Lichen planus (LP) is a mucocutaneous inflammatory disease. Inflammation plays a major role in the progression of atherosclerosis. Epicardial fat tissue (EFT) has been shown to produce and secrete various proatherogenic and proinflammatory hormones and cytokines. The aim of this study was to assess EFT in patients with lichen planus.
MethodsFifty-four patients with LP and 50 controls were enrolled in the study. LP was diagnosed according to the World Health Organization criteria. EFT was measured on the free wall of the right ventricle in parasternal long-axis view, as previously described and validated.
ResultsThere were positive correlations between EFT thickness and platelet/lymphocyte ratio, neutrophil/lymphocyte ratio, duration of LP, and high-sensitivity C-reactive protein (hsCRP) (p<0.001, p<0.001, p=0.002 and p<0.001, respectively). In multivariate analysis, after adjustments for relevant confounders, LDL cholesterol, hsCRP, platelet/lymphocyte ratio and duration of LP were independent predictors of EFT thickness in patients with LP (β=0.231, p=0.014; β=0.205, p=0.037; β=0.361, p=0.001 and β=0.133, p=0.047, respectively).
ConclusionEFT is increased in patients with LP compared to control subjects. Duration of LP is correlated with EFT, and duration of LP is also an independent predictor of increased EFT, which is a predictor of subclinical atherosclerosis.
O líquen plano (LP) é uma doença inflamatória mucocutânea. A inflamação tem um papel importante na progressão da aterosclerose. Demonstrou-se que o tecido adiposo epicárdico (TAE) produz e segrega várias hormonas e citocinas pró-aterogénicas e pró-inflamatórias. O objetivo deste estudo foi a avaliação do TAE em pacientes com LP.
MétodosCinquenta e quatro pacientes com LP e 50 controlos foram inscritos no estudo. O LP foi diagnosticado de acordo com os critérios da Organização Mundial de Saúde. O TAE foi medido na parede livre do ventrículo direito, do ponto de vista do eixo longo para-esternal, conforme descrito e validado anteriormente.
ResultadosVerificaram-se correlações positivas entre a espessura da gordura epicárdica e a relação linfócitos-plaquetas, a relação neutrófilos-linfócitos, a longevidade do LP, e o hsCRP (p < 0,001, p < 0,001, p = 0,002 e p < 0,001, respetivamente). Após análises multivariadas e ajustamentos para confundidores relevantes (colesterol LDL, hsCRP, relação plaquetas-linfócitos e longevidade do LP), foram confirmados como preditores independentes da espessura da gordura epicárdica em pacientes com LP (β = 0,231, p = 0,014; β = 0,205, p = 0,037; β = 0,361, p = 0,001 e β = 0,133, p = 0,047, respetivamente).
ConclusãoO TAE está aumentado em pacientes com LP em comparação com o grupo de controlo. A longevidade do LP está correlacionada com o TAE, e a sua longevidade é uma variável independente de previsão do TAE aumentado, que por sua vez é uma variável de previsão da aterosclerose subclínica.
Lichen planus (LP) is a mucocutaneous inflammatory disease that affects 0.5-1% of the population. Its etiology remains unknown; it may be caused by a cell-mediated immunological response in which auto-reactive T4 and T8 lymphocytes are the cytotoxic effector cells which cause degeneration and destruction of keratinocytes.1,2 LP is associated with lipid disorders, and the inflammatory process may lead to lipid metabolism disturbances such as increased serum triglycerides (TG) and decreased high-density lipoprotein (HDL).3,4 Inflammation is the predominant mechanical contributor to atherothrombosis and measurement of inflammatory markers could have a role in the management of risk stratification beyond the scope of current global risk assessment.5,6 It has been hypothesized that the association between LP and cardiovascular risk is due to chronic systemic inflammation.3,6
Epicardial fat tissue (EFT) is the adipose tissue located between the myocardial epicardium and visceral epicardium of the heart. EFT has been shown to produce and secrete various proatherogenic and proinflammatory hormones and cytokines, including tumor necrosis factor (TNF)-α, interleukin (IL)-6, adipocytokines and leptin.7–9 Previous studies have demonstrated an association between EFT and insulin resistance, diabetes mellitus, increased cardiometabolic risk, inflammatory markers and coronary artery disease (CAD).10–15
Like psoriasis, LP is a chronic inflammatory disease. Bacaksız et al. indicate that EFT is significantly increased in patients with psoriasis vulgaris.16 The aim of this study was to assess EFT in patients with lichen planus.
