The authors report the case of a 74-year-old man, with a history of chronic obstructive pulmonary disease (COPD), GOLD grade 3, stable for the past two decades, who was admitted to our center with severe right heart failure.
The chest radiograph showed moderate heart enlargement mainly of the right atrium and pulmonary artery, similar to previous chest radiographs in the previous 20 years. The transthoracic echocardiogram showed a pulmonary artery aneurysm (PAA), dilatation of the right chambers with pulmonary artery systolic pressure of 52 mmHg, and preserved right ventricular systolic function. A thoracic computed tomography scan confirmed the presence of a giant PAA 72 mm in diameter.
The patient was started on high-dose diuretics, with significant clinical improvement.
After optimization of medical therapy right heart catheterization was carried out with the patient in optimal clinical condition, which revealed mild precapillary pulmonary hypertension with a mean pulmonary artery pressure of 26 mmHg.
On the basis of the clinical and imaging findings a stable, giant, high-pressure, PAA was diagnosed secondary to pulmonary hypertension induced by COPD, with a 20-year follow-up without need for surgical repair, which helped in our decision to maintain medical surveillance. The recent onset of heart failure is explained by the unfavorable evolution of COPD.
This case may change the attitude expressed in previous studies favoring the choice of an invasive approach to treat giant high-pressure PAAs, instead supporting the maintenance of medical treatment.
Os autores relatam o caso de um homem de 74 anos, com história de doença obstrutiva pulmonar crónica (DPOC), categoria C de GOLD, estável nas últimas duas décadas, admitido por insuficiência cardíaca grave de câmaras direitas.
Na radiografia torácica era evidente o alargamento da silhueta cardíaca, em particular da aurícula direita e artéria pulmonar, sendo sobreponível a radiografias torácicas realizadas ao longo dos últimos 20 anos. O ecocardiograma transtorácico documentou um aneurisma da artéria pulmonar (AAP), dilatação das câmaras direitas, com pressão sistólica da artéria pulmonar de 52 mmHg e função sistólica do ventrículo direito preservada. A TC torácica confirmou a presença de um aneurisma gigante da artéria pulmonar com 72 mm de diâmetro.
Iniciou-se terapêutica diurética intensiva, com melhoria clínica.
Após otimização e com o doente clinicamente estável, foi realizado cateterismo cardíaco, que revelou hipertensão pulmonar pré-capilar ligeira com uma pressão da artéria pulmonar média de 26 mmHg.
Acreditamos que os dados clínicos e imagiológicos permitiram diagnosticar um aneurisma gigante da artéria pulmonar de altas pressões secundário a hipertensão pulmonar em contexto de DPOC, atualmente estável e com um seguimento de 20 anos sem necessidade de intervenção cirúrgica, que fundamentou a decisão de manter a vigilância médica, sendo a instalação recente de insuficiência cardíaca explicada pela progressão da DPOC.
Este caso poderá alterar a ideia defendida em estudos prévios, que favorecia a escolha de uma abordagem invasiva no tratamento de aneurismas gigantes da artéria pulmonar de altas pressões, dando mais robustez à manutenção de um tratamento médico.
Pulmonary artery aneurysm (PAA) is a rare condition appearing in 1/14000 of autopsies.1 However, there are no prospective studies focusing on PAA, so its precise incidence is unknown.2
Many patients are completely asymptomatic and are diagnosed incidentally in imaging studies.3 A high index of suspicion is thus required for an accurate diagnosis.
The treatment of high-pressure PAA remains controversial but most case reports support a trend for surgical intervention due to the high risk of complications.4
Case reportWe report the case of a 74-year-old Caucasian male followed in our hospital for the past two decades. The patient had a history of chronic obstructive pulmonary disease (COPD), Global Initiative for Chronic Obstructive Lung Disease (GOLD) staging system grade 3, high blood pressure, chronic atrial fibrillation (CAF), chronic right heart failure (HF) classified as New York Heart Association (NYHA) functional class II, and a 60 pack-year history of cigarette smoking.
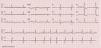
Reviewing the patient's medical record we found a chest radiograph from 1992 (Figure 1, left), on which mediastinal enlargement was already present.
During the first decade of follow-up the patient remained stable under standard medical treatment for COPD and HF, and anticoagulation for CAF.
In 2000 the patient had a gastrointestinal hemorrhage forcing the suspension of anticoagulation. Pharmacological rate control with digoxin was started for treatment of CAF.
