Whenever several therapeutic options exist, multidisciplinary decision-making is beneficial for the patient and for society at large. The main obstacles to the establishment of heart teams in Portugal are organizational and logistical. Implementing a heart team approach entails definition of the situations requiring multidisciplinary discussion, creation of clear lines of communication, written protocols and obtaining patient informed consent. The European Society of Cardiology guidelines define the clinical scenarios where intervention of the heart team is recommended.
A decisão médica tomada em equipas multidisciplinares é uma mais-valia indiscutível para o doente e para a sociedade, particularmente quando existem várias opções terapêuticas. A falta de disponibilidade dos intervenientes, problemas logísticos e barreiras interdisciplinares são alguns dos obstáculos à operacionalização do Heart Team em Portugal. A operacionalização passa pela definição das situações que necessitam discussão multidisciplinar, a elaboração de protocolos escritos, a criação de vias de comunicação claras, a consignação das decisões tomadas e a informação fornecida ao doente. As situações, na doença coronária e na doença valvular, que requerem a intervenção do Heart Team estão definidas nas recomendações da Sociedade Europeia de Cardiologia.
Whenever several therapeutic options exist, multidisciplinary decision-making is beneficial for the patient and for society at large, as it enables their risks and benefits to be assessed more accurately in the light of the individual patient's specific clinical characteristics. The most commonly cited example is in oncology, in which radiotherapy, surgery and chemotherapy are complementary treatments that require multidisciplinary discussion. There is evidence that multidisciplinary decision-making in the diagnosis and treatment of cancer promotes improved survival, reduced variation in survival rates between hospitals and better adherence to guidelines.1
Treatment of cardiovascular disease should be no different, since there are clear advantages to multidisciplinary decision-making in certain situations, including heart failure, complex coronary artery disease and severe aortic stenosis in patients with high surgical risk.
Albeit only with level of evidence C, the European Society of Cardiology (ESC) guidelines contain various class I recommendations on the need for therapeutic decisions to be taken by multidisciplinary teams when assessing non-cardiac surgical risk, and when choosing the method of coronary revascularization (percutaneous coronary intervention [PCI] or coronary artery bypass grafting [CABG]) and valve replacement in aortic stenosis (surgical or transcatheter aortic valve implantation [TAVI]).2–4 Following the European example, the 2011 American College of Cardiology Foundation/American Heart Association guidelines5 also contain a class I recommendation that decisions for the treatment of coronary artery disease should be taken by a heart team, a condition of reimbursement by the American federal authorities.6
A heart team consists of at least a clinical cardiologist, an interventional cardiologist and a cardiac surgeon, but can also include specialists in cardiac imaging, neurology, nephrology, pulmonology and anesthesiology, among others.
The rationale behind establishing heart teams in Portugal is that they are better equipped to assess the clinical situation, taking account of the patient's preferences, and to arrive at the best treatment approach through shared decision-making. As mentioned above, this process also improves adherence to guidelines and reduces variability in patient care.7,8
How to establish heart teams?ObstaclesThere are no published studies on the establishment of heart teams in Portugal, but informal analyses indicate that multidisciplinary teams in cardiology are uncommon, unlike in oncology. This leads to lower quality health care, considerable regional variability in treatment and possibly higher costs.
