Shorter patient delays are associated with a better prognosis for patients diagnosed with ST-segment elevation myocardial infarction (STEMI). This study aimed to identify predictors of patient delay in the Portuguese population.
MethodsData on 994 patients with suspected STEMI of less than 12 hours’ duration and referred for primary percutaneous coronary intervention (pPCI) and admitted to 18 Portuguese interventional cardiology centers were collected for a one-month period every year from 2011 to 2015. Univariate and multivariate linear regression models were used to identify predictors of patient delay.
ResultsNo significant differences were observed in patient delay over the course of the survey. The multivariate analysis identified five predictors of patient delay: age ≥75 years (exp[beta] 1.28; 95% CI 1.10-1.50; p=0.001), symptom onset between 0:00 and 8:00 a.m. (exp[beta] 1.26; 95% CI 1.10-1.45; p=0.001), and attending a primary care unit before first medical contact (exp[beta] 1.75; 95% CI 1.41-2.16; p<0.001) predicted longer patient delay, while calling the national medical emergency number (112) (exp[beta] 0.84; 95% CI 0.71-1.00; p=0.045) and transport by the emergency medical services to the pPCI facility (exp[beta] 0.71; 95% CI 0.59-0.84; p<0.001) predicted shorter patient delay.
ConclusionsWe identified five factors predicting patient delay, which will help in planning interventions to reduce patient delays and to improve the outcome of patients with STEMI.
Atrasos do doente diminutos estão relacionados com melhores prognósticos no enfarte agudo do miocárdio com supradesnivelamento de ST(STEMI). Este estudo tem como objetivo identificar os fatores preditivos do atraso do doente na população portuguesa.
Métodos e resultadosForam recolhidos dados de 994 doentes com suspeita de STEMI, com menos de 12 horas de evolução, propostos para intervenção coronária percutânea primária, que tivessem sido admitidos num dos 18 centros portugueses com cardiologia de intervenção. Esses dados foram recolhidos durante um mês por ano, entre 2011 e 2015. Modelos de regressão linear univariável e multivariável foram usados para identificar os fatores preditivos do atraso do doente. Não foram observadas diferenças significativas no atraso do doente ao longo do estudo. Na análise multivariável foram identificados cinco fatores preditivos do atraso do doente: idade ≥75 (Exp(beta) 1,28; CI95% 1,10-1,50; p=0,001); desencadear dos sintomas entre as 0:00 e as 8:00 (Exp(beta) 1,26; CI95% 1,10-1,45; p=0,001); primeiro contacto médico efetuado num centro de saúde (Exp(beta) 1,75; CI95% 1,41-2,16; p<0,001) com atrasos do doente mais longos; chamada telefónica para 112-EMS (Exp(beta) 0,84; CI95% 0,71-1,00; p=0,045) e transporte pelo Instituto Nacional de Emergência Médica (EMS) para um centro com P-PCI (Exp(beta) 0,71; CI95% 0,59-0,84; p<0,001) com tempos de atrasos devido ao doente mais curtos.
ConclusõesIdentificámos cinco fatores preditivos do tempo de espera devido ao doente, que irão permitir planear intervenções para reduzir o atraso do doente e melhorar os resultados dos doentes com STEMI.
Cardiovascular disease (CVD) is the leading cause of death and morbidity in Europe, and is estimated to be responsible for more than four million deaths in Europe every year, 49% of deaths among women and 40% among men.1 Treatment for patients with ST-segment elevation myocardial infarction (MI) (STEMI) consists of reperfusion therapy to restore blood flow to the ischemic myocardium. Reperfusion may be performed by primary percutaneous coronary intervention (pPCI) or by fibrinolysis. The current guidelines recommend pPCI as the preferred treatment for STEMI within 12 hours of symptom onset. The greatest benefits of reperfusion therapy in STEMI are achieved when it is performed expeditiously after symptom onset, preferably within the first two or three hours.2–4 Total ischemic time, i.e. time from symptom onset to reperfusion therapy, has prognostic implications.5–7 It is composed of two distinct periods: patient delay (time from symptom onset to first medical contact [FMC]), and system delay (time from FMC to reperfusion therapy).5 Recent evidence suggests that total ischemic time may be a more important clinical variable than door-to-balloon time (time from patient's arrival at a pPCI-capable hospital to reperfusion therapy), which is currently used as a measure of hospital performance regarding STEMI treatment.8,9 Thus, in order to reduce STEMI-related mortality, efforts should be made to improve the other times affecting treatment initiation, in addition to door-to-balloon time. In line with this strategy, the American Heart Association introduced the ‘Mission: Lifeline’ initiative in 2007,10 and the European Association of Percutaneous Cardiovascular Interventions and the European Society of Cardiology established the ‘Stent for Life’ (SFL) initiative in 2009.11 The SFL initiative established three main goals: (1) to treat 70% of STEMI patients by pPCI; (2) to perform 600 pPCI/year/million population; and (3) to ensure that centers with pPCI perform this procedure 24/7. Portugal joined SFL in 201112 and 18 Portuguese interventional cardiology centers able to perform pPCI protocols 24/7 are currently participating in this initiative. One of the aims of the SFL initiative in Portugal is to alert the public to the symptoms of MI and educate them to ask for help by calling the national medical emergency number (112), in order to reduce patient and system delays.
Portugal previously had one of the lowest rates of pPCI in western Europe, but in recent years this procedure has been performed more frequently in Portuguese hospitals, suggesting that participation in the SFL initiative has had a positive impact.13
Reducing patient delay has major implications for the prognosis of patients with STEMI, as it decreases total ischemic time and the occurrence of arrhythmias that can be life-threatening without immediate defibrillation.14,15 This study aims to analyze data on patient delay recorded in the four years after Portugal joined the SFL initiative, in order to identify factors that predict patient delay.
MethodsStudy design and data collectionThe study was based on a national survey covering 18 interventional cardiology centers in mainland Portugal with 24/7 pPCI and participating in the National Registry of Interventional Cardiology and the Portuguese Registry of Acute Coronary Syndromes.16 This survey recorded all catheterized patients with a presumed diagnosis of STEMI between 2011 and 2015, for one month per year. The survey was carried out at five time points: from 9 May to 8 June 2011, immediately after Portugal joined SFL (time zero, T0), and at the same point in 2012 (time one, T1), 2013 (time two, T2), 2014 (time three, T3) and 2015 (time four, T4).
The study population was composed of 1072 patients with suspected STEMI of less than 12 hours’ duration and referred for pPCI and admitted to one of the 18 centers. Patients who received fibrinolytic therapy prior to pPCI, those whose initial presentation of STEMI was in hospital, those admitted in non-mainland regions of Portugal, those with late presentation (more than 12 hours after symptom onset), and those diagnosed with non-ST-elevation MI were excluded from the study, leaving 994 patients for the analysis.
