Previous studies on health care and health behaviors in individuals with a family history of coronary heart disease (CHD) have produced contradictory results, and there is still no evidence that these individuals are more aware of their risk and have improved health behaviors and heath care. This study aims to evaluate health care and health behaviors according to family history of CHD.
MethodsIndividuals randomly selected from the general population living in Porto, Portugal, aged ≥18 years (evaluation period: 1999–2003), and without prior history of chronic diseases (n=764), were evaluated by questionnaires on family and personal disease history, health care and health behaviors. A family history of CHD was defined as the occurrence of acute myocardial infarction or sudden death in at least one first-degree relative. Odds ratios and 95% confidence intervals (OR, 95% CI) were calculated using unconditional logistic regression after stratification for age (18–39 vs. ≥40 years) and education (≤6 vs. >6 years schooling).
ResultsAmong men, 20% reported a family history of CHD, approximately the same proportion as in women (19.4%) (p=0.900). The proportion of subjects with a family history of CHD was significantly higher in older (≥40 vs. 18–39 years: 25.0% vs. 12.0%, p<0.001) and less educated individuals (>6 vs. ≤6 years: 27.0% vs. 17.1%, p=0.004). Overall, no significant associations were found between health care and behaviors and CHD family history. Only in younger individuals, after adjustment for education, was a significant positive association found between 1–2 dental visits and CHD family history (OR=2.92; 95% CI: 1.27–6.70). Younger subjects who smoked and consumed alcohol and caffeine also presented a higher probability of having CHD family history, but the associations were not statistically significant.
Discussion and conclusionsIn this population without disease requiring regular medical care, individuals with CHD family history had similar care-seeking patterns and health behaviors to those without. These results suggest a lack of awareness of their increased risk and highlight the importance of developing measures to promote sustained and effective changes in risk factors in individuals with genetic susceptibility to CHD.
Estudos prévios sobre cuidados e comportamentos em saúde em indivíduos com história familiar de doença coronária (DC) revelaram resultados contraditórios, pelo que não está ainda esclarecido se estes indivíduos apresentam uma melhor percepção do seu risco cardiovascular e por esse facto adoptam comportamentos mais saudáveis e apresentam melhores cuidados médicos. Este estudo pretende avaliar comportamentos e cuidados em saúde de acordo com a história familiar de DC.
MétodosOs participantes foram seleccionados aleatoriamente de entre a população residente no Porto com idade ≥ 18 anos e incluídos no estudo se não apresentassem história pessoal de doença crónica (n=764) (período de avaliação: 1999–2003). A informação foi recolhida através de um questionário estruturado sobre a história pessoal e familiar de doença, factores comportamentais e cuidados em saúde. Foi considerada uma história familiar de DC pela ocorrência de enfarte agudo do miocárdio ou morte súbita em pelo menos um familiar em primeiro grau (pais ou irmãos). As associações foram avaliadas por odds ratio e os respectivos intervalos de confiança a 95% (OR, IC 95%), obtidos por regressão logística não condicional após estratificação e ajuste para a idade (18–39 versus ≥ 40 anos) e a escolaridade (≤ 6 versus > 6 anos).
ResultadosA prevalência de história familiar de DC foi de 19,8% (20% nos homens e 19,4% nas mulheres; p=0,900). A proporção de indivíduos com história familiar de DC foi significativamente superior nos indivíduos mais velhos (≥ 40 versus 18–39 anos: 25,0% versus 12,0%, p<0,001) e menos escolarizados (> 6 versus ≤ 6 anos: 27,0% versus 17,1%, p=0,004). No geral não foi encontrada qualquer associação significativa entre os cuidados e comportamentos em saúde e a história familiar de DC. Apenas nos indivíduos mais jovens (18–39 anos) se observou uma associação estatisticamente significativa entre os que consultaram o dentista 1–2 vezes no último ano e a história familiar de DC, mesmo após ajuste para a escolaridade (OR=2,92; IC 95%: 1,27–6,70). Também os indivíduos mais novos com história familiar de DC apresentaram uma maior prevalência de hábitos tabágicos e de consumo de álcool e cafeína, apesar de as diferenças não se mostrarem estatisticamente significativas.