Several obstacles have been suggested, including organizational and logistical problems, interdisciplinary barriers, personal conflicts, failure to recognize the limitations of proposed treatments, and interests other than those of the patient.9–11 The information given to patients differs depending on whether it is supplied by an interventional cardiologist or a surgeon. A recent study in the USA showed that the guidelines for treatment of stable coronary artery disease were not followed in a high percentage of cases, particularly when CABG was indicated, which was performed in only 53%, with 34% undergoing PCI.12 When patients are faced with making a decision, they should be informed of the available options and have the possibility of discussing the advantages and disadvantages of each proposed method and the right to see their wishes reflected in the final decision. However, in practice, cardiovascular patients, unlike cancer patients, are not always adequately informed concerning the various treatment options.13
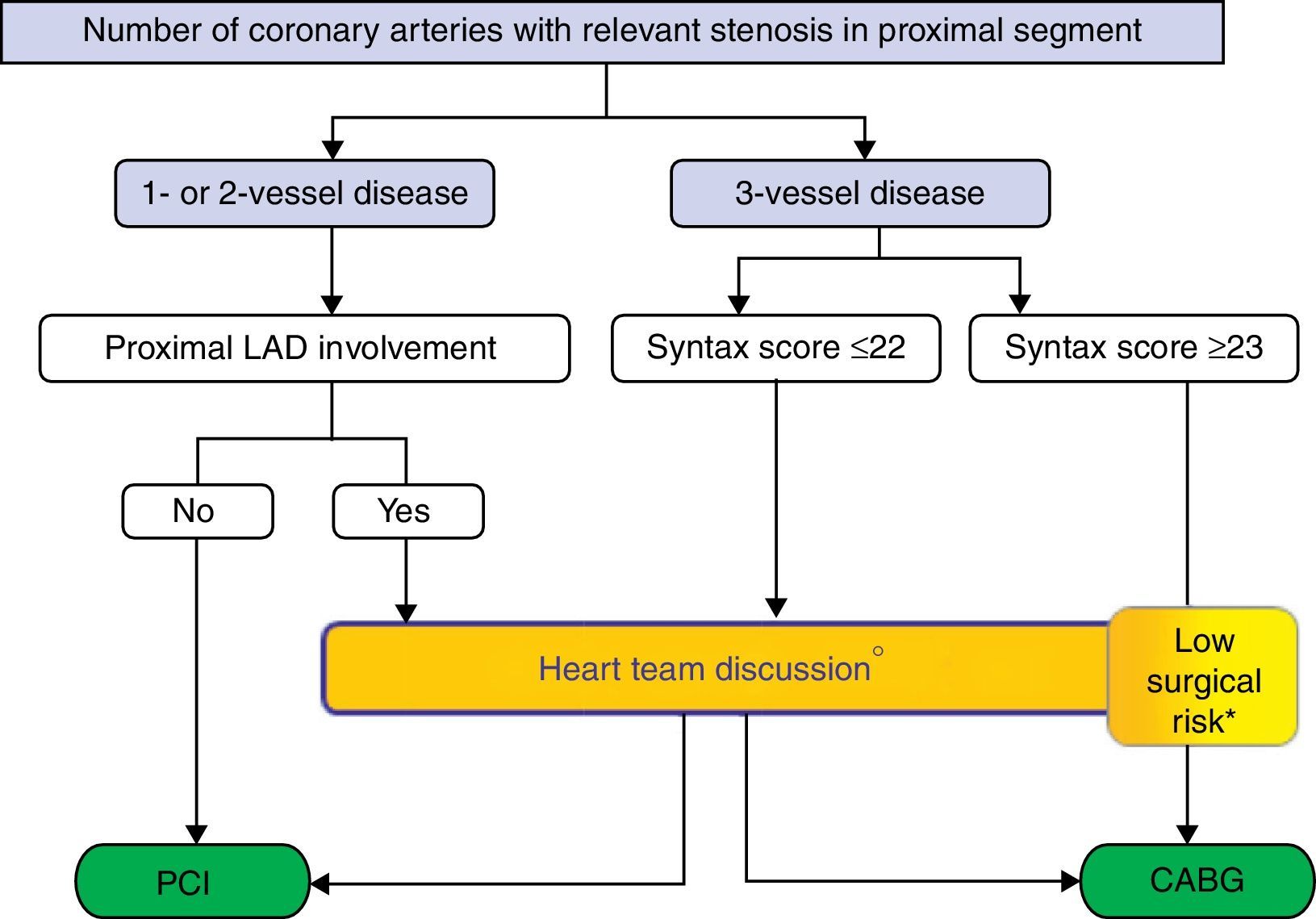
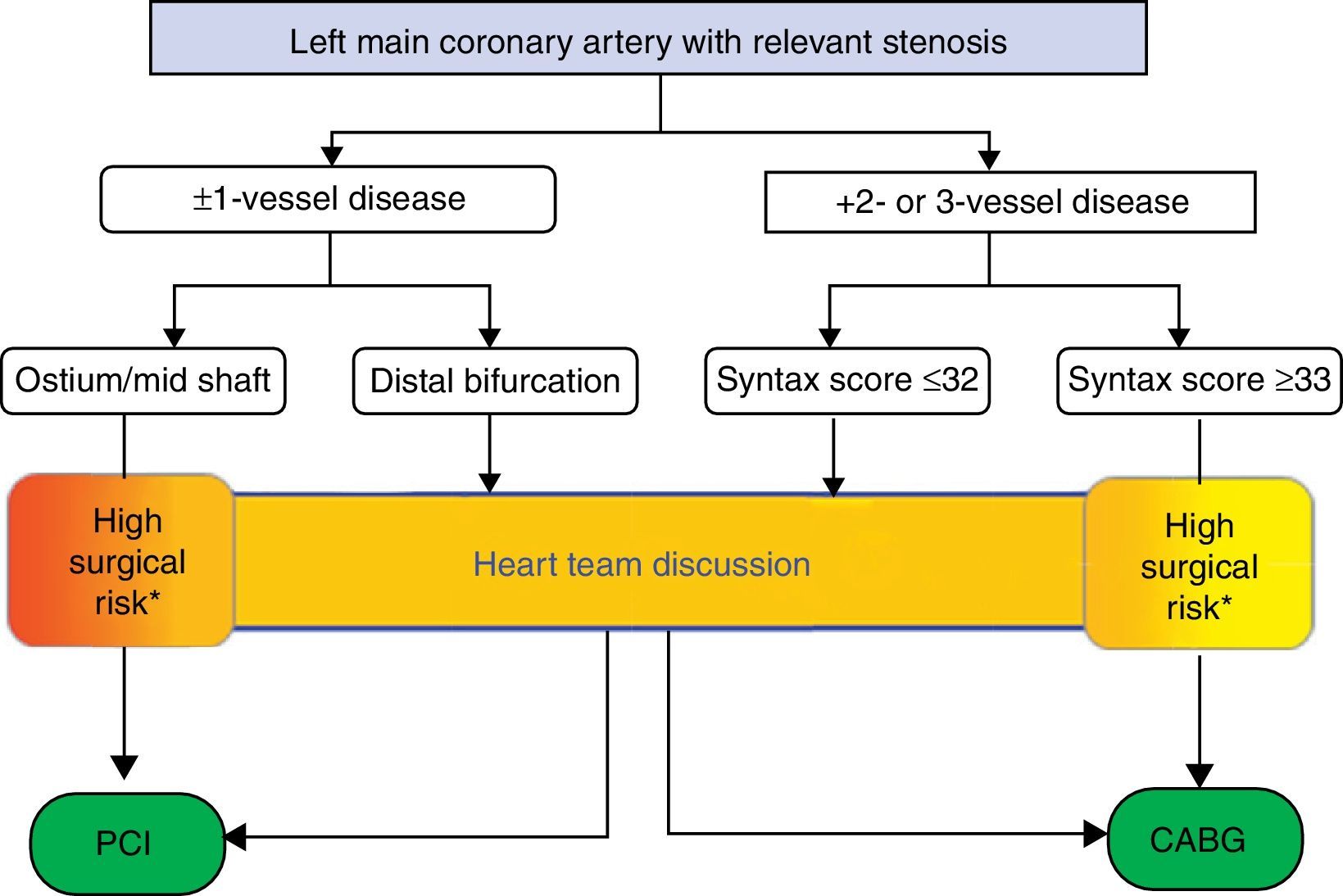