STEMI was defined as the presence of symptoms of myocardial ischemia for more than 30 min and persistent ST elevation (>1 mm in two contiguous leads) or new-onset or previously undocumented complete left bundle branch block. FMC was defined as the time of arrival of medical and/or paramedical staff to attend the patient or the time of arrival at a hospital for pPCI. Patient delay was defined as the delay between symptom onset and FMC. The survey collected various data and different variables were analyzed in this study.
Between 2011 and 2015, the SFL initiative conducted a national campaign on television and radio and in the press called ‘Act Now. Save A Life!’, aimed at reducing patient delay by increasing public knowledge of MI symptoms and encouraging patients to ask for help by calling the national medical emergency number (112).12
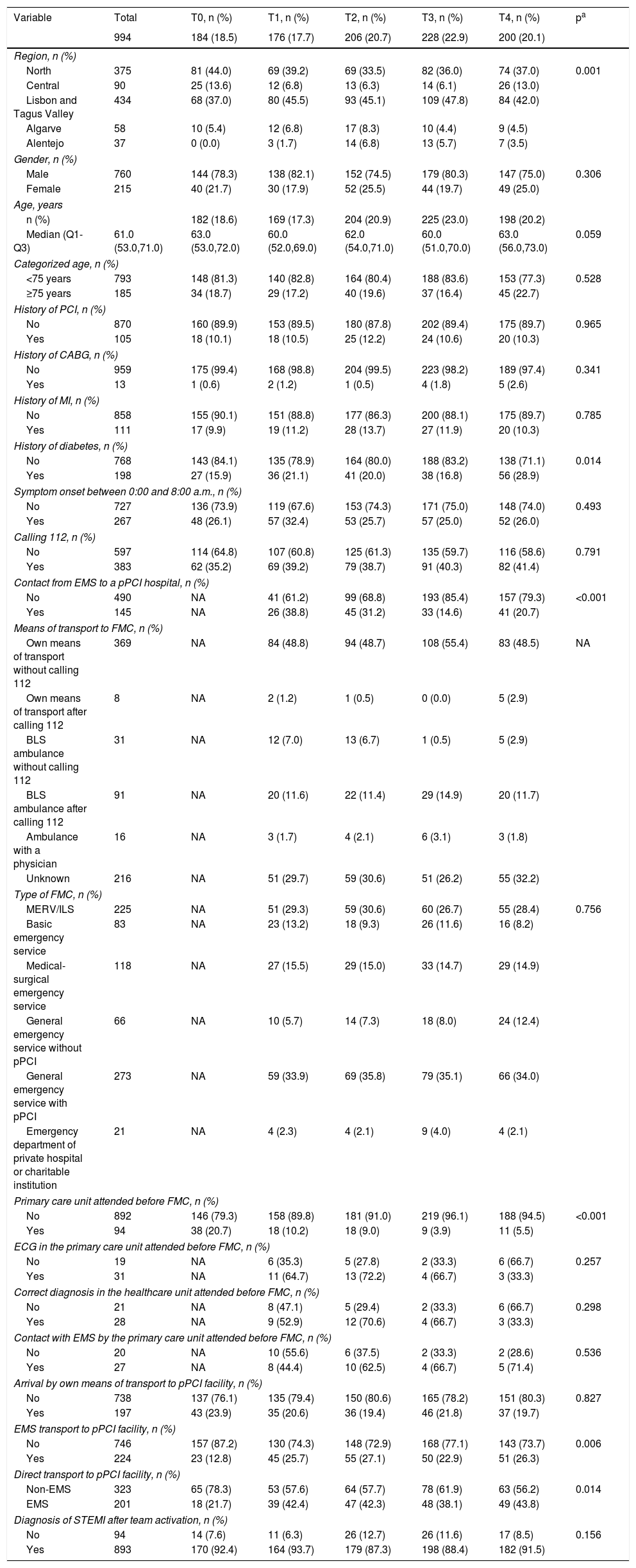
Patient delay and different variables that could influence and/or predict its duration were collected during the survey and are characterized in Table 1. These data were analyzed and compared at all time points (T0-T4) in the four years after Portugal joined the SFL initiative.
Characterization of the population included at the different time points of the survey.
| Variable | Total | T0, n (%) | T1, n (%) | T2, n (%) | T3, n (%) | T4, n (%) | pa |
|---|---|---|---|---|---|---|---|
| 994 | 184 (18.5) | 176 (17.7) | 206 (20.7) | 228 (22.9) | 200 (20.1) | ||
| Region, n (%) | |||||||
| North | 375 | 81 (44.0) | 69 (39.2) | 69 (33.5) | 82 (36.0) | 74 (37.0) | 0.001 |
| Central | 90 | 25 (13.6) | 12 (6.8) | 13 (6.3) | 14 (6.1) | 26 (13.0) | |
| Lisbon and Tagus Valley | 434 | 68 (37.0) | 80 (45.5) | 93 (45.1) | 109 (47.8) | 84 (42.0) | |
| Algarve | 58 | 10 (5.4) | 12 (6.8) | 17 (8.3) | 10 (4.4) | 9 (4.5) | |
| Alentejo | 37 | 0 (0.0) | 3 (1.7) | 14 (6.8) | 13 (5.7) | 7 (3.5) | |
| Gender, n (%) | |||||||
| Male | 760 | 144 (78.3) | 138 (82.1) | 152 (74.5) | 179 (80.3) | 147 (75.0) | 0.306 |
| Female | 215 | 40 (21.7) | 30 (17.9) | 52 (25.5) | 44 (19.7) | 49 (25.0) | |
| Age, years | |||||||
| n (%) | 182 (18.6) | 169 (17.3) | 204 (20.9) | 225 (23.0) | 198 (20.2) | ||
| Median (Q1-Q3) | 61.0 (53.0,71.0) | 63.0 (53.0,72.0) | 60.0 (52.0,69.0) | 62.0 (54.0,71.0) | 60.0 (51.0,70.0) | 63.0 (56.0,73.0) | 0.059 |
| Categorized age, n (%) | |||||||
| <75 years | 793 | 148 (81.3) | 140 (82.8) | 164 (80.4) | 188 (83.6) | 153 (77.3) | 0.528 |
| ≥75 years | 185 | 34 (18.7) | 29 (17.2) | 40 (19.6) | 37 (16.4) | 45 (22.7) | |
| History of PCI, n (%) | |||||||
| No | 870 | 160 (89.9) | 153 (89.5) | 180 (87.8) | 202 (89.4) | 175 (89.7) | 0.965 |
| Yes | 105 | 18 (10.1) | 18 (10.5) | 25 (12.2) | 24 (10.6) | 20 (10.3) | |
| History of CABG, n (%) | |||||||
| No | 959 | 175 (99.4) | 168 (98.8) | 204 (99.5) | 223 (98.2) | 189 (97.4) | 0.341 |
| Yes | 13 | 1 (0.6) | 2 (1.2) | 1 (0.5) | 4 (1.8) | 5 (2.6) | |
| History of MI, n (%) | |||||||
| No | 858 | 155 (90.1) | 151 (88.8) | 177 (86.3) | 200 (88.1) | 175 (89.7) | 0.785 |
| Yes | 111 | 17 (9.9) | 19 (11.2) | 28 (13.7) | 27 (11.9) | 20 (10.3) | |
| History of diabetes, n (%) | |||||||
| No | 768 | 143 (84.1) | 135 (78.9) | 164 (80.0) | 188 (83.2) | 138 (71.1) | 0.014 |
| Yes | 198 | 27 (15.9) | 36 (21.1) | 41 (20.0) | 38 (16.8) | 56 (28.9) | |
| Symptom onset between 0:00 and 8:00 a.m., n (%) | |||||||
| No | 727 | 136 (73.9) | 119 (67.6) | 153 (74.3) | 171 (75.0) | 148 (74.0) | 0.493 |
