Primary cardiac tumors are rare, with an incidence ranging from 0.0001% to 0.030%; 80% are benign, while sarcomas account for 95% of malignant tumors.
The authors report the case of a 75-year-old patient with a giant mass in the left atrium. The final diagnosis was of an undifferentiated cardiac sarcoma. This tumor represents a real challenge not only for timely diagnosis, but especially the therapeutic approach to adopt.
Os tumores cardíacos primários (TCP) são muito raros, com uma incidência de 0,001 a 0,030%. Os tumores benignos são os mais frequentes, representando cerca de 80% dos TCP; os sarcomas são responsáveis por 95% dos tumores malignos.
Os autores relatam o caso de uma doente de 75 anos de idade a quem foi diagnosticada uma massa na aurícula esquerda, que impressionava pelas suas dimensões. O diagnóstico final revelou tratar-se de um sarcoma cardíaco indiferenciado. Este tumor representa um verdadeiro desafio não só no diagnóstico atempado, mas principalmente a nível da terapêutica a instituir.
Primary malignant cardiac tumors, of which sarcomas are the most frequent, are extremely rare.1
Cardiac sarcomas are of mesenchymal origin and can affect any part of the heart. The most common types are angiosarcoma, undifferentiated cardiac sarcoma (UCS), malignant fibrous histiocytoma and leiomyosarcoma.2,3 They can develop at any age, but are more common in the fourth decade of life, occurring with equal frequency in both sexes.4
Around half are located in the left atrium (81% in the case of UCS). UCS is characterized by a lack of a specific histological pattern; it originates in fibroblasts or histoblasts, and due to its shape and location is often initially diagnosed as a probable myxoma.2 Valve involvement is reported in 50% of cases. It is less likely to metastasize than other sarcomas such as angiosarcoma, and patients most frequently die of local heart disease before metastases develop. Clinical manifestations of these tumors can include heart failure, dyspnea, acute pulmonary edema, syncope, systemic embolism, constitutional symptoms and fatigue.5 Diagnostic exams are those used to assess cardiac lesions in general, namely transthoracic and transesophageal echocardiography, magnetic resonance imaging (MRI) and computed tomography (CT).3,5
Macroscopically these tumors tend to be yellowish-white with areas of necrosis and extensive infiltration of the myocardium and cardiac structures. Histological study provides a definitive diagnosis. Microscopically they may be heterogeneous with a storiform pattern, marked pleomorphism, elevated mitotic activity, and at times foci of necrosis. Immunohistochemical analysis is crucial; epithelial, neuronal and endothelial markers are usually negative and vimentin is typically positive.4
The recommended treatment is complete surgical excision whenever possible, but this is often difficult due to extensive invasion of cardiac structures or to tumor location that would require complex surgical reconstruction.4 If resection is incomplete, over 90% of patients do not survive more than a year, even with adjuvant therapy. There is no firm consensus on non-surgical treatment: some authors recommend chemotherapy, but some studies have found no benefit6,7; while postoperative radiotherapy is an option, it is also of limited value due to its cardiotoxicity. Heart transplantation may be considered in selected patients.4
The authors describe the case of a patient diagnosed with a large UCS, followed by a review of the literature, clinical characteristics and the diagnostic exams used in this very rare and little documented disease, for which there is as yet no standard treatment.
Case reportWe present the case of a 75-year-old Caucasian woman with a known history of essential hypertension and type 2 diabetes, medicated with oral antidiabetics (metformin 850 mg twice daily and vildagliptin 50 mg twice daily) and a diuretic (furosemide 20 mg daily).
She had been suffering from constitutional symptoms, including losing 20 kg in weight, over the previous 12 months, and dyspnea on moderate exertion and lower limb edema in the six months before admission. She was admitted to the emergency department due to dyspnea on minimal exertion, orthopnea and paroxysmal nocturnal dyspnea. On physical examination she was tachypneic with jugular distension at 45° and moderate lower limb edema of the entire leg; she was hemodynamically and electrically stable, with oxygen saturation of 90% in room air. Cardiac auscultation revealed a grade II/VI systolic murmur at the left sternal border and a grade II/VI apical mid-diastolic murmur, and blood gas analysis was compatible with type 1 respiratory failure. The ECG showed sinus rhythm with non-specific ventricular repolarization abnormalities. The following alterations were detected by laboratory testing: normochromic normocytic anemia (hemoglobin 9.2 g/dl), C-reactive protein 3.1 mg/dl, pro-brain natriuretic peptide 7332 pg/ml and D-dimers 2 mg/ml; myocardial necrosis markers were negative. The chest X-ray revealed increased cardiothoracic index and bilateral pleural effusion. Thoracic CT angiography was then performed due to suspicion of pulmonary thromboembolism, one of the initial diagnostic hypotheses, but the exam ruled this out, showing a medium-sized bilateral pleural effusion, a large lesion in the left atrium and mediastinal nodules less than 1 cm in size.
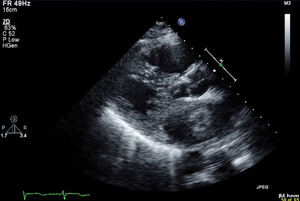
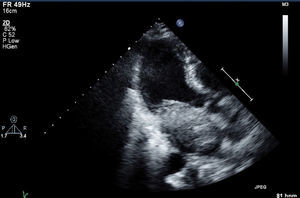
In the light of the clinical setting and the findings of initial exams, the patient was admitted for treatment and further investigation. Transthoracic and subsequently transesophageal echocardiography revealed a well-defined mass in the left atrium attached to the interatrial septum, measuring approximately 5.4cm×3.2cm and protruding into the left ventricle in diastole (Figures 1 and 2), significantly obstructing mitral flow (peak gradient 20mmHg and mean gradient 13mmHg; functional area 1.0cm2 by the pressure half-time method and 0.8cm2 by the continuity equation). Severe tricuspid regurgitation was also observed (dilatation of the annulus to around 41mm) and pulmonary artery systolic pressure was estimated at 100mmHg.