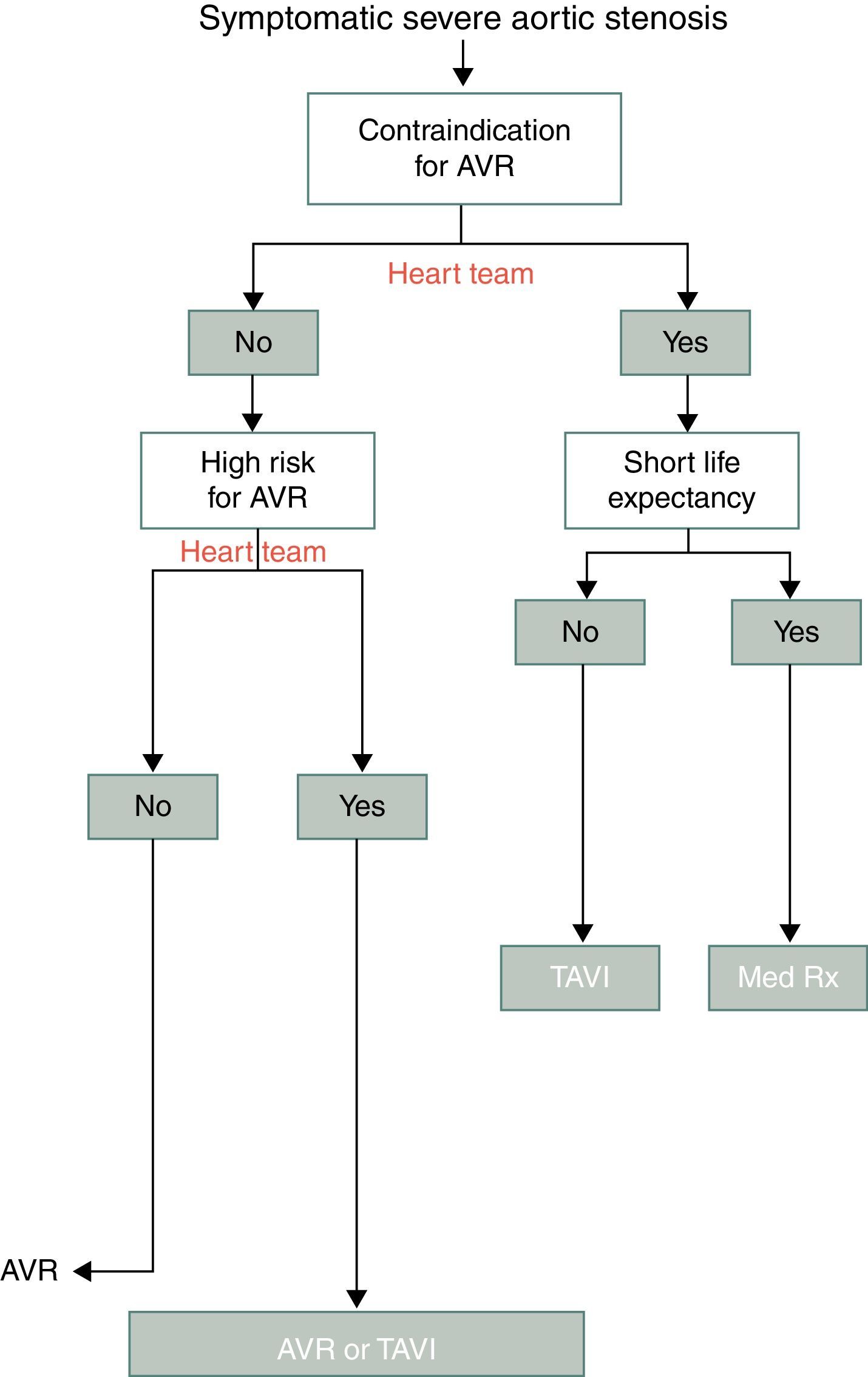
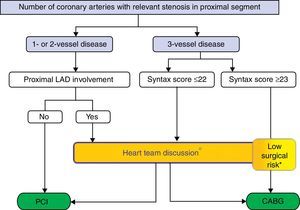
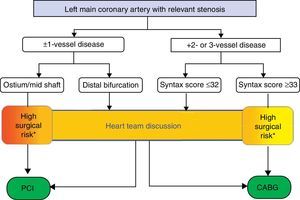
Measures requiredThe first step in establishing heart teams is to prepare written protocols, local or preferably national, that define which situations require multidisciplinary discussion. These protocols should be supported by decision tree algorithms that simplify and clarify the approach to adopt, and can be modified by prior agreement between team members, as established in the heart team protocol (Figures 1 and 2).
