that the study population was mostly male and aged over 65 years, with low educational level, mainly married and living in nuclear families, with low or intermediate socioeconomic level. The incidence of uncontrolled hypertension was 56.1% of the overall population, higher among those living alone or in a nuclear family, in the oldest age group, in lower socioeconomic groups, obese, and taking NSAIDs.
Variables in the controlled and uncontrolled hypertension groups.
| Variable | Controlled, n (%) | Uncontrolled, n (%) | p | |
|---|---|---|---|---|
| Gender | Male | 99 (58.2) | 109 (50.2) | 0.071 |
| Female | 71 (41.8) | 108 (49.8) | ||
| Age group | 35–49 years | 15 (8.8) | 15 (6.9) | |
| 50–64 years | 7 (33.5) | 83 (38.2) | 0.737 | |
| ≥65 years | 98 (57.6) | 119 (54.8) | ||
| Educational level | Low | 114 (84.7) | 194 (89.4) | 0.111 |
| High | 26 (15.3) | 23 (10.6) | ||
| Civil status | Married or civil union | 135 (79.4) | 152 (70.0) | |
| Single, divorced or widowed | 35 (20.6) | 65 (30.0) | 0.024 | |
| Family type | Nuclear | 126 (87.5) | 187 (94.9) | 0.012 |
| Extended | 18 (12.5) | 10 (5.1) | ||
| Graffar class | Low (I-II) | 33 (22.6) | 22 (11.9) | |
| Intermediate (III) | 28 (19.2) | 30 (14.9) | 0.018 | |
| High (IV-V) | 85 (58.2) | 150 (74.3) | ||
| Target organ damage | Yes | 36 (9.3) | 43 (11.1) | 0.995 |
| Associated disease | Yes | 33 (8.5) | 35 (9.0) | 0.925 |
| Obesitya | 41 (24.3) | 73 (33.6) | 0.029 | |
| Central obesityb | 134 (84.8) | 178 (86.0) | 0.432 | |
| 10-year CV risk ≥5%, age 40–65 years | 2 (4.3) | 7 (9.2) | 0.268 | |
| Diagnosis of depression | Yes | 37(21.8) | 58 (26.7) | 0.157 |
| GFR≤60ml/min/1.73m2 | 29 (17.5) | 25 (11.7) | 0.072 | |
| No. of antihypertensive drugs prescribed | 1 | 57 (34.3) | 66 (31.4) | |
| 2 | 76 (45.8) | 100 (47.6) | ||
| 3 | 27 (16.3) | 30 (14.3) | 0.274 | |
| 4 | 4 (2.4) | 14 (6.5) | ||
| ≥5 | 1 (0.6) | 5 (2.3) | ||
| No. of antihypertensive drugs per person | 1.9±0.82 | 2.0±1.0 | 0.481 | |
| Chronotherapy prescribed | Yes | 52 (30.8) | 60 (27.6) | 0.288 |
| NSAIDs prescribedc | Yes | 41 (24.3) | 75 (34.6) | 0.018 |
| mean±SD | mean±SD | |||
| BMI, kg/m2 | 28.0±3.9 | 28.7±4.4 | 0.101 | |
| WC, cm | 98.1±10.8 | 97.7±13.0 | 0.668 | |
| 10-year CV risk, age 40–65 years | 1.9±1.4 | 2.5±2.9 | 0.116 | |
| GFR, ml/min/1.73m2 | 92.1±32.7 | 93.6±32.4 | 0.712 | |
| No. of comorbidities (ICPC-2 classification) | 7.9±4.4 | 7.5±4.1 | 0.612 |
BMI: body mass index; CV: cardiovascular; GFR: glomerular filtration rate; ICPC-2: International Classification of Primary Care, Second Edition; NSAIDs: non-steroidal anti-inflammatory drugs; WC: waist circumference.
It should be noted that there was no evidence of therapeutic inertia, as there were no significant differences between groups in the number of drug associations or mean number of different drugs, although there were only five patients with controlled hypertension (3.0%) taking four or more antihypertensive drugs, as opposed to 19 (8.9%) of those with uncontrolled hypertension.
Obesity defined by BMI was associated with significantly greater WC (105.8±15.2cm vs. 94.5±8.4cm, p<0.001), but was not associated with central obesity defined by WC. High 10-year cardiovascular risk (≥5%) was infrequent, but significantly more prevalent in individuals with uncontrolled hypertension.
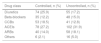
Fewer diuretics and CCBs were prescribed in uncontrolled patients, in whom drugs acting on the renin-angiotensin-aldosterone system (RAAS) were more frequently prescribed. Drug classes other than RAAS agents were prescribed in 58.7% of controlled patients and in 50.0% of uncontrolled patients (Table 2).