As part of surgical evaluation, cardiac catheterization was performed, which revealed only non-significant vessel wall disease in the mid anterior descending coronary artery. Given the size of the lesion and the resulting obstruction, the patient was rapidly proposed and accepted for surgery. In view of the location of the mass and the clinical setting, the initial diagnostic hypothesis was a cardiac myxoma.
Five days after admission the patient underwent surgical excision of the lesion, the interatrial septum being opened via the fossa ovale and the incision extended to the left atrium (Figure 3). A tumor was observed invading the interatrial septum and part of the left atrial roof and protruding through the mitral valve, the anterior leaflet of which it appeared also to have invaded. The mass was excised; on visual inspection it was nodular with an uneven surface, and consisted of relatively soft and elastic tissue with hemorrhagic areas, weighing around 55 g and measuring 7.4 cm × 5 cm × 3 cm (Figure 4). On direct observation the diagnosis of myxoma appeared less likely.
After tumor excision, severe mitral valve regurgitation was seen, with failure of central coaptation, and the valve was replaced with a biological prosthesis, removing the anterior leaflet and preserving the posterior leaflet. Inspection of the tricuspid valve and intraoperative transesophageal echocardiography revealed moderate rather than severe regurgitation and it was decided not to perform valvuloplasty.
The operation took longer and was more complex than expected and the postoperative period was complicated by a stroke on the second day manifested clinically by left hemiparesis, predominantly of the arm. Brain CT showed a partial infarction of the anterior circulation.
At discharge the patient was significantly improved in neurological terms, with only residual paresis of the arm. Due to the prolonged postoperative period (one month of hospitalization) she was discharged to a continuing care unit, where she began rehabilitation. Anatomopathological study revealed cellular proliferation with marked pleomorphism, atypical mitosis and positivity for vimentin, these results being compatible with UCS. The same histopathological characteristics were found in the resected anterior mitral leaflet and in the biopsy specimen of the preserved subvalvular apparatus.
After discussion of the therapeutic options, a multidisciplinary decision was taken not to proceed with chemotherapy or radiotherapy. Repeat echocardiography two months after the surgery showed no images suggestive of intracardiac masses and CT did not reveal signs of metastasization or pleural effusion. Almost six months after the operation the patient continues in a rehabilitation and physiotherapy program, with residual neurological deficits mainly in the arm, and is in NYHA class II.
DiscussionThere have been few cases reported of UCS, particularly as large as the one described, which occupied practically the entire left atrium.
Due to its location and size, the mass was initially thought to be a myxoma, but visual inspection of the surgical specimen cast doubt on this diagnosis, which was ruled out by pathoanatomical study.
In this patient the tumor's clinical manifestations were essentially heart failure and constitutional symptoms. On initial observation the patient presented a large lesion and significant symptoms, and was therefore rapidly proposed for surgery.
Echocardiography is extremely useful in the assessment of any cardiac lesion, particularly of this type.3 The high resolution of contrast CT also helps characterize lesions.5 However, MRI is superior in several ways, especially for differential diagnosis,8 and would have been valuable in the case presented, but could not be performed promptly.
With regard to adjuvant therapy, the decision was taken not to proceed with radiotherapy or chemotherapy. According to the literature (which consists of a few case reports and small series), if complete resection is impossible, over 90% of patients die within a year even with adjuvant therapy. Some studies have found that chemotherapy conferred no benefit7; there have been no clinical trials specifically on UCS, due to its rarity, and chemotherapy regimes are based on those for extracardiac sarcomas. Radiotherapy is also used as adjuvant therapy for incompletely resected extracardiac sarcoma, but its value in the treatment of cardiac sarcomas is limited by its cardiotoxicity, and its role in the treatment of such tumors is unclear.4
The prognosis of cardiac sarcoma is generally very poor whatever treatment is used.3,4,7
In view of our patient's clinical course, the results of the histological study (showing invasion of the subvalvular apparatus) and the state of the art, and after careful weighing of risks and benefits, it was decided not to proceed with chemotherapy or radiotherapy.
ConclusionThe rarity of cardiac sarcoma means that this tumor represents a challenge for diagnosis and especially the therapeutic approach to adopt.
A high index of suspicion is required for timely diagnosis and treatment. Surgical excision is the only treatment that has been shown to improve symptoms and survival in selected patients. The role of adjuvant therapy remains unclear.
Further studies, particularly biomolecular and genetic, are required to improve the characterization, management and treatment of these tumors, with a view to improving their prognosis.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflict of interestThe authors have no conflict of interest to declare.
We thank Dr. Fátima Neves and Dr. Couceiro, of Centro Hospitalar de Vila Nova de Gaia/Espinho, Hospital Eduardo Santos Silva.
Please cite this article as: Ferreira C, Martins D, Pereira R, et al. Lesão tumoral gigante na aurícula esquerda: um caso incomum de sarcoma cardíaco indiferenciado. Rev Port Cardiol. 2013;32:713–716.