MethodsPatient selectionA total of 54 patients with LP and 50 age-matched controls were enrolled in the study from January 2014 to January 2015. The inclusion criteria for the study group were as follows: men or women aged more than 18 years with LP confirmed according to the clinical and histopathologic criteria established by the World Health Organization. LP was assessed clinically in a standardized dermatological examination by trained and experienced physicians, some of them dermatological consultants. The examination involved the whole body including the scalp and nails. Patients with renal failure, hepatic insufficiency, a history of cardiovascular, cerebrovascular or connective tissue disease, hypertension or epithelial dysplasia were excluded from the study, as were those undergoing systemic treatment with steroids or other drugs, immunosuppressive treatment, retinoids, lipid-lowering therapy, or antihypertensive or antiplatelet drugs. The study was approved by the local ethics committee. Informed consent was obtained from all participants.
Clinical and biochemical parametersBody height and weight, blood pressure, and body mass index were measured. Serum TG, low-density lipoprotein (LDL) cholesterol, HDL cholesterol, and glucose levels were determined in samples collected after a 12-hour fasting period. Total plasma cholesterol, TG, and HDL cholesterol were measured by an enzymatic colorimetric method using an autoanalyzer (Olympus AU 600) and reagents from Olympus Diagnostics GmbH, Hamburg, Germany. LDL cholesterol levels were calculated by the Friedewald formula. Blood glucose was measured by the glucose oxidase method. Blood was collected in tripotassium EDTA tubes. Blood counts were performed on an XT-1800i Hematology Analyzer (Sysmex Corporation, Kobe, Japan). Baseline neutrophil/lymphocyte ratio (NLR) was determined by dividing neutrophil count by lymphocyte count and baseline platelet/lymphocyte ratio (PLR) by dividing platelet count by lymphocyte count.
Echocardiographic examinationThe echocardiographic examination was performed at rest, with the patient in left lateral decubitus position, using a commercially available echocardiographic device (Vivid 7, GE Medical Systems, Milwaukee, WI, USA) with a 3-MHz transducer, by a single experienced echocardiographer (M.E.) who was blinded to the clinical data. Using M-mode echocardiography, long-axis measurements were obtained at the level distal to the mitral valve leaflets according to the current recommendations of the American Society of Echocardiography.17
Measurement of epicardial fat tissueEFT was measured on the free wall of the right ventricle in parasternal long-axis view, as previously described and validated.18 EFT was described as an echo-free space in the pericardial layers on two-dimensional echocardiography, and its thickness was measured perpendicularly to the free wall of the right ventricle at end-systole for 3-10 cardiac cycles. The measurement was performed at a point on the free wall of the right ventricle along the midline of the ultrasound beam, perpendicular to the aortic annulus. In order to increase confidence in the results, EFT measurement was performed at two different times and the percentage of the R-R interval with the least amount of motion was used.
Statistical analysisThe Kolmogorov-Smirnov test was used to assess normal distribution. Continuous variables were expressed as mean±SD and categorical variables were expressed as numbers and percentages. The Student's t test was used to compare continuous variables and the Mann-Whitney U test was used for non-normally distributed data. Differences in the distribution of categorical variables were assessed by chi-square analysis. Pearson and Spearman analyses were used for correlation analysis. Multiple linear regression analysis was performed for parameters affecting EFT. p values less than 0.05 were considered statistically significant. SPSS version 16.0 (SPSS, Chicago, IL, USA) was used for all statistical analyses.
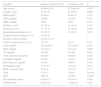
ResultsDemographic, clinical, hematological and biochemical characteristics of patients with LP and control subjects are shown in Table 1. Mean duration of LP was 20.51±11.40 months. No statistical differences was found between LP and controls except in terms of NLR, PLR, EFT thickness, hsCRP and HDL cholesterol (p<0.001, p<0.001, p=0.005, p=0.001, p=0.001 and p=0.001, respectively). There were positive correlations between EFT thickness and PLR, NLR, duration of LP, and hsCRP (p<0.001, p<0.001, p=0.002 and p<0.001, respectively) (Table 2). As shown in Table 3, in multivariate analysis, after adjustments for relevant confounders, LDL cholesterol, hsCRP, PLR and duration of LP were independent predictors of EFT thickness in patients with LP (β=0.231, p=0.014; β=0.205, p=0.037; β=0.361, p=0.001 and β=0.133, p=0.047, respectively).