Antihypertensive drug classes.
| Drug class | Controlled, n (%) | Uncontrolled, n (%) |
|---|---|---|
| Diuretics | 74 (25.9) | 55 (17.2) |
| Beta-blockers | 35 (12.2) | 48 (15.0) |
| CCBs | 53 (18.5) | 41 (12.8) |
| ACEIs | 78 (27.2) | 102 (31.9) |
| ARBs | 40 (14.0) | 58 (18.1) |
| Others | 6 (2.1) | 16 (5.0) |
ACEIs: angiotensin-converting enzyme inhibitors; ARBs: angiotensin receptor blockers; CCBs: calcium channel blockers.
The prevalence of resistant hypertension (despite administration of three antihypertensive drugs, one of them a diuretic) was 18.4% among uncontrolled patients, while 5.0% of controlled and uncontrolled patients were taking three or more antihypertensive drugs.
Binary logistic regression analysis was performed to determine significant differences between the controlled and uncontrolled groups. This revealed that living alone or in a nuclear family, and in a family with low socioeconomic level, were associated with uncontrolled hypertension, after NSAID prescription and obesity were excluded from the model. This model had Cox and Snell r2 of 0.071 and Nagelkerke r2 of 0.096, thus representing 9.6% of the likelihood of having uncontrolled hypertension (Table 3).
Binary logistic regression analysis using the enter method.
| Variables in the model | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| 95% CI for Exp(B) | |||||||||
| B | EP | Wald | DF | Sig. | Exp(B) | Inferior | Superior | ||
| Civil status | −0.767 | 0.299 | 6.595 | 1 | 0.010 | 0.465 | 0.259 | 0.834 | |
| Step 1 | Graffar class | −0.487 | 0.161 | 9.125 | 1 | 0.003 | 0.614 | 0.448 | 0.843 |
| Nuclear family vs. others | 1.051 | 0.426 | 6.101 | 1 | 0.014 | 2.861 | 1.242 | 6.590 | |
| Constant | 0.700 | 0.685 | 1.045 | 1 | 0.307 | 2.014 | |||
CI: confidence interval; DF: degrees of freedom.
Variables entered in step 1: civil status, Graffar class, nuclear family vs. others.
This multicenter randomized study with replacement in general practice identified significant differences in certain variables related to social factors and medical activity.
Only instruments and values recorded in electronic medical records were studied, and no attempt was made to verify whether BP was measured according to standard practice.6,35
Other variables that can only be measured by means of interviews or questionnaires are not recorded in SClínico, even though they may be key to improving hypertension control. These include adherence to therapy, patient concerns about their medication, knowledge about hypertension, and patient enablement and empowerment (the assumption of responsibility by the hypertensive individual for their situation and their participation in the application of therapeutic measures).
The rate of hypertension control found in this study was 43.9%, compared to 35.6% in a report from the Portuguese Directorate-General of Health in 2015 and 42.5% in a 2014 study.12,13
The prevalences of target organ damage and of associated disease (20.4% and 17.6%, respectively) were higher, albeit without statistical significance, in uncontrolled patients, which is in line with the findings of other studies4,5,18 but not with those of a Portuguese study on a sample of 201 individuals out of a population of 972 hypertensive patients, in which target organ damage and associated disease were found in 17.4% and 27.9%, respectively, which calls into question the quality of the classifications entered by the physicians responsible for filling in the records.24
We did not study hypertension-related mortality since deceased individuals do not have active records in the general practice database and were therefore not selected.
In agreement with the literature,14,15 uncontrolled hypertension was more likely to be associated with lower educational level (63% vs. 47% in those with higher educational level), although without statistical significance. The influence of social variables (civil status, type of family and Graffar score) is also in line with previous studies,14–16,18 with uncontrolled hypertension being more frequent in single, divorced or widowed individuals, those living in nuclear families, and those in lower socioeconomic classes. Our results thus confirm those of non-randomized studies.
Obesity, defined as BMI>30kg/m2, has also been associated with absence of control.12,14,19,20 This was also seen in our study, although there was no such association with mean BMI. The presence of central obesity as defined by WC did not differ between controlled and uncontrolled subjects, but was significantly more frequent in subjects defined as obese according to BMI, supporting the findings of guidelines and other studies.22,23
Mean cardiovascular risk among subjects aged 40–65 years did not differ significantly between controlled and uncontrolled patients, in agreement with previous findings,6,20 nor did the proportion with 10-year risk of ≥5%, but there was a significantly higher risk in those with uncontrolled hypertension, although the prevalence of this elevated risk level was low. This may be due to antihypertensive or other medication, but this aspect is not analyzed in our study. High cardiovascular risk should alert physicians to the need for earlier and more intensive therapy, as well as helping to focus the attention of the hypertensive individual on the scope of the problem.