| Yes | 267 | 48 (26.1) | 57 (32.4) | 53 (25.7) | 57 (25.0) | 52 (26.0) | |
| Calling 112, n (%) | |||||||
| No | 597 | 114 (64.8) | 107 (60.8) | 125 (61.3) | 135 (59.7) | 116 (58.6) | 0.791 |
| Yes | 383 | 62 (35.2) | 69 (39.2) | 79 (38.7) | 91 (40.3) | 82 (41.4) | |
| Contact from EMS to a pPCI hospital, n (%) | |||||||
| No | 490 | NA | 41 (61.2) | 99 (68.8) | 193 (85.4) | 157 (79.3) | <0.001 |
| Yes | 145 | NA | 26 (38.8) | 45 (31.2) | 33 (14.6) | 41 (20.7) | |
| Means of transport to FMC, n (%) | |||||||
| Own means of transport without calling 112 | 369 | NA | 84 (48.8) | 94 (48.7) | 108 (55.4) | 83 (48.5) | NA |
| Own means of transport after calling 112 | 8 | NA | 2 (1.2) | 1 (0.5) | 0 (0.0) | 5 (2.9) | |
| BLS ambulance without calling 112 | 31 | NA | 12 (7.0) | 13 (6.7) | 1 (0.5) | 5 (2.9) | |
| BLS ambulance after calling 112 | 91 | NA | 20 (11.6) | 22 (11.4) | 29 (14.9) | 20 (11.7) | |
| Ambulance with a physician | 16 | NA | 3 (1.7) | 4 (2.1) | 6 (3.1) | 3 (1.8) | |
| Unknown | 216 | NA | 51 (29.7) | 59 (30.6) | 51 (26.2) | 55 (32.2) | |
| Type of FMC, n (%) | |||||||
| MERV/ILS | 225 | NA | 51 (29.3) | 59 (30.6) | 60 (26.7) | 55 (28.4) | 0.756 |
| Basic emergency service | 83 | NA | 23 (13.2) | 18 (9.3) | 26 (11.6) | 16 (8.2) | |
| Medical-surgical emergency service | 118 | NA | 27 (15.5) | 29 (15.0) | 33 (14.7) | 29 (14.9) | |
| General emergency service without pPCI | 66 | NA | 10 (5.7) | 14 (7.3) | 18 (8.0) | 24 (12.4) | |
| General emergency service with pPCI | 273 | NA | 59 (33.9) | 69 (35.8) | 79 (35.1) | 66 (34.0) | |
| Emergency department of private hospital or charitable institution | 21 | NA | 4 (2.3) | 4 (2.1) | 9 (4.0) | 4 (2.1) | |
| Primary care unit attended before FMC, n (%) | |||||||
| No | 892 | 146 (79.3) | 158 (89.8) | 181 (91.0) | 219 (96.1) | 188 (94.5) | <0.001 |
| Yes | 94 | 38 (20.7) | 18 (10.2) | 18 (9.0) | 9 (3.9) | 11 (5.5) | |
| ECG in the primary care unit attended before FMC, n (%) | |||||||
| No | 19 | NA | 6 (35.3) | 5 (27.8) | 2 (33.3) | 6 (66.7) | 0.257 |
| Yes | 31 | NA | 11 (64.7) | 13 (72.2) | 4 (66.7) | 3 (33.3) | |
| Correct diagnosis in the healthcare unit attended before FMC, n (%) | |||||||
| No | 21 | NA | 8 (47.1) | 5 (29.4) | 2 (33.3) | 6 (66.7) | 0.298 |
| Yes | 28 | NA | 9 (52.9) | 12 (70.6) | 4 (66.7) | 3 (33.3) | |
| Contact with EMS by the primary care unit attended before FMC, n (%) | |||||||
| No | 20 | NA | 10 (55.6) | 6 (37.5) | 2 (33.3) | 2 (28.6) | 0.536 |
| Yes | 27 | NA | 8 (44.4) | 10 (62.5) | 4 (66.7) | 5 (71.4) | |
| Arrival by own means of transport to pPCI facility, n (%) | |||||||
| No | 738 | 137 (76.1) | 135 (79.4) | 150 (80.6) | 165 (78.2) | 151 (80.3) | 0.827 |
| Yes | 197 | 43 (23.9) | 35 (20.6) | 36 (19.4) | 46 (21.8) | 37 (19.7) | |
| EMS transport to pPCI facility, n (%) | |||||||
| No | 746 | 157 (87.2) | 130 (74.3) | 148 (72.9) | 168 (77.1) | 143 (73.7) | 0.006 |
| Yes | 224 | 23 (12.8) | 45 (25.7) | 55 (27.1) | 50 (22.9) | 51 (26.3) | |
| Direct transport to pPCI facility, n (%) | |||||||
| Non-EMS | 323 | 65 (78.3) | 53 (57.6) | 64 (57.7) | 78 (61.9) | 63 (56.2) | 0.014 |
| EMS | 201 | 18 (21.7) | 39 (42.4) | 47 (42.3) | 48 (38.1) | 49 (43.8) | |
| Diagnosis of STEMI after team activation, n (%) | |||||||
| No | 94 | 14 (7.6) | 11 (6.3) | 26 (12.7) | 26 (11.6) | 17 (8.5) | 0.156 |
| Yes | 893 | 170 (92.4) | 164 (93.7) | 179 (87.3) | 198 (88.4) | 182 (91.5) | |
For difference between groups.