Discussão e conclusõesNesta população de indivíduos sem história prévia de doença que os obrigue a cuidados médicos regulares verificou-se que os indivíduos com história familiar de DC apresentavam comportamentos e cuidados em saúde semelhantes aos indivíduos sem história familiar de DC. Os resultados obtidos sugerem um desconhecimento da relevância da história familiar no desenvolvimento da sua própria doença e do seu risco acrescido. Salientam também a importância do desenvolvimento de medidas que conduzam à mudança efectiva dos factores de risco modificáveis nestes indivíduos com susceptibilidade genética à DC.
The higher risk for coronary heart disease (CHD) in individuals with a family history reflects both inherited genetic susceptibility and the familial occurrence of modifiable risk factors1–3. Jousilahti and colleagues3 showed that major cardiovascular risk factors such as smoking, high serum cholesterol and high blood pressure had similar relative risk estimates for CHD in individuals with and without a family history of CHD, but the effect of the interaction between family history and these major risk factors on occurrence of acute myocardial infarction is additive and sometimes multiplicative.
The perception of family history, and thus individual risk, is particularly important for health promotion4. One might expect that individuals with a family history of CHD, and consequently a higher risk for the disease, would be more aware of healthy behaviors. However, individuals at risk for CHD do not always adopt appropriate health behaviors, due either to the individual's inability to change their habits or to simple ignorance.
Tracing risk factors in first-degree relatives of individuals with CHD, particularly those who have suffered a premature event, should be considered as an approach for CHD prevention5,6. Nevertheless, the small number of studies on health care and health behaviors in individuals with a family history of CHD have produced contradictory results, and there is still no evidence that individuals with a family history of CHD have better health behaviors and heath care awareness7.
The present study aims to determine whether individuals with a family history of CHD sought health care more frequently and had different health behaviors from those without CHD family history.
MethodsStudy participantsAs part of the EPIPorto study, 2485 adults aged over 17 years living in Porto, Portugal, were recruited by random digit dialing. Households were used as the sampling unit and refusals were not replaced. A participation rate of 70% was achieved8.
Out of 2485 participants evaluated at baseline (1999–2003), 74 were excluded due to cognitive impairment (<24 points on the Mini-Mental State Examination9) and eight due to incomplete information. For the analysis, those who reported a previous medical diagnosis of diabetes mellitus and/or hypertension, had suffered a previous acute myocardial infarction or stroke or presented any other disease requiring regular medical care, were also excluded (n=1639).
The final sample included 764 participants, 419 men and 345 women.
Data collectionA structured standard questionnaire was applied by trained interviewers to obtain data on sociodemographic characteristics including gender, age, and educational level, personal and family medical history, and behavioral characteristics, such as physical activity, smoking, and alcohol and dietary intake. Anthropometrics (weight and height) were also measured.
A positive family history of CHD was defined as at least one first-degree relative having had an acute myocardial infarction or sudden death of unknown cause, regardless of age when the event occurred.
Health care characteristics were self-reported and included blood pressure measurement and blood tests, the number of medical and dental visits, and the use of medication and/or vitamin and mineral supplements, during the year before the interview.
Sports practice was recorded and defined as regular practice (at least 30 min/week) of any physical activity, including walking as a leisure activity. Smoking status was also assessed and participants were classified as current smokers (both daily smokers — at least one cigarette a day, and occasional smokers — less than one cigarette a day), and non-smokers (including those who had never smoked at all, and ex-smokers — who had formerly smoked but not for at least 6 months). Dietary intake was estimated by a validated semi-quantitative food frequency questionnaire, covering the previous year10,11. Two categories of alcohol consumption were defined, according to the American Heart Association guidelines12, using cut-points of 15.0 g/ day for women and 30.0 g/day for men, corresponding to approximately one and two glasses of alcoholic beverages, respectively. For caffeine intake, two categories were considered: <90 mg/day and ≥90 mg/day, considering the cut-point as three cups of coffee per day (45 ml of caffeine each). Total energy intake was categorized into tertiles and subjects were classified accordingly. For fiber, a cut-point of 25 g/day was used12.
Body weight was measured using a digital scale and height was measured in the standing position, using a wall stadiometer. Participants were classified as normal weight (BMI <25.0 kg/m2) or overweight (BMI ≥25.0 kg/m2)13.
EthicsThe local ethics committee approved the study protocol. All participants gave written informed consent to participation, and the study was carried out in accordance with the Helsinki Declaration II.