In February 2011 a routine transthoracic echocardiogram revealed moderate to severe dilatation of both atria and mild dilatation of both ventricles with normal thickness of the ventricular walls. There was no significant morphological alteration in valve structures. Moderate mitral regurgitation, mild aortic and pulmonary regurgitation, and mild to moderate tricuspid regurgitation were observed. Pulmonary artery systolic pressure (PASP) was 60 mmHg. Biventricular systolic function was preserved.
On the basis of the echocardiographic findings, pulmonary hypertension due to lung disease (GOLD grade 3) was diagnosed.
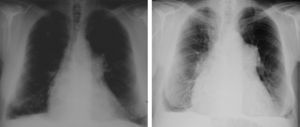
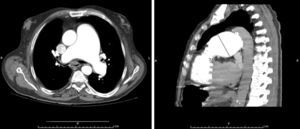
A routine thoracic computed tomography (CT) scan (Figure 2) was also performed in February 2011 and revealed pronounced dilatation of the pulmonary trunk, with a maximum diameter of 72 mm, and dilatation of the main pulmonary arteries, 40 mm in diameter on the right and 33 mm in diameter on the left. There was no evidence of thrombus in the central pulmonary arteries.
The imaging exams led to a diagnosis of a giant pulmonary artery aneurysm (PAA). Closer examination of the recent chest radiographs (Figure 1, right) confirmed the persistence of mediastinal enlargement, without significant increase, which, in comparison with the oldest chest radiograph, showed that the evolution of the PAA had been stable for the previous 20 years.
Despite the patient's stable evolution under medical treatment for the last 10 years, he was admitted to our hospital in March 2012 with severe right HF.
On admission, physical examination revealed blood pressure of 112/63 mmHg, mild peripheral cyanosis, and increased expiratory time, jugular venous distention, and crackles in both lung bases on pulmonary auscultation; cardiac auscultation revealed arrhythmia with a mean ventricular rate of 70 bpm, and severe lower limb edema was observed.
Laboratory tests performed in the emergency department showed leukocyte count of 4100/μl, 59.7% neutrophils, 12.2 g/dl hemoglobin, and C-reactive protein 5.6 mg/l. On biochemical analysis, electrolytes, renal and liver function, cardiac enzymes and coagulation were all within normal limits, but serum brain natriuretic peptide (BNP) level was elevated (577.4 pg/ml).
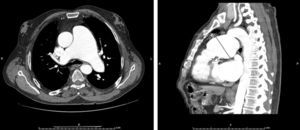
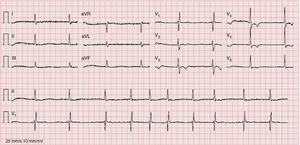
Electrocardiography showed atrial fibrillation with a ventricular rhythm of 63/min, and no significant ST-T abnormalities (Figure 3). The chest radiograph (Figure 1) showed an increased cardiothoracic index, mainly due to enlargement of the right atrium and pulmonary artery.
Thoracic CT angiography revealed a PAA 72 mm in diameter but no signs of thromboembolism or thrombosis in the main pulmonary arteries and branches (Figure 4).
The transthoracic echocardiogram showed a PAA (not quantified because of a poor acoustic window), mild tricuspid regurgitation and PASP of 52 mmHg. The right atrial chamber was dilated and right ventricular systolic function was preserved.
The patient was admitted to the medical ward with a diagnosis of HF and was started on high-dose diuretics, with significant clinical improvement.
A history of major thoracic trauma or significant clinical infection was ruled out, and antinuclear autoantibodies, serology for HIV1 and 2, and the Venereal Disease Research Laboratory and Treponema pallidum hemagglutination tests for syphilis were negative.
After optimization of medical therapy the patient underwent right cardiac catheterization, which revealed mean pulmonary arterial pressure of 26 mmHg, right atrial pressure of 8 mmHg, pulmonary capillary wedge pressure of 12 mmHg, pulmonary vascular resistance of 3.8 Wood units and cardiac index of 2.0 l/min/m2, which is compatible with mild precapillary pulmonary hypertension.
The diagnosis was of a giant PAA with precapillary pulmonary hypertension, possibly related to COPD (GOLD grade 3). Since there is no specific evidence-based treatment for this condition, the patient was discharged on standard HF medication, with the indication for clinical surveillance and specific treatment for COPD. At two-year follow-up he was in a stable condition and the control thoracic CT scan showed no increase in the size of the PAA.