112: national medical emergency number; BLS: basic life support; CABG: coronary artery bypass grafting; ECG: electrocardiogram; EMS: emergency medical services; FMC: first medical contact; ILS: independent life support; MERV: medical emergency response vehicle; MI: myocardial infarction; NA: not available; pPCI: primary percutaneous coronary intervention; Q1-Q3: 1st quartile - 3rd quartile; SD: standard deviation; STEMI: ST-segment elevation myocardial infarction; T0: time zero, 2011; T1: time one, 2012; T2: time two, 2013; T3: time three, 2014; T4: time four, 2015.
Descriptive statistics were used to summarize data for all variables and for the five time points of the survey. For categorical data, associations between groups were assessed by the chi-square test or Fisher's exact test; for continuous data, differences were assessed by analysis of variance or by the Kruskal-Wallis test for non-normally distributed data. The normality of data was assessed by the Shapiro-Wilk test.
Patient delay was defined as the time from symptom onset to FMC. It was considered a continuous variable and expressed in min.
For analysis of patient delays, as these values were skewed, they were described using medians and interquartile ranges (IQR) and tested using the Mann-Whitney U test or the Kruskal-Wallis test for two or more independent samples, respectively.
Patient delays were log-transformed for subsequent analyses. The effect of each potential predictor of patient delay was assessed by linear regression. The effect of each potential predictor was first tested in a univariate model and then, if it was statistically significant, in a multivariate model to eliminate the effect of potential confounders. Exponential beta coefficients (exp[beta]) and 95% confidence intervals (CI) were reported and correspond to changes in the ratio of the expected geometric means of the original delay. The analysis was conducted at a 5% level of significance. All statistical analyses were performed using R software version 3.1.0.17
ResultsA total of 994 patients who underwent pPCI were included in the survey during the four-year study period. As shown in Table 1, significant differences were observed over the years in the proportion and distribution of patients among the different national regions, the proportion of patients with known diabetes, the occurrence of contact from EMS with a cardiologist, and the proportions of patients who attended a primary care unit before FMC, who had EMS transport to the pPCI facility, and who arrived directly at the pPCI facility.
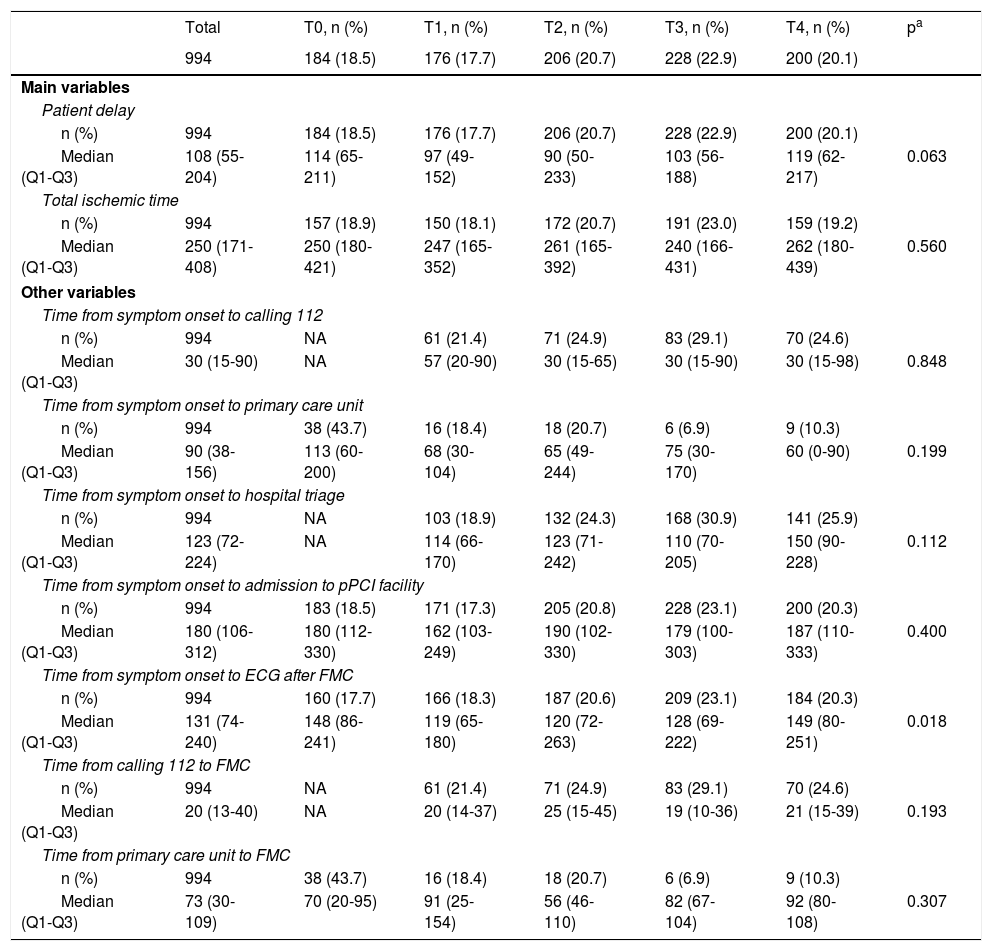
Table 2 presents the evolution of patient delay over the course of the survey, as well as eight other times influencing patient delay. No differences were observed between patient delay before the campaign and four years later (median 114 min in 2011 vs. 119 min in 2015). However, we found a trend for a decrease in patient delay from 2011 to 2013, but this decrease was reversed in 2014 and 2015. We also observed that only the variable ‘time from symptom onset to ECG after FMC’ differed statistically during the survey, decreasing from 2011 to 2014. However, in 2015, similar values were seen to those observed before the SFL campaign.
Characterization of patient delay and other times influencing it over the different time periods of the survey.