Percutaneous coronary intervention or coronary artery bypass grafting in stable coronary artery disease without left main stenosis. * Multidisciplinary discussion preferable, but direct decision-making possible in predefined situations established in the local protocol by the heart team. CABG: coronary artery bypass grafting; LAD: left anterior descending; PCI: percutaneous coronary intervention. Reproduced with permission from the 2013 ESC Guidelines on Management of Stable Angina.
Percutaneous coronary intervention or coronary artery bypass grafting in stable coronary artery disease with left main stenosis. * Multidisciplinary discussion preferable, but direct decision-making possible in predefined situations established in the local protocol by the heart team. CABG: coronary artery bypass grafting; PCI: percutaneous coronary intervention. Reproduced with permission from the 2013 ESC Guidelines on Management of Stable Angina.
Implementing a heart team approach also requires that clear lines of communication be established between the various specialists (who to contact, when and how) and between the specialists and physicians outside the institution, with alternative means when necessary. The heart team can function in an informal manner with discussions taking place remotely, in the catheterization laboratory or at the patient's bedside, or formally, in regular medical and surgical evaluations for complex elective cases. The lack of a cardiac surgery department is not an obstacle to consultation and discussion, since information can be shared electronically (WebEx meetings, image transmission, teleconferencing), as long as these means of communication have been established and tested. The most important elements in a heart team are mutual trust and commitment on the part of all members to work as a group. All members must actively participate, in a climate of interdisciplinary respect and openness, with clear acceptance of all contributions and of both positive and negative reactions. Decision-making should be based on three key points: (1) knowledge transfer; (2) discussion; and (3) reaching agreement on the approach to adopt, in which patient preferences should be prioritized.7
Ideally, each team member's opinion should be recorded in the patient's medical record, together with the final decision on treatment and the patient's informed consent. Institutional databases and national registries (for acute coronary syndrome, PCI and VASP) should include information on heart team interventions and their decisions in the situations described below, as well as the reasons when no discussion takes place. The Portuguese Society of Cardiology is committed to implementing the heart team approach in Portugal and could play an important role in ensuring the results are included in national registries and in promoting studies of outcomes before and after the introduction of heart teams.
Clinical scenarios in which heart teams should be involvedTeam decision-making is recommended by the ESC when choosing between PCI and CABG for coronary revascularization and between surgery or TAVI for valve replacement in aortic stenosis. Other clinical situations, such as severe symptomatic mitral regurgitation despite optimized medical therapy in patients who are unsuitable or at high risk for surgery, should also be discussed by a heart team with a view to possible percutaneous treatment. Multidisciplinary discussion should also take place on the treatment of heart failure, particularly concerning the management of comorbidities and the use of cardiac resynchronization or implantable cardioverter-defibrillator devices.