Statistical analysisProportions were compared by the chi-square test or Fisher's exact test, as appropriate. Means between two independent samples were compared by the Student's t test. To estimate associations between health care and health behaviors and family history of CHD, odds ratios and 95% confidence intervals (OR, 95% CI) were calculated using unconditional logistic regression, after stratification by age (18–39 vs. ≥40 years) and education (≤6 vs. >6 years schooling).
SPSS® software (versión 16.0) was used for the statistical analysis.
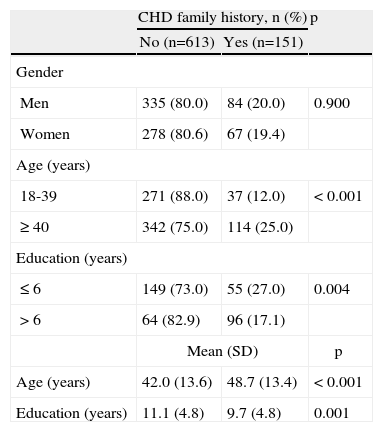
ResultsAmong men, 20% reported a family history of CHD, approximately the same proportion as in women (19.4%) (p=0.900). The proportion of subjects with a family history of CHD was significantly higher in older (≥40 vs. 18–39 years: 25.0% vs. 12.0%, p<0.001) and less educated individuals (>6 vs. ≤6 years: 17.1% vs. 27.0%, p=0.004) (Table 1). The total sample had a mean age of 43.4 years (standard deviation [SD]=13.8) and 10.8 completed years of education (SD=4.8).
Demographic characteristics of participants by family history of coronary heart disease
| CHD family history, n (%) | p | ||
| No (n=613) | Yes (n=151) | ||
| Gender | |||
| Men | 335 (80.0) | 84 (20.0) | 0.900 |
| Women | 278 (80.6) | 67 (19.4) | |
| Age (years) | |||
| 18-39 | 271 (88.0) | 37 (12.0) | <0.001 |
| ≥40 | 342 (75.0) | 114 (25.0) | |
| Education (years) | |||
| ≤6 | 149 (73.0) | 55 (27.0) | 0.004 |
| >6 | 64 (82.9) | 96 (17.1) | |
| Mean (SD) | p | ||
| Age (years) | 42.0 (13.6) | 48.7 (13.4) | <0.001 |
| Education (years) | 11.1 (4.8) | 9.7 (4.8) | 0.001 |
CHD: coronary heart disease.
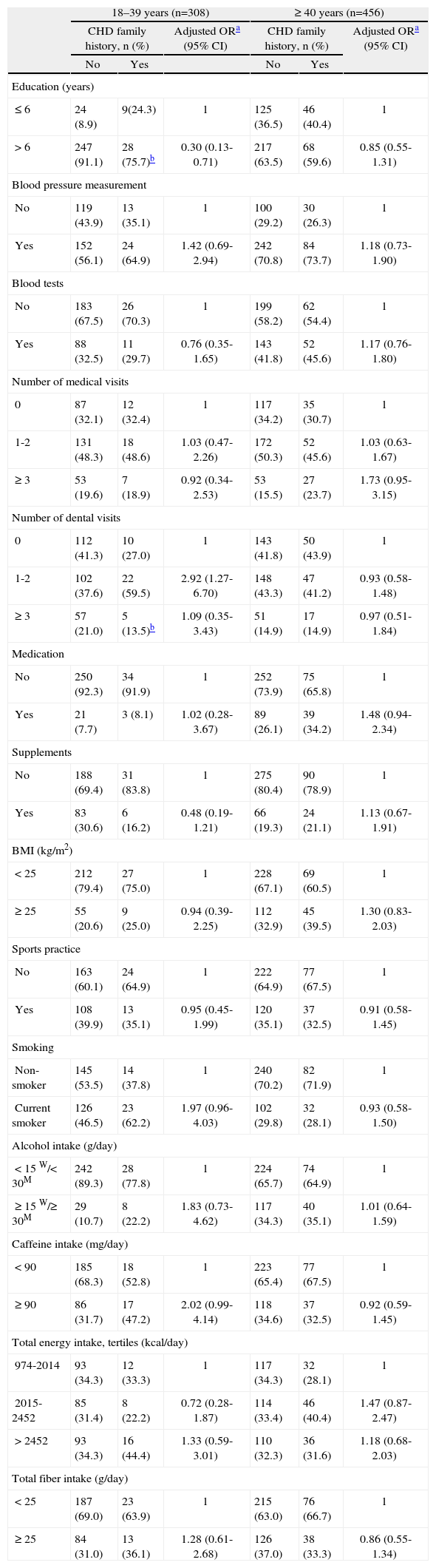
Table 2 shows the prevalence of health care and health behavioral characteristics according to family history of CHD, by age group. In individuals aged between 18 and 39 years, the percentage of those who had 6 or more years education was significantly higher in individuals without a family history of CHD (91.1% vs. 75.7%, p=0.009; OR=0.30; 95% CI: 0.13-0.71). In younger participants, the number of dental appointments in the previous year also varied significantly according to family history of CHD: individuals with a family history of CHD more frequently visited the dentist once or twice a year (59.5% vs. 37.6%). After adjusting for education level, this association remained significant (OR=2.92; 95% CI: 1.27-6.70). For all the other variables, no statically significant associations with CHD family history were found. Nevertheless, younger individuals with a family history of CHD were nearly twice as likely to be current smokers (62.2% vs. 46.5%; p=0.107; OR=1.97; 95% CI: 0.96-4.03) and to drink more alcohol than recommended (22.2% vs. 10.7%; p=0.057; OR=1.83; 95% CI: 0.73-4.62).
