Intravascular fracture of catheters, especially guiding catheters, is uncommon. We present an unusual case in which a guide twisted and broke in a tortuous iliac artery during manipulation of the guiding catheter with a 0.014inch wire firmly trapped inside and was retrieved by a larger sheath.
A fratura intravascular de cateteres é pouco frequente, especialmente dos cateteres guia. Reportamos um caso inabitual em que o cateter guia foi torcido e lacerado numa artéria ilíaca durante a sua manipulação, estando o fio guia de 0,014″ no seu interior, e sua ulterior extração através de uma bainha de maior calibre.
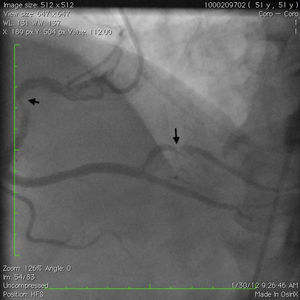
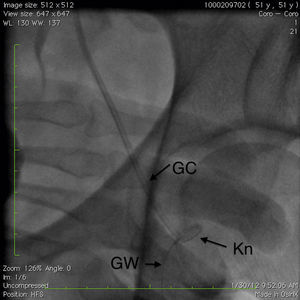
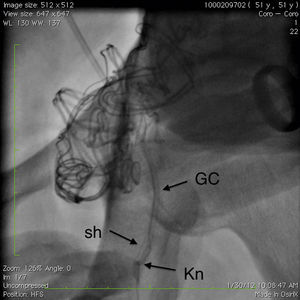
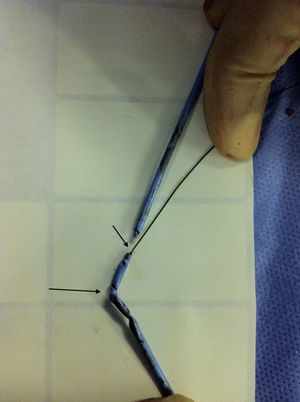
A 51-year-old white man with a history of hypertension and tobacco abuse and a strong family history of premature coronary artery disease was initially admitted to our hospital with worsening chest pain and underwent pharmacological stress testing, which showed distal anterior and apical wall ischemia with preserved left ventricular systolic function. He was referred for coronary angiography, initially performed using a 6F system and right femoral artery access. A 95% lesion of the left anterior descending artery with thrombus was stented without complications. He continued to have chest pain and a second intervention via the left groin was performed four days later on a 80–90% stenosis of the mid right coronary artery (RCA) and 80% stenosis of the mid posterolateral ventricular branch (PLV). During the procedure a 0.035inch wire and 6F sheath were advanced without difficulty. The RCA was engaged with a 6F Amplatz Left (AL) 0.75 guiding catheter (GC) (Cordis, Miami Lakes, FL) for better back-up and a 0.014inch Balance Middle Weight (BMW) wire was advanced to the distal PLV without difficulty. Both lesions were predilated with a 3.0mm×12mm compliant balloon and 3mm×15mm Vision and 4.5mm×18mm Ultra stents were placed in the PLV and mid RCA, respectively, without difficulty and with an optimal result (Figures 1 and 2). During the last cineangiogram, with the BMW wire inside the guide but outside the coronary artery, the AL GC became disengaged. We attempted to reengage the RCA but were unsuccessful, and could not transmit torque through the GC. Fluoroscopy revealed kinking of the distal GC in the external iliac artery. During attempts to straighten the GC by counterclockwise rotation, the guiding catheter fractured into two pieces (Figure 3). The proximal broken piece came out with the sheath and manual pressure was applied. The BMW wire was still firmly attached to the guide. An 8F arterial sheath was then introduced partially up the broken GC over the BMW wire, the introducer sheath was removed, and attempts were made to advance a loop snare next to the kinked GC, with no success, and to advance a 0.035inch J-tip wire next to the GC, also without success. At this time, the other option was to obtain access by the right femoral or brachial/radial artery to try to snare the proximal or distal end of the GC, but there were concerns because of the significant kink potentially traumatizing the exit vessel, especially with a brachial/radial approach. While we were considering advancing a 15-mm Amplatz gooseneck snare (ev3 Inc., Plymouth, MN) over the wire to snare out the distal fragment, it was decided to use the unusually firmly stuck BMW wire as an advantage and to pull back the wire while simultaneously advancing the 8F sheath over the GC. The BMW wire was pulled back rotating a hemostat in a counterclockwise direction and the sheath was advanced while clockwise rotation was applied, which enabled the GC to be straightened; we were able to withdraw the GC inside the sheath (Figure 4), then the sheath was pulled out with the GC inside. Although the distal portion of the fractured GC was out, we were still unable to remove the BMW wire (Figure 5); we therefore cut the guiding catheter proximal to the kink, removed the BMW wire and inserted a J-wire, removed the remaining GC and then reinserted the 8F sheath. The femoral angiogram showed tortuous iliac arteries with a small leak on the medial side of the sheath with no dissection or perforation (Figure 6). A FemoStop was applied at low pressure to stop the leak around the sheath, and the sheath was then removed once active clotting time was <150s. Hemostasis was achieved using manual pressure, and then a FemoStop was applied at low pressure for two more hours, followed by bed rest for a total of eight hours. The patient remained stable and asymptomatic throughout the procedure and overnight, and ambulated without difficulty the next day. The following day, before he was discharged, he went to the bathroom and had to strain, and subsequently developed acute left groin swelling and pain. Examination revealed a palpable hematoma suggestive of pseudoaneurysm. An ultrasound exam confirmed the existence of a 4.2cm×2.9cm pseudoaneurysm which was treated with ultrasound-guided compression. He was subsequently ambulating with no difficulty and was discharged home, and no new problems occurred during follow-up.