DiscussionIn the literature, several etiologies have been described in the pathogenesis of PAA, including congenital cardiac malformations with intracardiac shunt, vascular abnormalities such as arteritis (e.g., Takayasu disease) and primary pulmonary hypertension, vasculitis (e.g., Behçet's disease), connective tissue disorders (such as Marfan, Ehlers-Danlos and Hughes-Stovin syndromes and systemic lupus erythematosus), tuberous sclerosis, atherosclerosis, hereditary hemorrhagic telangiectasia (Osler-Weber-Rendu disease), vascular trauma, tuberculosis, syphilis, and bacterial, fungal or other infections.5
Since the introduction of antibiotics, non-infectious causes of PAA have become more common,5 with recent studies revealing an association in more than 50% of cases with congenital heart disease.6
PAA is defined by pulmonary artery dilatation of >40 mm,1 with some authors considering that dilatation >50 mm defines a giant aneurysm.7
The clinical manifestations of PAA are diverse and non-specific. Symptoms include chest pain, dyspnea, cough, hemoptysis or palpitations.1,8
Nevertheless, it can be asymptomatic, only found incidentally on a routine imaging study such as a chest radiograph, as in our patient.2,3
Imaging studies such as CT, echocardiography and cardiac catheterization aid in the diagnosis and prediction of complications, however the gold standard for establishing a diagnosis of PAA is pulmonary angiography.10,11
There is no consensus on the management of PAA, as different etiologies lead to different management approaches.12 In fact, since PAA is a rare lesion, there are no clear guidelines on treatment and patients have been managed individually.11
Surgical intervention is generally recommended for symptomatic patients and in those with underlying diseases or complications, left-to-right shunt, pulmonary arterial hypertension and large aneurysm size (≥60 mm diameter).5,13–15 Nevertheless, some authors consider that PAA, even when very large, confer low risk in the presence of low pulmonary pressures, absence of congenital or acquired significant right shunt and no association with collagenopathies.7,15 As these patients have a relatively benign prognosis with an uncomplicated course, some authors, not surprisingly, argue that conservative management is a reasonable strategy.16,17
However, little is known about the natural history of PAA, and whatever treatment is chosen, close follow-up is essential.
The approach to high-pressure PAA is even more controversial. Many authors support an aggressive surgical approach in a presence of severe complications such as airway compression,18 pulmonary artery dissection19 and intravascular thrombosis, with most reports describing an unfavorable evolution, such as low quality of life or even death, with medical treatment only.4,9,20
In the case presented, we describe the longest reported history of an uncomplicated giant high-pressure PAA, with at least 20 years of evolution without significant complications, favoring a conservative approach for such cases.
In our case we suspect that the recent unfavorable evolution of COPD may have contributed to the patient's HF.
According to the literature, intensification of specific pulmonary hypertension treatment improves airway compression. Maintenance of anticoagulation, although controversial, is usually needed due to the risk of PAA thrombosis. Nevertheless this may be need to be suspended in cases of hemoptysis, progressive growth of the PAA or concomitant dissection.20 In our case, although indicated, we decided not to start anticoagulation as we believed that the risk of death due to rupture of the PAA in a patient under anticoagulation was higher than the risk of thrombus formation.
Treatment with conventional vasodilators is not recommended in this case since they may impair gas exchange due to the inhibition of hypoxic pulmonary vasoconstriction. In addition, loss of efficacy is observed after long-term use.
Therefore, as the patient had a stable evolution for more than 20 years and his current clinical condition was being treated medically, we decided to maintain a conservative approach and monitor the other clinical conditions.
ConclusionIn the case presented, the recent onset of HF was explained by precapillary pulmonary hypertension associated with COPD in a patient with a giant high-pressure PAA.
A surgical approach was considered, nevertheless, since our patient has severe lung disease which would have significantly increased the surgical risk, we decided not to follow this approach.
In conclusion, giant high-pressure PAA is a rare condition for which in most cases surgical intervention is recommended, nevertheless, since our patient has had a stable evolution for more than 20 years, contradicting the accepted belief found in the literature, we decided to maintain a conservative approach and monitor the patient's comorbidities closely.
Conflicts of interestThe authors have no conflicts of interest to declare.