Distribution of health care and health behaviors according to family history of coronary heart disease, by age group, and respective associations
| 18–39 years (n=308) | ≥40 years (n=456) | |||||
| CHD family history, n (%) | Adjusted ORa (95% CI) | CHD family history, n (%) | Adjusted ORa (95% CI) | |||
| No | Yes | No | Yes | |||
| Education (years) | ||||||
| ≤6 | 24 (8.9) | 9(24.3) | 1 | 125 (36.5) | 46 (40.4) | 1 |
| >6 | 247 (91.1) | 28 (75.7)b | 0.30 (0.13-0.71) | 217 (63.5) | 68 (59.6) | 0.85 (0.55-1.31) |
| Blood pressure measurement | ||||||
| No | 119 (43.9) | 13 (35.1) | 1 | 100 (29.2) | 30 (26.3) | 1 |
| Yes | 152 (56.1) | 24 (64.9) | 1.42 (0.69-2.94) | 242 (70.8) | 84 (73.7) | 1.18 (0.73-1.90) |
| Blood tests | ||||||
| No | 183 (67.5) | 26 (70.3) | 1 | 199 (58.2) | 62 (54.4) | 1 |
| Yes | 88 (32.5) | 11 (29.7) | 0.76 (0.35-1.65) | 143 (41.8) | 52 (45.6) | 1.17 (0.76-1.80) |
| Number of medical visits | ||||||
| 0 | 87 (32.1) | 12 (32.4) | 1 | 117 (34.2) | 35 (30.7) | 1 |
| 1-2 | 131 (48.3) | 18 (48.6) | 1.03 (0.47-2.26) | 172 (50.3) | 52 (45.6) | 1.03 (0.63-1.67) |
| ≥3 | 53 (19.6) | 7 (18.9) | 0.92 (0.34-2.53) | 53 (15.5) | 27 (23.7) | 1.73 (0.95-3.15) |
| Number of dental visits | ||||||
| 0 | 112 (41.3) | 10 (27.0) | 1 | 143 (41.8) | 50 (43.9) | 1 |
| 1-2 | 102 (37.6) | 22 (59.5) | 2.92 (1.27-6.70) | 148 (43.3) | 47 (41.2) | 0.93 (0.58-1.48) |
| ≥3 | 57 (21.0) | 5 (13.5)b | 1.09 (0.35-3.43) | 51 (14.9) | 17 (14.9) | 0.97 (0.51-1.84) |
| Medication | ||||||
| No | 250 (92.3) | 34 (91.9) | 1 | 252 (73.9) | 75 (65.8) | 1 |
| Yes | 21 (7.7) | 3 (8.1) | 1.02 (0.28-3.67) | 89 (26.1) | 39 (34.2) | 1.48 (0.94-2.34) |
| Supplements | ||||||
| No | 188 (69.4) | 31 (83.8) | 1 | 275 (80.4) | 90 (78.9) | 1 |
| Yes | 83 (30.6) | 6 (16.2) | 0.48 (0.19-1.21) | 66 (19.3) | 24 (21.1) | 1.13 (0.67-1.91) |
| BMI (kg/m2) | ||||||
| <25 | 212 (79.4) | 27 (75.0) | 1 | 228 (67.1) | 69 (60.5) | 1 |
| ≥25 | 55 (20.6) | 9 (25.0) | 0.94 (0.39-2.25) | 112 (32.9) | 45 (39.5) | 1.30 (0.83-2.03) |
| Sports practice | ||||||
| No | 163 (60.1) | 24 (64.9) | 1 | 222 (64.9) | 77 (67.5) | 1 |
| Yes | 108 (39.9) | 13 (35.1) | 0.95 (0.45-1.99) | 120 (35.1) | 37 (32.5) | 0.91 (0.58-1.45) |
| Smoking | ||||||
| Non-smoker | 145 (53.5) | 14 (37.8) | 1 | 240 (70.2) | 82 (71.9) | 1 |
| Current smoker | 126 (46.5) | 23 (62.2) | 1.97 (0.96-4.03) | 102 (29.8) | 32 (28.1) | 0.93 (0.58-1.50) |
| Alcohol intake (g/day) | ||||||
| <15 W/<30M | 242 (89.3) | 28 (77.8) | 1 | 224 (65.7) | 74 (64.9) | 1 |