Baseline demographic, clinical, hematological and biochemical characteristics of study and control subjects.
| Variable | Patients with LP (n=54) | Controls (n=50) | p |
|---|---|---|---|
| Age (years) | 45.68±13.01 | 47.29±6.88 | 0.475 |
| Female, n (%) | 32 (59.3) | 30 (60.8) | 0.866 |
| BMI (kg/m2) | 28.8±4.2 | 29.4±5.0 | 0.518 |
| SBP (mmHg) | 126±9 | 127±12 | 0.262 |
| DBP (mmHg) | 79±6 | 78±9 | 0.577 |
| Diabetes, n (%) | 10 (18.5) | 14 (29.2) | 0.221 |
| Smoking, n (%) | 15 (27.7) | 14 (29.2) | 0.284 |
| Hypercholesterolemia, n (%) | 22 (40.7) | 13 (26.8) | 0.161 |
| Topical steroid treatment, n (%) | 30 (55.5) | - | - |
| Duration of LP (months) | 20.51±11.40 | - | - |
| Positive family history, n (%) | 17 (31) | 8 (17) | 0.111 |
| LDL (mg/dl) | 118.5±39.4 | 117.4±33.7 | 0.891 |
| HDL (mg/dl) | 42.8±10.3 | 55.4±2.5 | 0.005 |
| TG (mg/dl) | 161±97 | 141±82 | 0.281 |
| Total cholesterol (mg/dl) | 203±44 | 192±36 | 0.207 |
| Creatinine (mg/dl) | 0.8±0.2 | 1.1±0.4 | 0.228 |
| Blood glucose (mg/dl) | 97±30 | 109±37 | 0.101 |
| Hemoglobin (g/l) | 11.4±3.4 | 12.1±2.3 | 0.475 |
| WBC count (103/μl) | 7.6±1.6 | 7.5±1.6 | 0.772 |
| NLR | 3.1±1.3 | 1.8±0.5 | <0.001 |
| PLR | 165±31 | 107±26 | <0.001 |
| EFT thickness (mm) | 0.89±0.21 | 0.53±0.11 | 0.001 |
| hsCRP (mg/l) | 4.67±3.35 | 1.48±0.50 | 0.001 |
BMI: body mass index; DBP: diastolic blood pressure; EFT: epicardial fat tissue; HDL: high-density lipoprotein; hsCRP: high-sensitivity C-reactive protein; LDL: low-density lipoprotein; LP: lichen planus; NLR: neutrophil/lymphocyte ratio; PLR: platelet/lymphocyte ratio; SBP: systolic blood pressure; TG: triglycerides; WBC: white blood cell.
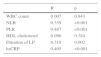
Correlation analysis of epicardial fat tissue and confounding variables.
| R | p | |
|---|---|---|
| WBC count | 0.007 | 0.943 |
| NLR | 0.359 | <0.001 |
| PLR | 0.487 | <0.001 |
| HDL cholesterol | 0.090 | 0.384 |
| Duration of LP | 0.318 | 0.002 |
| hsCRP | 0.405 | <0.001 |
HDL: high-density lipoprotein; hsCRP: high-sensitivity C-reactive protein; LP: lichen planus; NLR: neutrophil/lymphocyte ratio; PLR: platelet/lymphocyte ratio; WBC: white blood cell.
Multivariate linear regression analysis of predictors of epicardial fat tissue in patients with lichen planus.
| β | p | |
|---|---|---|
| Age | 0.101 | 0.275 |
| Diabetes | -0.164 | 0.062 |
| Smoking | 0.027 | 0.765 |
| LDL cholesterol | 0.231 | 0.014 |
| HDL cholesterol | -0.060 | 0.492 |
| hsCRP | 0.205 | 0.037 |
| NLR | 0.179 | 0.069 |
| PLR | 0.361 | 0.001 |
| LVEF | -0.071 | 0.408 |
| Duration of LP | 0.133 | 0.047 |
HDL: high-density lipoprotein; hsCRP: high-sensitivity C-reactive protein; LDL: low-density lipoprotein; LP: lichen planus; LVEF: left ventricular ejection fraction; NLR: neutrophil/lymphocyte ratio; PLR: platelet/lymphocyte ratio.