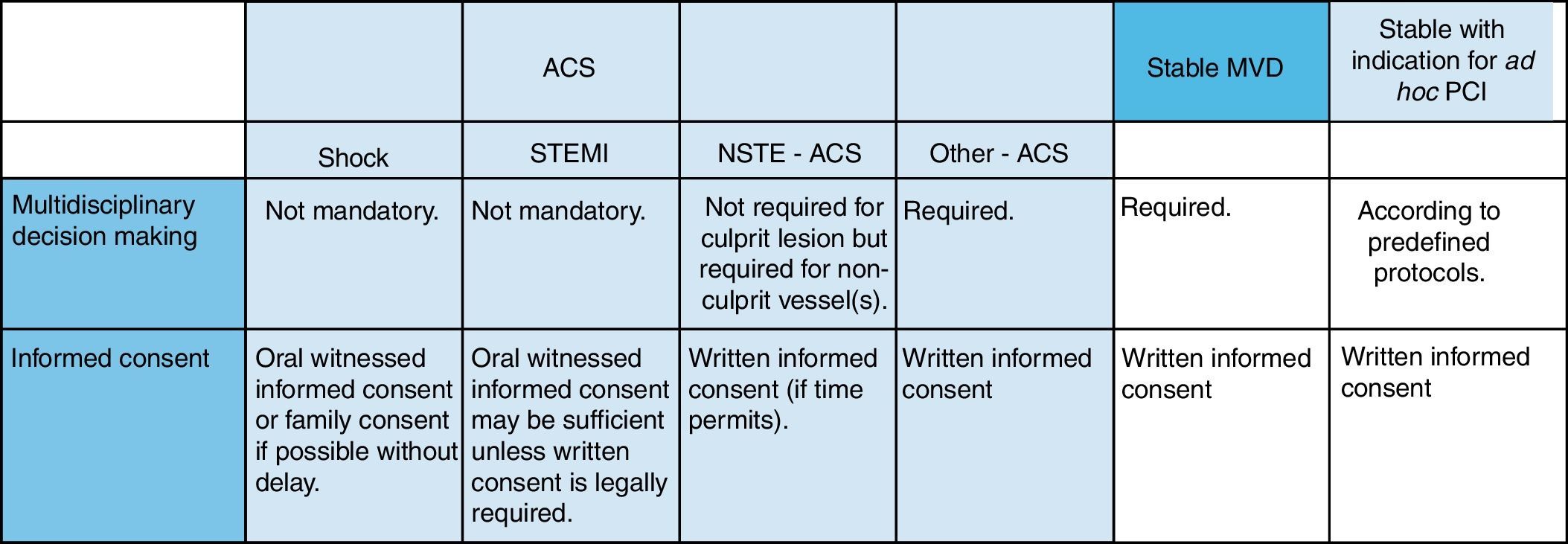
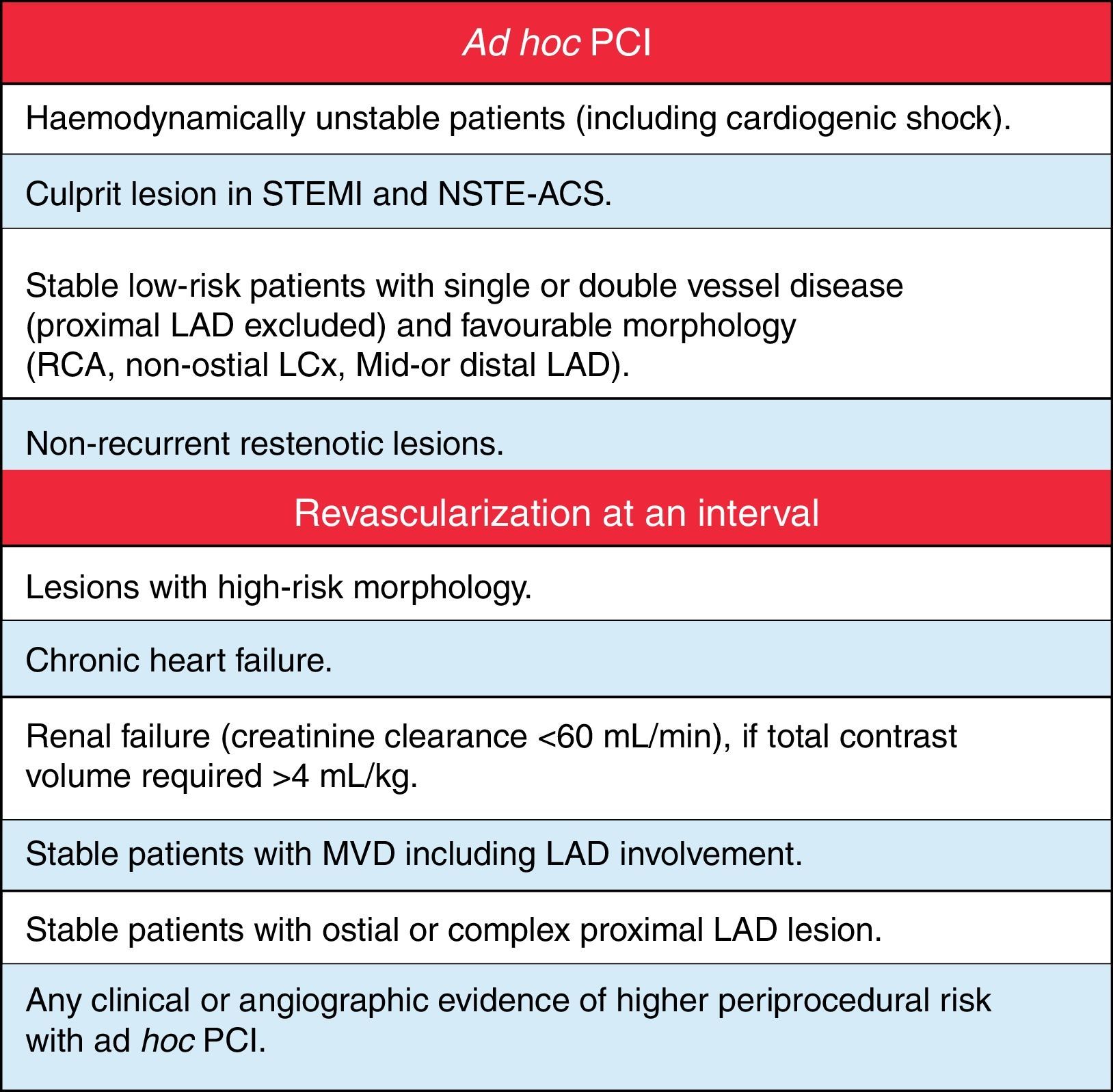
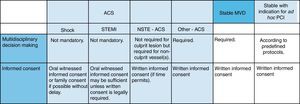
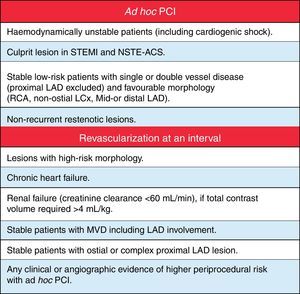
Coronary diseaseIn coronary disease, the decision-making process begins with assessment of the patient's coronary anatomy, history and comorbidities that affect operative risk. The SYNTAX score, validated in the study of the same name, is able to distinguish patients who will benefit from PCI and those who will benefit from CABG.14 Interobserver variability in calculating the score is another reason for interpretation of coronary angiograms and calculation of the SYNTAX score to be carried out by various heart team members. The recently developed SYNTAX score II combines two anatomical variables (the SYNTAX score and presence of unprotected left main coronary artery disease) and six clinical variables (age, gender, creatinine clearance, ejection fraction, chronic obstructive pulmonary disease and peripheral vascular disease).15 Deciding the best treatment approach – medical therapy, PCI or CABG – should be based on multidisciplinary assessment of the anatomical score (SYNTAX score) and operative risk, a process that can be simplified by decision-making algorithms (Figures 1 and 2). Various risk scores have been developed to assess operative risk, the EuroSCORE and STS score being the most widely used. However, these are merely tools to aid decision-making and cannot cover all situations or replace assessment by a heart team and clinical judgment. It is also important in this process to inform the patient of the advantages and disadvantages of each therapeutic option, using such aids as diagrams and answers to frequently asked questions, as well as information on the results and experience of the institution and its physicians. The ESC guidelines on myocardial revascularization include tables defining the clinical and anatomical characteristics of coronary artery disease that require treatment to be delayed after diagnosis to enable multidisciplinary discussion and situations in which it is possible to perform ad-hoc PCI (Figures 3 and 4).2 Not all clinical situations lend themselves to the timeframe required for multidisciplinary consultation, as in ST-elevation myocardial infarction (Figure 3). In other cases, particularly stable angina with left main or three-vessel disease involving the anterior descending artery, an interval is recommended following coronary angiography to enable the patient to be informed and the case discussed by the heart team (Figure 4).