| ≥15 W/≥30M | 29 (10.7) | 8 (22.2) | 1.83 (0.73-4.62) | 117 (34.3) | 40 (35.1) | 1.01 (0.64-1.59) |
| Caffeine intake (mg/day) | ||||||
| <90 | 185 (68.3) | 18 (52.8) | 1 | 223 (65.4) | 77 (67.5) | 1 |
| ≥90 | 86 (31.7) | 17 (47.2) | 2.02 (0.99-4.14) | 118 (34.6) | 37 (32.5) | 0.92 (0.59-1.45) |
| Total energy intake, tertiles (kcal/day) | ||||||
| 974-2014 | 93 (34.3) | 12 (33.3) | 1 | 117 (34.3) | 32 (28.1) | 1 |
| 2015-2452 | 85 (31.4) | 8 (22.2) | 0.72 (0.28-1.87) | 114 (33.4) | 46 (40.4) | 1.47 (0.87-2.47) |
| >2452 | 93 (34.3) | 16 (44.4) | 1.33 (0.59-3.01) | 110 (32.3) | 36 (31.6) | 1.18 (0.68-2.03) |
| Total fiber intake (g/day) | ||||||
| <25 | 187 (69.0) | 23 (63.9) | 1 | 215 (63.0) | 76 (66.7) | 1 |
| ≥25 | 84 (31.0) | 13 (36.1) | 1.28 (0.61-2.68) | 126 (37.0) | 38 (33.3) | 0.86 (0.55-1.34) |
CHD: coronary heart disease; OR: odds ratio; 95% CI: 95% confidence intervals; BMI: body mass index; W: women; M: men. For some variables, the total does not equal 100% due to missing information.
In older participants, no significant associations between health care and health behavioral characteristics and CHD family history were found.
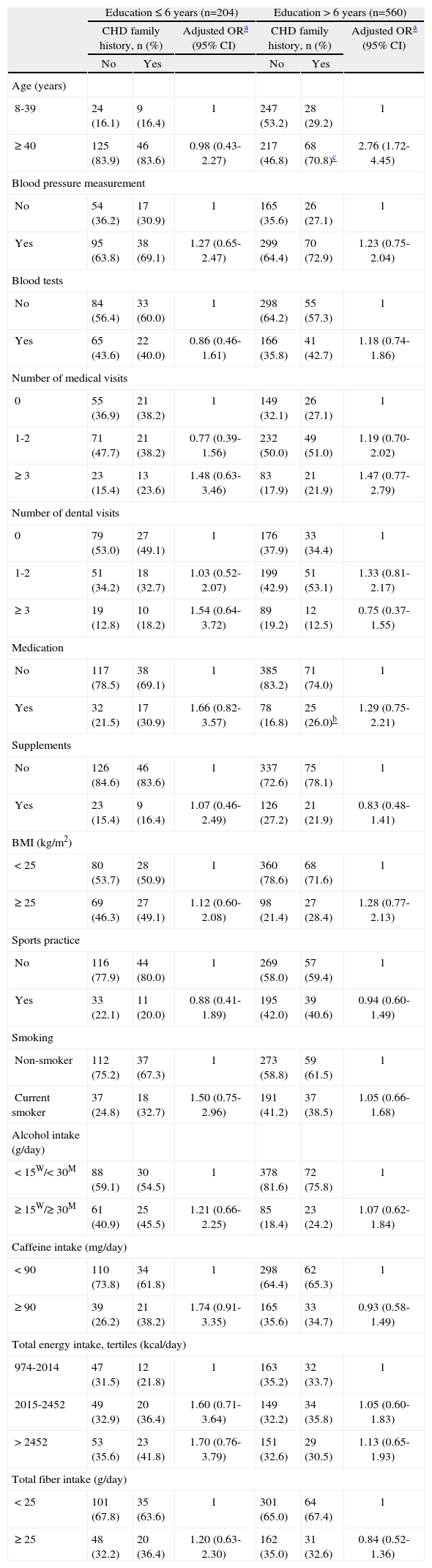
Table 3 shows the prevalence of health care and health behaviors according to family history of CHD, by education level. In more educated individuals (>6 years schooling), the proportion of those aged 40 or over was significantly higher in those with a family history of CHD (70.8% vs. 46.8%; p<0.001). This association was significant only in more educated subjects (OR=2.76; 95% CI: 1.72-4.45). Additionally, in more educated individuals, medication use in the year before interview was significantly higher in those with CHD family history (26.0% vs. 16.8%; p=0.042). After adjusting for age, this association did not remain statistically significant (OR=1.29; 95% IC: 0.75-2.21). No significant associations were found between family history of CHD and the other study variables.
Distribution of health care and health behaviors according to family history of coronary heart disease, by education level, and respective associations
| Education ≤6 years (n=204) | Education >6 years (n=560) | |||||
| CHD family history, n (%) | Adjusted ORa (95% CI) | CHD family history, n (%) | Adjusted ORa (95% CI) | |||
| No | Yes | No | Yes | |||
| Age (years) | ||||||
| 8-39 | 24 (16.1) | 9 (16.4) | 1 | 247 (53.2) | 28 (29.2) | 1 |
| ≥40 | 125 (83.9) | 46 (83.6) | 0.98 (0.43-2.27) | 217 (46.8) | 68 (70.8)c | 2.76 (1.72-4.45) |
| Blood pressure measurement | ||||||
| No | 54 (36.2) | 17 (30.9) | 1 | 165 (35.6) | 26 (27.1) | 1 |