Depression had an overall prevalence of 24.6% in this study and was more frequent in the group with uncontrolled hypertension (26.7% vs. 21.7%), although without statistical significance. This has also been seen in previous studies.14,28,29 It should be noted that we studied the association between the two entities, not their causal relationship. When depression has been diagnosed after a diagnosis of hypertension, the Portuguese guidelines state that caution should be exercised in the prescription of antidepressants.30
Serum creatinine and GFR were not significantly associated with uncontrolled hypertension. This may be due to various factors, including the fact that most of the medications prescribed in this study act on the RAAS, unlike in other studies.19,25,26
Multimorbidity is associated with less therapeutic inertia and better hypertension control,14,27 but this was not seen in the present study, although as we studied only chronic conditions that were recorded and followed by the physicians responsible for completing medical records, this may have been affected by information bias.
Chronotherapy, with at least one drug being taken at night, did not have a significant effect in our study. It was not frequently prescribed, particularly in individuals with uncontrolled hypertension, which highlights the need to take more advantage of the known benefits of this treatment.24,32
With regard to medical activity, more drugs were prescribed in those with uncontrolled hypertension, both in therapeutic associations and in the mean number of drugs prescribed per patient, although without statistical significance. Again without statistical significance, diuretics and CCBs were more often prescribed in those with controlled hypertension, while beta-blockers, ACEIs, ARBs and other drugs including rilmenidine and methyldopa, were more often prescribed in those with uncontrolled hypertension. This may be the reason that only 3.0% of those with controlled hypertension were taking four or more antihypertensive drugs, as opposed to 8.8% of those with uncontrolled hypertension.
NSAIDs (excluding COX-2 inhibitors) were significantly more often prescribed in those with uncontrolled hypertension. NSAIDs are known to have a hypertensive effect36 and are widely prescribed in Portugal, even more in older patients, in whom osteoarthritis is more prevalent, although this is not always inflammatory in nature.37–39
Binary logistic regression in our analysis ruled out prescription of NSAIDs and obesity according to BMI as variables significantly affecting control of hypertension, and clearly highlighted the importance of social factors in the problem of absence of control.
The above findings strongly suggest that the main factors influencing hypertension control are not those relating specifically to medical activity in terms of drug prescription, but rather social variables, on which general practitioners should focus instead, in order to gain a better understanding of the factors that lead to absence of control. Our analysis indicates that, rather than variables such as obesity or prescription of NSAIDs, absence of control is due to social characteristics that, although not amenable to alteration by physicians, should can and should be the subject of different interventions, such as those that can be offered by other health professionals whose work is linked to that of general practitioners in the setting of primary health care, such as occupational therapists, exercise specialists, nutritionists and social workers.
It is clearly necessary to adopt measures other than pharmacological therapy, and therefore support needs to be provided to assist hypertensive individuals in their daily lives to take more exercise, improve their diet and implement other aspects of a healthier lifestyle.
Further light could be shed on the results of this study by seeking answers to questions such as who cooks in the household and where meals are taken, to what extent individuals can adopt new eating habits, how physical exercise can be promoted both in the family and in society at large, especially in cities, to what extent hypertensive individuals understand the nature of their disease, what is the best motivation to maintain adherence to pharmacological and non-pharmacological therapy, and – in general terms – how ready society is to adopt new habits.
It is also of crucial importance to facilitate access to data from the hypertension listing in SClínico in order to assess individuals, families and social characteristics and their relationship with hypertension.
Cohort studies are therefore required, both retrospective and prospective, that will provide further information relevant to our results.
Possible limitations of this study include possible bias due to the fact that the data were collected by four different observers and that introduction of data in the clinical records was the responsibility of the attending physician, although the latter aspect can be assumed to be improving due to the application and achievement of performance indicators.40 A positive point is that the study sample was randomized and representative of the overall population.
ConclusionsThis study revealed significant differences between those with controlled and uncontrolled hypertension in terms of social variables including type of family, socioeconomic level, obesity and prescription of NSAIDs. Cardiovascular risk was higher among uncontrolled individuals aged 40–65 years, although without statistical significance. Based on the characteristics of the study sample and how it was obtained, our results can be generalized to the Portuguese population. Medical activity by general practitioners and other physicians should thus ally therapeutic competencies with knowledge gained from studying individual, family and social characteristics in order to improve BP control in Portugal.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Martins RdS, et al. Pessoas que sofrem de hipertensão arterial: implicac¸ões na atividade médica das diferenc¸as entre os controlados e os não controlados. Rev Port Cardiol. 2019;38:745–753.