| Total | T0, n (%) | T1, n (%) | T2, n (%) | T3, n (%) | T4, n (%) | pa | |
|---|---|---|---|---|---|---|---|
| 994 | 184 (18.5) | 176 (17.7) | 206 (20.7) | 228 (22.9) | 200 (20.1) | ||
| Main variables | |||||||
| Patient delay | |||||||
| n (%) | 994 | 184 (18.5) | 176 (17.7) | 206 (20.7) | 228 (22.9) | 200 (20.1) | |
| Median (Q1-Q3) | 108 (55-204) | 114 (65-211) | 97 (49-152) | 90 (50-233) | 103 (56-188) | 119 (62-217) | 0.063 |
| Total ischemic time | |||||||
| n (%) | 994 | 157 (18.9) | 150 (18.1) | 172 (20.7) | 191 (23.0) | 159 (19.2) | |
| Median (Q1-Q3) | 250 (171-408) | 250 (180-421) | 247 (165-352) | 261 (165-392) | 240 (166-431) | 262 (180-439) | 0.560 |
| Other variables | |||||||
| Time from symptom onset to calling 112 | |||||||
| n (%) | 994 | NA | 61 (21.4) | 71 (24.9) | 83 (29.1) | 70 (24.6) | |
| Median (Q1-Q3) | 30 (15-90) | NA | 57 (20-90) | 30 (15-65) | 30 (15-90) | 30 (15-98) | 0.848 |
| Time from symptom onset to primary care unit | |||||||
| n (%) | 994 | 38 (43.7) | 16 (18.4) | 18 (20.7) | 6 (6.9) | 9 (10.3) | |
| Median (Q1-Q3) | 90 (38-156) | 113 (60-200) | 68 (30-104) | 65 (49-244) | 75 (30-170) | 60 (0-90) | 0.199 |
| Time from symptom onset to hospital triage | |||||||
| n (%) | 994 | NA | 103 (18.9) | 132 (24.3) | 168 (30.9) | 141 (25.9) | |
| Median (Q1-Q3) | 123 (72-224) | NA | 114 (66-170) | 123 (71-242) | 110 (70-205) | 150 (90-228) | 0.112 |
| Time from symptom onset to admission to pPCI facility | |||||||
| n (%) | 994 | 183 (18.5) | 171 (17.3) | 205 (20.8) | 228 (23.1) | 200 (20.3) | |
| Median (Q1-Q3) | 180 (106-312) | 180 (112-330) | 162 (103-249) | 190 (102-330) | 179 (100-303) | 187 (110-333) | 0.400 |
| Time from symptom onset to ECG after FMC | |||||||
| n (%) | 994 | 160 (17.7) | 166 (18.3) | 187 (20.6) | 209 (23.1) | 184 (20.3) | |
| Median (Q1-Q3) | 131 (74-240) | 148 (86-241) | 119 (65-180) | 120 (72-263) | 128 (69-222) | 149 (80-251) | 0.018 |
| Time from calling 112 to FMC | |||||||
| n (%) | 994 | NA | 61 (21.4) | 71 (24.9) | 83 (29.1) | 70 (24.6) | |
| Median (Q1-Q3) | 20 (13-40) | NA | 20 (14-37) | 25 (15-45) | 19 (10-36) | 21 (15-39) | 0.193 |
| Time from primary care unit to FMC | |||||||
| n (%) | 994 | 38 (43.7) | 16 (18.4) | 18 (20.7) | 6 (6.9) | 9 (10.3) | |
| Median (Q1-Q3) | 73 (30-109) | 70 (20-95) | 91 (25-154) | 56 (46-110) | 82 (67-104) | 92 (80-108) | 0.307 |
For difference between groups.
Times are presented in min.
112: national medical emergency number; ECG: electrocardiogram; FMC: first medical contact; NA: not available; Patient delay: time from symptom onset to first medical contact; pPCI: primary percutaneous coronary intervention; Q1-Q3: 1st quartile - 3rd quartile; T0: time zero, 2011; T1: time one, 2012; T2: time two, 2013; T3: time three, 2014; T4: time four, 2015; Total ischemic time: time from symptom onset to reperfusion.
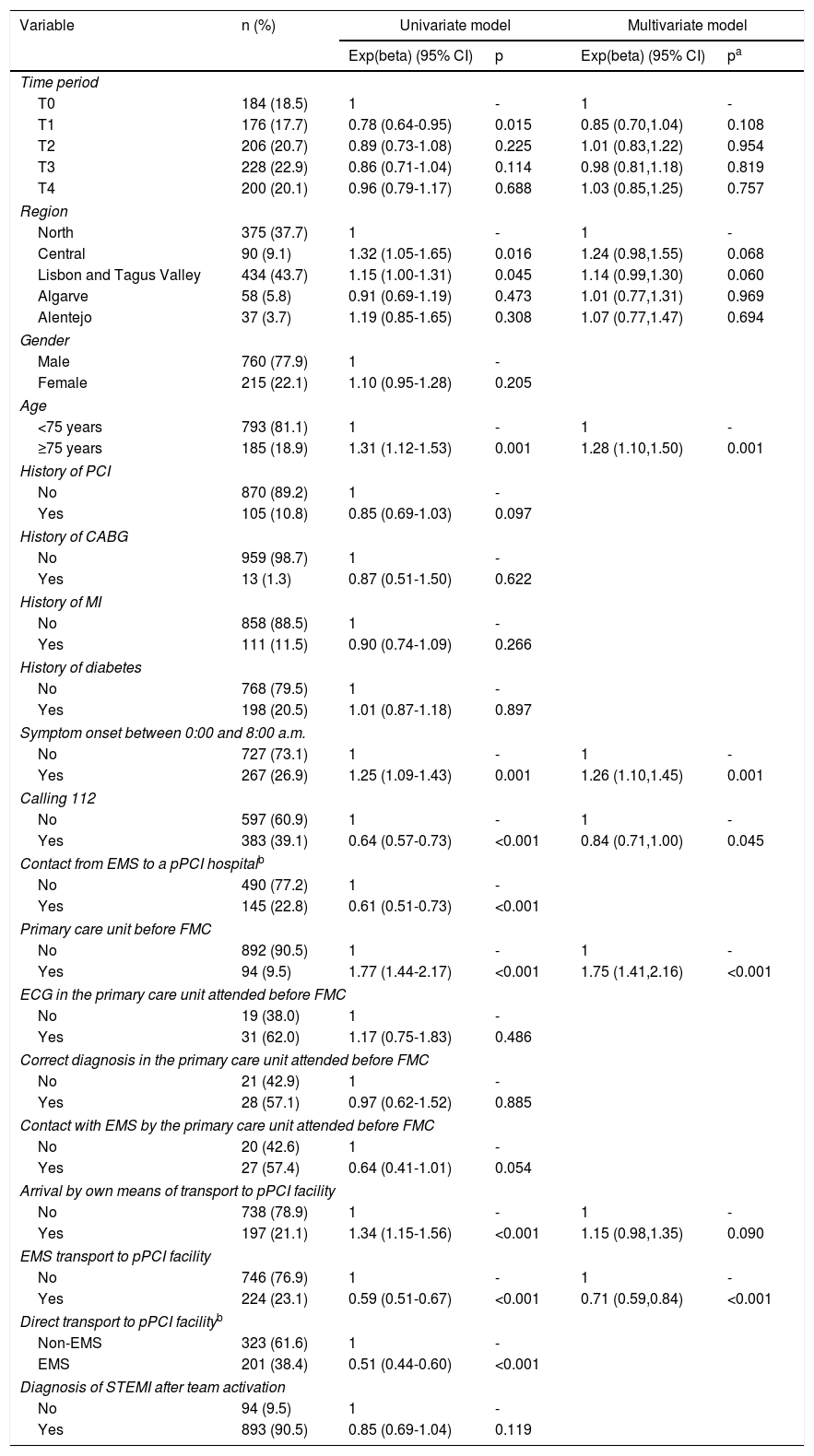
Variables that could influence patient delay were analyzed with regard to their predictive potential, using univariate and multivariate models (Table 3). The univariate linear regression analysis showed that the variables ‘T0’, ‘calling 112’, ‘contact from EMS to a pPCI hospital’, ‘EMS transport to the pPCI facility’ and ‘direct transport to the pPCI facility’ were predictive of shorter patient delay, whereas ‘Central’ and ‘Lisbon and Tagus Valley’ regions, ‘≥75 years old’, ‘symptom onset between 0:00 and 8:00 a.m.’, ‘primary care unit before FMC’, and ‘arrival by own means of transport to a pPCI facility’ were predictive of longer patient delay. However, multivariate linear regression analysis of these variables showed that only the variables ‘≥75 years old’, ‘symptom onset between 0:00 and 8:00 a.m.’ and ‘primary care unit before FMC’ were independent predictive factors of longer patient delay, and only ‘calling 112’ and ‘EMS transport to the pPCI facility’ were independent predictive factors of shorter patient delay.