| Yes | 95 (63.8) | 38 (69.1) | 1.27 (0.65-2.47) | 299 (64.4) | 70 (72.9) | 1.23 (0.75-2.04) |
| Blood tests | ||||||
| No | 84 (56.4) | 33 (60.0) | 1 | 298 (64.2) | 55 (57.3) | 1 |
| Yes | 65 (43.6) | 22 (40.0) | 0.86 (0.46-1.61) | 166 (35.8) | 41 (42.7) | 1.18 (0.74-1.86) |
| Number of medical visits | ||||||
| 0 | 55 (36.9) | 21 (38.2) | 1 | 149 (32.1) | 26 (27.1) | 1 |
| 1-2 | 71 (47.7) | 21 (38.2) | 0.77 (0.39-1.56) | 232 (50.0) | 49 (51.0) | 1.19 (0.70-2.02) |
| ≥3 | 23 (15.4) | 13 (23.6) | 1.48 (0.63-3.46) | 83 (17.9) | 21 (21.9) | 1.47 (0.77-2.79) |
| Number of dental visits | ||||||
| 0 | 79 (53.0) | 27 (49.1) | 1 | 176 (37.9) | 33 (34.4) | 1 |
| 1-2 | 51 (34.2) | 18 (32.7) | 1.03 (0.52-2.07) | 199 (42.9) | 51 (53.1) | 1.33 (0.81-2.17) |
| ≥3 | 19 (12.8) | 10 (18.2) | 1.54 (0.64-3.72) | 89 (19.2) | 12 (12.5) | 0.75 (0.37-1.55) |
| Medication | ||||||
| No | 117 (78.5) | 38 (69.1) | 1 | 385 (83.2) | 71 (74.0) | 1 |
| Yes | 32 (21.5) | 17 (30.9) | 1.66 (0.82-3.57) | 78 (16.8) | 25 (26.0)b | 1.29 (0.75-2.21) |
| Supplements | ||||||
| No | 126 (84.6) | 46 (83.6) | 1 | 337 (72.6) | 75 (78.1) | 1 |
| Yes | 23 (15.4) | 9 (16.4) | 1.07 (0.46-2.49) | 126 (27.2) | 21 (21.9) | 0.83 (0.48-1.41) |
| BMI (kg/m2) | ||||||
| <25 | 80 (53.7) | 28 (50.9) | 1 | 360 (78.6) | 68 (71.6) | 1 |
| ≥25 | 69 (46.3) | 27 (49.1) | 1.12 (0.60-2.08) | 98 (21.4) | 27 (28.4) | 1.28 (0.77-2.13) |
| Sports practice | ||||||
| No | 116 (77.9) | 44 (80.0) | 1 | 269 (58.0) | 57 (59.4) | 1 |
| Yes | 33 (22.1) | 11 (20.0) | 0.88 (0.41-1.89) | 195 (42.0) | 39 (40.6) | 0.94 (0.60-1.49) |
| Smoking | ||||||
| Non-smoker | 112 (75.2) | 37 (67.3) | 1 | 273 (58.8) | 59 (61.5) | 1 |
| Current smoker | 37 (24.8) | 18 (32.7) | 1.50 (0.75-2.96) | 191 (41.2) | 37 (38.5) | 1.05 (0.66-1.68) |
| Alcohol intake (g/day) | ||||||
| <15W/<30M | 88 (59.1) | 30 (54.5) | 1 | 378 (81.6) | 72 (75.8) | 1 |
| ≥15W/≥30M | 61 (40.9) | 25 (45.5) | 1.21 (0.66-2.25) | 85 (18.4) | 23 (24.2) | 1.07 (0.62-1.84) |
| Caffeine intake (mg/day) | ||||||
| <90 | 110 (73.8) | 34 (61.8) | 1 | 298 (64.4) | 62 (65.3) | 1 |
| ≥90 | 39 (26.2) | 21 (38.2) | 1.74 (0.91-3.35) | 165 (35.6) | 33 (34.7) | 0.93 (0.58-1.49) |
| Total energy intake, tertiles (kcal/day) | ||||||
| 974-2014 | 47 (31.5) | 12 (21.8) | 1 | 163 (35.2) | 32 (33.7) | 1 |
| 2015-2452 | 49 (32.9) | 20 (36.4) | 1.60 (0.71-3.64) | 149 (32.2) | 34 (35.8) | 1.05 (0.60-1.83) |
| >2452 | 53 (35.6) | 23 (41.8) | 1.70 (0.76-3.79) | 151 (32.6) | 29 (30.5) | 1.13 (0.65-1.93) |
| Total fiber intake (g/day) | ||||||