Multidisciplinary decision pathways, patient informed consent, and timing of intervention. ACS: acute coronary syndrome; MVD: multivessel disease; PCI: percutaneous coronary intervention; STEMI: ST-elevation myocardial infarction; NSTE-ACS: non-ST elevation acute coronary syndrome. Reproduced with permission from the 2010 ESC-EACTS Guidelines on Myocardial Revascularization.
Indications for ad hoc percutaneous coronary intervention or revascularization at an interval. LAD: left anterior descending; LCx: left circumflex; MVD: multivessel disease; STEMI: ST-elevation myocardial infarction; NSTE-ACS: non-ST elevation acute coronary syndrome; PCI: percutaneous coronary intervention; RCA: right coronary artery. Reproduced with permission from the 2010 ESC-EACTS Guidelines on Myocardial Revascularization.
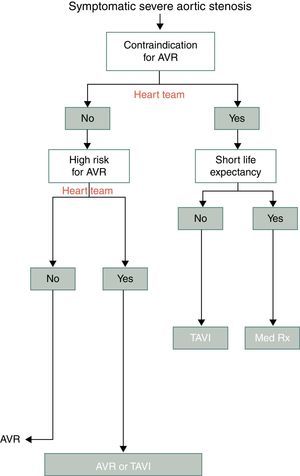
Aortic valve replacement is a class IA recommendation for symptomatic severe aortic stenosis in the 2012 ESC guidelines. Surgical valve replacement should be considered except in patients with contraindications to surgery or high surgical risk; in such cases, TAVI should be discussed. The suggested algorithm indicates that the decision should be taken by a heart team (Figure 5).3
TAVI should be performed only in hospitals with on-site cardiac surgery. The heart team should assess comorbidities, surgical risk, the technical feasibility of TAVI and the patient's life expectancy, as well as identifying cases in which the procedure is likely to improve quality of life. TAVI may be indicated in patients who are unsuitable for surgery due to severe comorbidities or for technical reasons. In patients with high surgical risk but who are operable, the decision between surgical valve replacement and TAVI should be on a case-by-case basis, taking account of the advantages and disadvantages of each method. The decision should be based on clinical assessment by the heart team aided by risk scores (EuroSCORE and STS score), bearing in mind that these scores have significant limitations as they do not include important risk factors such as neurocognitive dysfunction, decreased mobility and frailty, and should not be used in isolation.
ChecklistEvery institution involved in the medical and surgical treatment of patients with coronary artery or valve disease should have a checklist that includes the following:
- (1)
Situations in which the heart team should be consulted;
- (2)
Reasons for not consulting the heart team;
- (3)
Reasons for recommending a particular approach: medical therapy, percutaneous treatment or surgery;
- (4)
Decision of the heart team;
- (5)
Informed consent signed by the patient and members of the heart team.
Attached to this document there should be an information sheet for the patient, prepared by the heart team, describing the medical, percutaneous and surgical options in plain language, including the advantages and disadvantages of each in terms of physical discomfort, functional limitations, potential complications, possible need for reintervention and long-term outcomes.
ConclusionHeart teams bring several benefits for patients and for society at large: better adherence to guidelines, less risk of inappropriate indications, more comprehensive and balanced information, reduced variability in patient care, better overall understanding of patients’ values and preferences, and less risk of malpractice.
Establishing heart teams will require the commitment and concerted efforts of physicians who are aware of the potential benefits and are determined to overcome existing obstacles. However, the support of medical societies, producing guidelines and providing a registry platform, together with encouragement from health authorities, are all factors that can facilitate this process. Hopefully, in the not too distant future, cardiology and cardiothoracic surgery societies will collaborate more closely, coordinating educational initiatives, disease and intervention registries, outcome analysis and certification. Interdisciplinary cooperation and shared decision-making will play an increasingly important role in modern societies faced with the need to optimize health care.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Sousa Uva M, Leite Moreira A, Gavina C, et al. Operacionalização do Heart Team em Portugal. Rev Port Cardiol. 2014;33:45–50.