Ideally catheter material needs to be sufficiently stiff to maintain structural integrity but also to be sufficiently flexible to minimize discomfort or injury, which makes material selection very important. Catheters are made from polyvinyl chloride (PVC), polyethylene (PE), polyolefin copolymer (POC), or polyethylene terephthalate (PET). GCs are different from diagnostic catheters in that they are stiffer and have a larger lumen size. Their inner liner is a polytetrafluoroethylene coating with lubricating properties, the middle layer is braided stainless steel with stiffening properties, and the outer layer is a polymer (blended nylon).1
Intravascular fracture of angiographic catheters is very rare and few incidents have been reported in the literature.2–4 Kyriakides et al.2 reported reuse of catheters and polymer aging as the reasons for the four fractures they described. All of these six reported fractures were near the bond between the body and the catheter tip2–4; four were diagnostic 7F or 8F Judkins right coronary catheters, one was a 4F diagnostic catheter and one was a 7F pigtail catheter. Schneider et al. reported an 8F diagnostic catheter fracture in the aortic arch and tested the tensile strength of Cordis 7F and USCI catheters. In their study, Cordis catheters have stable tensile strength for up to five years but deterioration was observed after seven years with deep cracks appearing in the lumen wall on microscopic examination.4 Currently, Cordis catheters have three-year expiration dates and our GC had one more year before expiration.
Knotting of a coronary artery catheter at the level of the iliac arteries during coronary angiography is a recognized complication5 but there is no previous reported case of a GC fracture in the proximal shaft in the iliac artery. Knotting usually occurs as a result of excessive torquing mostly of the right coronary catheter when there is a tortuous iliac artery or aorta. When a knot formation is detected, simple maneuvers such as counterclockwise or clockwise rotation (depending on the last rotation applied to the catheter), or advancing the guidewire with gentle traction of the catheter and passing the wire through the knot, may reduce the knotting, but tighter knots may not resolve with such measures.5 In such cases, after obtaining alternative distal access (contralateral femoral or radial), the proximal segment of the catheter above the knot can be snared with a loop snare to secure it and the proximal end of the catheter can be torqued clockwise or counterclockwise until the knot is reduced. This technique is usually effective in resolving these situations.5
Unfortunately, in our patient a slight counterclockwise rotation fractured the GC. Part of the reason for this could be the three knots in the GC visible after it was withdrawn (Figure 5), suggesting multiple kink points in a highly tortuous iliac artery making multiple three-dimensional turns (Figure 6). This was probably also the reason for the BMW wire entrapment.
Once a catheter has fractured, snare-loop wires, nitinol goose-neck snares, or wire balloons3 can be used percutaneously, but surgical intervention may be necessary. In our case, we were able to advance a larger (8F) sheath over the entrapped wire and successfully retrieved the remaining GC by simultaneously pushing the sheath and pulling the GC, applying opposite rotations which helped to straighten the knot and advance the sheath with less chance of vessel trauma. This technique can be used in fractured catheters with trapped wires.
ConclusionWe describe a proximal GC shaft fracture in a patient with a tortuous iliac artery. Using a longer sheath and avoiding excessive manipulation would have prevented this complication in our patient. Once resistance is felt in torquing the catheters it is important to evaluate catheter shape at the level of the iliac arteries or aorta for knot formation before further manipulation. If there is catheter fracture with wire entrapment, advancing a larger sheath over the wire to capture the fractured segment can be considered for retrieval of this segment.
Ethical responsibilitiesProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.