| <25 | 101 (67.8) | 35 (63.6) | 1 | 301 (65.0) | 64 (67.4) | 1 |
| ≥25 | 48 (32.2) | 20 (36.4) | 1.20 (0.63-2.30) | 162 (35.0) | 31 (32.6) | 0.84 (0.52-1.36) |
CHD: coronary heart disease; OR: odds ratio; 95% CI: 95% confidence intervals; BMI: body mass index; W: women; M: men. For some variables, the total does not equal 100% due to missing information.
The early hypothesis that individuals whose first-degree relatives had had an acute myocardial infarction or sudden death have an increased risk for developing the same disease, and therefore are more aware of their health and present healthier behaviors in order to reduce their risk, was not confirmed. In the present study, there were no significant associations between health care and behavioral characteristics and CHD family history, suggesting that individuals disregard or are unaware of their individual risk.
Nevertheless, it should be noted that in younger individuals the proportion of current smokers was higher among those with a family history of CHD and the difference approached statistical significance. In a population-based study in the UK4, individuals with a family history of CHD smoked less than those without. Another study of Americans without a previous history of CHD14 concluded that the increased risk of disease in men with a family history of CHD predominantly affected smokers. The authors also concluded that 68% of deaths due to family history of CHD could be attributed to the interaction with smoking, and could therefore have been avoided. The West of Scotland Twenty-07 Study4, of 676 individuals in three age cohorts (15, 35 and 55 years), suggested that those with a real perception of their own CHD family history had a lower frequency of smoking than those without, since they recognized the importance of lifestyles in the development of CHD. Recognition of the relation between the perception of CHD family history and changes in behavior, particularly smoking, is of considerable importance for health promotion strategies in groups at higher risk for the disease. On the other hand, the CARDIA study — Coronary Artery Risk Development in (Young) Adults7 — found that, at baseline, the proportion of smokers was similar in individuals with and without a family history of CHD, and that during follow-up, the probability of smoking cessation was very low (5% to 8%) and not related to CHD family history. For other health behaviors (e.g. dietary intake and physical activity), the present study found no significant associations with CHD family history.