Univariate and multivariate log-linear regression model for assessment of patient delay predictors.
| Variable | n (%) | Univariate model | Multivariate model | ||
|---|---|---|---|---|---|
| Exp(beta) (95% CI) | p | Exp(beta) (95% CI) | pa | ||
| Time period | |||||
| T0 | 184 (18.5) | 1 | - | 1 | - |
| T1 | 176 (17.7) | 0.78 (0.64-0.95) | 0.015 | 0.85 (0.70,1.04) | 0.108 |
| T2 | 206 (20.7) | 0.89 (0.73-1.08) | 0.225 | 1.01 (0.83,1.22) | 0.954 |
| T3 | 228 (22.9) | 0.86 (0.71-1.04) | 0.114 | 0.98 (0.81,1.18) | 0.819 |
| T4 | 200 (20.1) | 0.96 (0.79-1.17) | 0.688 | 1.03 (0.85,1.25) | 0.757 |
| Region | |||||
| North | 375 (37.7) | 1 | - | 1 | - |
| Central | 90 (9.1) | 1.32 (1.05-1.65) | 0.016 | 1.24 (0.98,1.55) | 0.068 |
| Lisbon and Tagus Valley | 434 (43.7) | 1.15 (1.00-1.31) | 0.045 | 1.14 (0.99,1.30) | 0.060 |
| Algarve | 58 (5.8) | 0.91 (0.69-1.19) | 0.473 | 1.01 (0.77,1.31) | 0.969 |
| Alentejo | 37 (3.7) | 1.19 (0.85-1.65) | 0.308 | 1.07 (0.77,1.47) | 0.694 |
| Gender | |||||
| Male | 760 (77.9) | 1 | - | ||
| Female | 215 (22.1) | 1.10 (0.95-1.28) | 0.205 | ||
| Age | |||||
| <75 years | 793 (81.1) | 1 | - | 1 | - |
| ≥75 years | 185 (18.9) | 1.31 (1.12-1.53) | 0.001 | 1.28 (1.10,1.50) | 0.001 |
| History of PCI | |||||
| No | 870 (89.2) | 1 | - | ||
| Yes | 105 (10.8) | 0.85 (0.69-1.03) | 0.097 | ||
| History of CABG | |||||
| No | 959 (98.7) | 1 | - | ||
| Yes | 13 (1.3) | 0.87 (0.51-1.50) | 0.622 | ||
| History of MI | |||||
| No | 858 (88.5) | 1 | - | ||
| Yes | 111 (11.5) | 0.90 (0.74-1.09) | 0.266 | ||
| History of diabetes | |||||
| No | 768 (79.5) | 1 | - | ||
| Yes | 198 (20.5) | 1.01 (0.87-1.18) | 0.897 | ||
| Symptom onset between 0:00 and 8:00 a.m. | |||||
| No | 727 (73.1) | 1 | - | 1 | - |
| Yes | 267 (26.9) | 1.25 (1.09-1.43) | 0.001 | 1.26 (1.10,1.45) | 0.001 |
| Calling 112 | |||||
| No | 597 (60.9) | 1 | - | 1 | - |
| Yes | 383 (39.1) | 0.64 (0.57-0.73) | <0.001 | 0.84 (0.71,1.00) | 0.045 |
| Contact from EMS to a pPCI hospitalb | |||||
| No | 490 (77.2) | 1 | - | ||
| Yes | 145 (22.8) | 0.61 (0.51-0.73) | <0.001 | ||
| Primary care unit before FMC | |||||
| No | 892 (90.5) | 1 | - | 1 | - |
| Yes | 94 (9.5) | 1.77 (1.44-2.17) | <0.001 | 1.75 (1.41,2.16) | <0.001 |
| ECG in the primary care unit attended before FMC | |||||
| No | 19 (38.0) | 1 | - | ||
| Yes | 31 (62.0) | 1.17 (0.75-1.83) | 0.486 | ||
| Correct diagnosis in the primary care unit attended before FMC | |||||
| No | 21 (42.9) | 1 | - | ||
| Yes | 28 (57.1) | 0.97 (0.62-1.52) | 0.885 | ||
| Contact with EMS by the primary care unit attended before FMC | |||||
| No | 20 (42.6) | 1 | - | ||
| Yes | 27 (57.4) | 0.64 (0.41-1.01) | 0.054 | ||
| Arrival by own means of transport to pPCI facility | |||||
| No | 738 (78.9) | 1 | - | 1 | - |
| Yes | 197 (21.1) | 1.34 (1.15-1.56) | <0.001 | 1.15 (0.98,1.35) | 0.090 |
| EMS transport to pPCI facility | |||||
| No | 746 (76.9) | 1 | - | 1 | - |
| Yes | 224 (23.1) | 0.59 (0.51-0.67) | <0.001 | 0.71 (0.59,0.84) | <0.001 |
| Direct transport to pPCI facilityb | |||||
| Non-EMS | 323 (61.6) | 1 | - | ||
| EMS | 201 (38.4) | 0.51 (0.44-0.60) | <0.001 | ||
| Diagnosis of STEMI after team activation | |||||
| No | 94 (9.5) | 1 | - | ||
| Yes | 893 (90.5) | 0.85 (0.69-1.04) | 0.119 | ||
Variable that revealed multicollinearity or absence of data at T0. Apart from these variables, only significant variables in the univariate model were included in the multivariate model.
112: national medical emergency number; CABG: coronary artery bypass grafting; CI: confidence interval; ECG: electrocardiogram; EMS: emergency medical services; Exp(beta): exponential beta coefficient; FMC: first medical contact; MI: myocardial infarction; PCI: percutaneous coronary intervention; pPCI: primary percutaneous coronary intervention; Q1-Q3: 1st quartile - 3rd quartile; SD: standard deviation; STEMI: ST-segment elevation myocardial infarction; T0: time zero, 2011; T1: time one, 2012; T2: time two, 2013; T3: time three, 2014; T4: time four, 2015.