The major findings of our study are that EFT thickness is increased in patients with LP compared to controls, and that duration of LP, LDL cholesterol, hsCRP, and PLR are independent predictors of increased EFT thickness in patients with LP.
LP is an immune-mediated disease of unknown cause that affects the skin, genitalia, mucous membranes and appendages, in which antigens are processed by Langerhans cells and then presented to T lymphocytes. Previous studies showed that patients with LP have high lipid levels, acute phase reactants and atherogenic index. Similar to previous studies, in our population HDL cholesterol levels were lower in patients with LP than controls. Several cytokines, such as TNF-α, IL-2, and IL-6, have been implicated in the increased lipids levels in patients with LP.4,19
Studies have shown that LP is associated with cardiovascular risk factors including dyslipidemia, diabetes, and increased oxidative stress.3,5,20,21 Most cardiovascular disorders (including atherosclerosis, hypertension, insulin resistance, dyslipidemia, and arrhythmias) have similar mechanisms, such as chronic inflammation, endothelial dysfunction, and increased oxidative stress.22 In our study, indirect parameters of oxidative stress levels (PLR and NLR) were higher in patients with LP than in controls.
Saleh et al. have shown that serum homocysteine, fibrinogen and hsCRP are significantly higher in patients with lichen planus.23 In LP, Th1 inflammatory cytokines such as TNF-α, IL-4, IL-6 and IL-10 are increased in skin and blood.4 The inflammatory mediators involved in LP may have a range of effects on insulin signaling, lipid metabolism, and adipogenesis.
EFT shares the same embryological origin as intra-abdominal visceral adipose tissue.24 Similarly to other visceral adipose tissues, epicardial adipose tissue functions as a lipid store that secretes hormones, inflammatory cytokines and chemokines such as TNF-α, monocyte chemoattractant protein (MCP)-1, IL-6 and plasminogen activator inhibitor-1 (PAI-1).25 EFT is associated with higher levels of atherogenic IL-6 in subjects with CAD.26
It is important to identify subclinical atherosclerosis, for which noninvasive tests play an important role. A close association between EFT and subclinical atherosclerosis, coronary calcium score, and presence and severity of coronary stenosis has been reported in several observational studies.27–32
EFT (as measured by echocardiography) is associated with increased left ventricular mass, endothelial dysfunction, and the presence and severity of CAD.29 It is also independently associated with blood pressure, LDL cholesterol, fasting glucose, and both traditional and novel cardiovascular risk factors.33 Although EFT thickness was increased in patients with LP, we were unable to show these associations in comparisons between patients with LP and control subjects.
EFT is an endocrine and paracrine source of cytokines, and its thickness is correlated with several circulating proatherogenic and proinflammatory adipokines such as visfatin, PAI-1, monocyte chemoattractant protein-1 (MCP-1), and CRP.17,33,34 However, it is inversely related to adiponectin, an anti-inflammatory and antiatherogenic adipokine.12 In our study, hsCRP levels correlated with EFT and were an independent predictor of increased EFT thickness.
A recent article by Aksu et al. showed reduced flow-mediated dilatation and increased carotid-intima media thickness, which are predictors of atherosclerosis and cardiovascular end organ damage, in LP patients.35 In our study, we found that duration of LP is correlated with EFT, and also that duration of LP is an independent predictor of increased EFT, which is a predictor of subclinical atherosclerosis.
Why is EFT thickness increased in patients with LP? One possible underlying mechanism may be persistent inflammation. Inflammatory adipokines such as TNF-α, MCP-1, and IL-6 play a significant role in inflammation and can potentially lead to a predisposition to atherosclerosis.
ConclusionIn conclusion, we have shown that patients with LP have more EFT, indicating an increased risk for atherosclerosis. Further long-term prospective studies are needed to clarify the clinical utility and prognostic importance of the link between LP and atherosclerosis.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.