A study on health behaviors and attitudes15, including individuals with no known history of CHD, showed, independently of age, significant associations only between CHD family history and blood cholesterol measurement in the five years before the interview and the use of aspirin to reduce risk. In the CARDIA study7, the authors concluded that after follow-up individuals with a family history of CHD had a less favorable risk profile than individuals without CHD family history, contrasting with the early hypothesis that individuals who had had a relative with CHD are active in reducing their modifiable risk.
Overall, health care and health behaviors did not differ significantly between individuals with and without a family history of CHD, and so it could be suggested that there is a lack of perception of individual risk by those with a family history. In the present study, there is no information on behavioral counseling by physicians or other health professionals; it could thus be hypothesized that individuals with CHD family history might not have received health behavior recommendations or information on their risk for developing the disease, since physicians do not always gather information on their patient's family history and lifestyles16,17.
Moreover, if individuals with CHD family history were a target group for effective interventions, the results of the present study might have been different. As awareness of genetics becomes more widespread18, having some knowledge of heredity can influence attitudes and behaviors. However, this knowledge may have an adverse effect, as the 'geneticization' of society could increase skepticism about the capacity of behavioral change to improve health, and result in reluctance to accept health promotion campaigns.
Study limitations and strengthsIn the present study, the exclusion of participants with any chronic diseases requiring regular health care produced a study sample with younger and more educated individuals, and consequently with a lower prevalence of cardiovascular risk factors. Age and education distributions were significantly different between individuals with and without family history of CHD, and so all the analyses in this study were stratified by these two variables and further adjusted. It could be argued that this stratification, along with the relatively small number of individuals with CHD family history, may have reduced the study's statistical power, but this does not seem to influence the general conclusions given the low magnitude of the risk estimates. However, it is possible that greater statistical power might help to show differences between the groups with and without CHD family history in younger individuals, regarding smoking and alcohol and caffeine intake.
The inclusion only of individuals without chronic diseases has the advantage of minimizing any confounding effects that might influence care-seeking and the improvement of behaviors. Selection of participants within a populationbased sample is valuable for the extrapolation of the results to individuals with these characteristics.
A potential limitation of this study could be the inclusion of only those individuals with a home telephone. However, at the time of selection, 97% of Porto households had a telephone number. Additionally, the high participation rate8, as well as the sample characteristics, support the representativeness of the sample.
At first sight, an additional limitation might be the cross-sectional nature of this study, which could limit the establishment of relations and their temporal sequence. However, as the exposure variable is CHD family history, which is not changeable by behavioral modifications, and as the results obtained showed the absence of associations, the reverse causality problem is not relevant. A longitudinal analysis might enhance the ability to examine risk reduction practices over time.
Family history is considered a valid method to determine the occurrence of disease in families19. In most studies, CHD family history is evaluated using a questionnaire, with attendant problems of recall bias in the identification of first-degree relatives affected by CHD. In the present study, though recall bias cannot be excluded, information on family history was collected by trained interviewers using separate questions on the occurrence of acute myocardial infarction and sudden death in the mother, father, brothers and sisters.
Additionally, analysis of family history of premature coronary heart disease (before the age of 55 in men and 60 in women) would help explain behavioral differences between the groups. However, in our sample we have excluded those with disease requiring regular medical care, and for this reason we are dealing with a relatively young sample (mean age 43 years), in which this potential effect would be minimized. Moreover, the population was stratified by age, and multivariate analyses were adjusted for age.
ConclusionsIn a population with no disease requiring regular medical care, individuals with a family history of CHD had no different health care and health behaviors from those without a family history of CHD, which might suggest their lack of awareness of their increased risk.
The results obtained in this study highlight the importance of improving identification of these high-risk groups, and of developing measures conducive to sustained and effective modifications in risk factors in individuals with a genetic susceptibility to CHD.
Conflicts of interestThe authors have no conflicts of interest to declare.
This work received grants from Fundacao para a Ciencia e a Tecnologia, Portugal [POCTI/ESP/42361/200; POCTI / SAU-ESP/61160/2004].