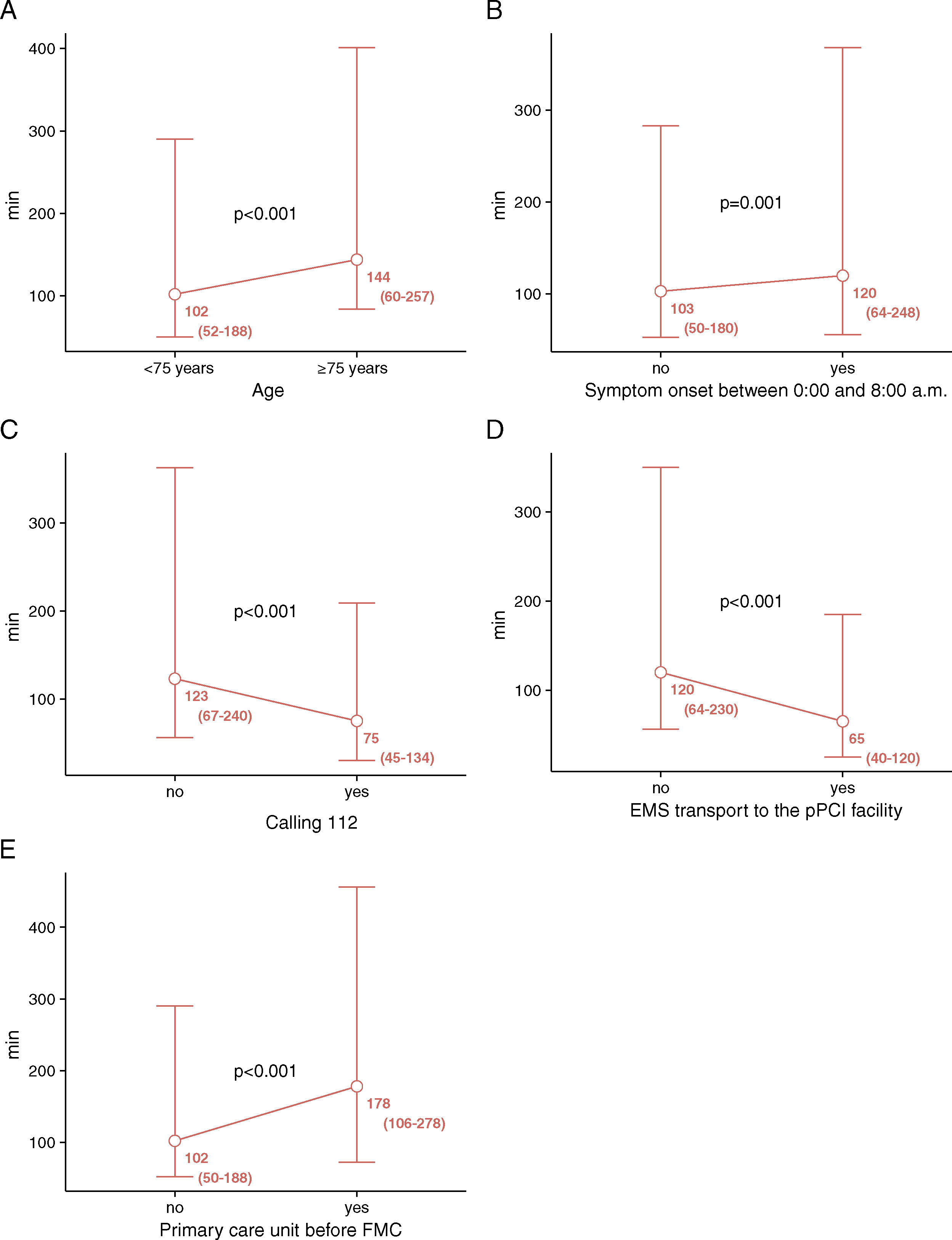
Figure 1 shows the variables that were independent predictors of patient delay. Age <75 years, symptom onset outside the period 0:00 to 8:00 a.m., calling 112, use of EMS transport to the pPCI facility and not attending a primary care unit before FMC were associated with shorter patient delay.
Variables that impact patient delay. (A) Age; (B) symptom onset between 0:00 and 8:00 a.m.; (C) calling 112; (D) EMS transport to the pPCI facility; (E) primary care unit before FMC. Results are presented as median and interquartile range. 112: national medical emergency number; EMS: emergency medical services; FMC: first medical contact; pPCI: primary percutaneous coronary intervention.
To further explore the combined impact of the three modifiable independent predictors of patient delay, the patient delay of patients who called 112 and used EMS transport to the pPCI facility and did not attend a primary care unit before FMC (n=202, 20.3%), was determined. These patients presented a median patient delay of 60 min, which corresponds to a ratio of 0.56, in comparison with the patient delay of the overall study population (108 min).
Discussion and limitationsReducing patient delay has major implications for the prognosis of patients with STEMI. In the last two decades, a marked decrease has been seen in mortality due to ischemic heart disease, but this decrease has been higher in the in-hospital phase than in the prehospital phase.18–21 In addition, recent studies in the USA have shown that reducing door-to-balloon time does not reduce mortality,7,8,22 emphasizing the importance of actions to promote reductions in prehospital patient delay. In this study, we report the effects on patient delay and assessment of predictive factors in the four years after the implementation of the SFL initiative in Portugal. Patient delay did not significantly change over these years, although a non-statistically significant positive trend was observed in the number of patients calling 112. We also identified five factors predicting patient delay.
Reducing patient delay is associated with significant improvement in patients’ prognosis,23–26 so current strategies to improve patient prognosis are focused on reducing prehospital times.5 However, during the last decade, efforts to reduce prehospital time have not been effective22 and most patients do not use the EMS to reach the hospital.27,28 During the ten years before Portugal joined the SFL initiative, only 19% of STEMI patients received pPCI and only 23% called 112.28 To reverse this trend, the SFL initiative launched the national campaign ‘Act Now. Save A Life!’ in December 2011.12 However, our study shows that this campaign did not significantly affect patient delays during the four-year study period (114 min in 2011 vs. 119 min in 2015). The impact of such campaigns on patient delay in other countries has been variable. In Sweden, patient delay decreased from 180 min to 138 min after a one-year media campaign.29 Two nationwide educational campaigns launched in Switzerland were also effective in reducing patient delay,30,31 as was another mass media campaign in Australia.14 On the other hand, similarly to our results, other public campaigns did not lead to significant reductions.32,33 The Rapid Early Action for Coronary Treatment (REACT) Trial was carried out in 20 US cities, of which 10 were assigned to an 18-month public campaign to increase appropriate patient actions for MI symptoms and the other 10 were assigned to reference status.34 No significant differences were found in patient delay between these two groups of cities, but the interventional group saw an increase of 20% in use of the EMS.34 Our data also showed an increase in the number of patients who called 112, although without statistical significance. In 2013, we carried out an unpublished study in collaboration with ISCTE- Instituto Universitário de Lisboa, in which 95% of the 1000 responders knew the EMS number and 91% answered that they would use this number to call an ambulance in the event of MI. However, only 24% of the responders were familiar with the symptoms of MI. Thus, in view of the ineffectiveness of conventional public campaigns in reducing patient delay and increasing awareness of MI symptoms, it is important to identify factors related to prolonged patient delay and to focus media campaigns on these factors.
On the other hand, in our study an increase was observed in the number of patients transported by EMS and transported directly to a pPCI facility. Moreover, EMS transportation was a predictor of shorter patient delay, which is corroborated by other studies.35,36 Nevertheless, EMS transportation is still underused in Portugal by STEMI patients, and efforts should be made to counteract this tendency.
There are various factors that can influence patient delay and the use of the EMS number, including social, cognitive and emotional factors.19 Analysis of our results by a univariate model showed that several variables were predictive of patient delay. Nevertheless, using a multivariate model, most of these variables were not statistically significant, suggesting that they may not be useful as independent predictive factors of patient delay. Thus, we concluded that ‘≥75 years old’, ‘symptom onset between 0:00 and 8:00 a.m.’, and ‘primary care unit before FMC’ were predictive factors of longer patient delay, whereas ‘calling 112’ and ‘EMS transport to the pPCI facility’ was predictive of shorter patient delay. Among these predictors, ‘≥75 years old’ and ‘symptom onset between 0:00 and 8:00 a.m.’ are obviously non-modifiable variables, whereas the other three predictors can be modified by implementing initiatives to increase public awareness. Corroborating the importance of these predictors, patients who called 112 and used EMS transport to the pPCI facility and did not attend a primary care unit before FMC showed an approximately 50% shorter patient delay that the overall study population.
Sociodemographic factors, including age, gender and socioeconomic status, appear to be related to prolonged prehospital delay.19 Our study revealed that patients aged <75 years presented shorter patient delay, whereas no difference was detected with regard to gender. Similarly to these results, other studies also concluded that younger patients presented shorter patient delays.21,37–40 In the light of these results, it is important to conduct public campaigns targeting the elderly population, in order to increase their knowledge of the symptoms of MI. Moreover, as a significant proportion of older patients live alone, it is essential to be alert for symptom onset at night and to stress the importance of asking for help as soon as possible.
In our study, gender was not an independent predictive factor of patient delay, although other studies have reported that female patients present longer patient delays.21,40,41 Patients’ previous clinical condition also did not influence patient delay in this study. In the literature, some studies support our data,42,43 although other reports conclude that a history of heart disease may increase patient delay.37,44
This study showed that ‘symptom onset between 0:00 and 8:00 a.m.’ and ‘attending a primary care unit before FMC’ were independent predictive factors of prolonged patient delay. Other authors also report that symptom onset during off-hours45,46 and interhospital transfer43,47 may have a negative influence on patient delay.
The primary care network also influences how patients ask for help and arrive at a pPCI facility. In this study, the proportion of patients who attended another healthcare unit before FMC significantly decreased throughout the survey, which is notable, as these patients present longer patient delay. This has also been reported by other authors.43 This delay may have a higher impact in countries in which the general practitioner service is the primary route to medical care, such as the UK, where the proportion of patients being attended by a general practitioner is much higher than in this study.48
This work essentially aimed to identify the main predictors of patient delay, not to assess the overall success of the SFL initiative. We did not observe a decrease in patient delay, but this should not be immediately assumed to represent a failure. In addition to the fact that awareness campaigns may have only long-term results, the inclusion of new centers located in regions with few inhabitants and poor access to hospitals has led to the inclusion in the study of patients who will take longer to FMC. On the other hand, the EMS arrive faster for patients in big cities than those in rural areas, impacting patient delay. The SFL initiative will be evaluated later and, in addition to analysis of overall delays, other indicators will also be considered that will enable a thorough assessment of the initiative's success.
The success of a pPCI program should be assessed by the number of patients treated (quantity) and by reductions in total ischemic time (quality). Patient delay is only one of the elements of total ischemic time; system delay is the other. The strategic approach of the SFL task force developed completely different programs for each of these variables, by increasing the public's awareness of patient delays and by promoting educational programs for healthcare professionals targeting system delay. The results obtained for system delay will be the subject of another publication.
Despite our interesting findings, this study also has some limitations. Our data only reflect the results in patients treated with pPCI, so they cannot be generalized to all STEMI patients whether or not they received reperfusion therapy. In addition, data used in this study were only collected during a one-month period per year, and consequently the possible effects of seasonal factors was not addressed. Future studies should be based on a continuous survey, in order to minimize these limitations.
Impact on daily practiceThis study contributes significantly to identifying the independent factors that may predict patient delay in Portuguese STEMI patients. Based on this information, it will be possible to plan more effective media campaigns, focusing on minimizing the impact of these factors and targeting specific groups, such as older patients. These actions will be important to enable reductions in patient delay and more timely treatment of STEMI patients.
FundingThe authors state that they have no funding to declare.
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors gratefully acknowledge all centers that participated in the Stent for Life Initiative Portugal between 2011 and 2015.
Hospital Vila Real (Dr. Henrique Cyrne Carvalho and Dr. Paulino Sousa), Hospital Braga (Dr. João Costa), Hospital S. João (Dr. João Carlos Silva), Hospital Santo António (Dr. Henrique Cyrne Carvalho), Centro Hospitalar Vila Nova de Gaia (Dr. Vasco Gama Fernandes), Hospital de Viseu (Dr. João Pipa), Centro Hospitalar de Coimbra (Dr. Marco Costa and Dr. Vitor Matos), Hospital de Leiria (Dr. João Morais), Hospital Fernando da Fonseca (Dr. Pedro Farto e Abreu), Hospital de Santa Maria (Dr. Pedro Canas da Silva), Hospital Santa Cruz (Dr. Manuel Almeida), Hospital de Santa Marta (Dr. Rui Ferreira), Hospital Curry Cabral (Dr. Luis Mourão), Hospital Pulido Valente (Dr. Pedro Cardoso), Hospital Garcia de Orta (Dr. Hélder Pereira), Hospital Setúbal (Dr. Ricardo Santos); Hospital de Évora (Dr. Lino Patrício and Dr. Renato Fernandes), Hospital de Faro (Dr. Victor Brandão).