Ebstein's anomaly is a rare complex congenital heart defect of the tricuspid valve. We aimed to describe the frequency, clinical profile, and early and short-term post-operative results in patients under the age of 18 years operated for this anomaly in a tertiary center in Angola.
MethodsA retrospective cross-sectional study was conducted over a period of 37 months. We analyzed all patients diagnosed with congenital heart defects.
ResultsOf the 1362 patients studied, eight (0.6%) had Ebstein's anomaly; six patients (75%) were female. Mean age was 69±59 months. Five patients were in NYHA functional class III or IV. Mean cardiothoracic index was 0.72. Seven patients (87.5%) had severe tricuspid regurgitation and five (62.5%) had another associated congenital heart defect. All patients were operated: two had complications and one (12.5%) died in the early post-operative period. The mean follow-up time was 1.22±0.6 years, and mortality during follow-up was 12.5% (n=1). At the end of the study, of the five patients in whom cone reconstruction was performed, four (80%) were in functional class I. Mean cardiothoracic index decreased to 0.64. Three patients had mild and two had moderate tricuspid regurgitation. The patient who underwent cone reconstruction and a Glenn procedure was in functional class I.
ConclusionThe frequency of Ebstein's anomaly was similar to that in other centers. Cone reconstruction was viable in the majority of patients, with good early and short-term results.
A anomalia de Ebstein é uma cardiopatia congénita complexa e rara da válvula tricúspide. Descrever a frequência, o perfil clínico e os resultados pós operatórios imediatos desta anomalia em crianças e adolescentes.
MétodosEstudo transversal retrospetivo no único centro com tratamento integrado em cardiopatias congénitas em recém nascidos, crianças e adolescentes (<18 anos de idade) em Angola, num período de 37 meses. Foram analisados todos os doentes com diagnóstico de cardiopatia congénita. O diagnóstico foi feito com base no exame clínico e dados da ecocardiografia transtorácica e Doppler. Os ecocardiogramas foram realizados pelos Cardiologistas Pediátricos numa máquina Vivid 7 G.E.
ResultadosForam analisados 1362 ecocardiogramas sequenciais. Oito doentes (0,6%) tinham anomalia de Ebstein, destes 6 (75%) eram do género feminino. As idades variaram entre 4 a 168 meses, a média foi de 69 ± 59 meses. Cinco estavam em classe funcional III ou IV da NYHA. A média do índice cardiotorácico foi de 0,72. Sete doentes (87,5%) tinham regurgitação tricúspide grave e 5 (62,5%) tinham outra cardiopatia congénita associada. Todos os doentes foram submetidos a intervenção cirúrgica. Dois tiveram complicações no pós-operatório imediato. A mortalidade pós operatória foi de 12,5% (n=1).
ConclusãoA frequência da Anomalia de Ebstein encontrada foi semelhante a de outros Centros. A técnica de Cone foi viável na maior parte dos pacientes. A mortalidade pós operatória imediata foi baixa.
atrial septal defect
congenital heart defect
cone reconstruction
cardiothoracic index
Ebstein's anomaly
modified Blalock-Taussig
New York Heart Association
pulmonary artery hypoplasia
patent ductus arteriosus
right ventricular
tricuspid valve
Wolff-Parkinson-White
Ebstein's anomaly (EA) is a rare complex congenital heart defect (CHD) of the tricuspid valve (TV) first described by Wilhelm Ebstein in 1866.1 It occurs in about 1 per 200000 live births and accounts for less than 1% of all CHDs.2–8 The anatomical basis of EA consists in displacement by more than 8 mm/m2 body surface area of the septal and posterior leaflets of the TV in relation to the position of the mitral valve anterior leaflet.4,6 The genetic etiology is unknown.5 The usual clinical presentation is cyanosis, heart failure, arrhythmia and sudden death.3,8 The severity and onset of symptoms depend on the degree of displacement of the TV leaflets.3 Transthoracic echocardiography is the gold standard for diagnosis of this entity.4,6 EA may coexist with other CHDs, genetic syndromes, or Wolff-Parkinson-White (WPW) syndrome.2–4,9 Surgical management of EA depends on the patient's age, the clinical presentation and association with other CHDs, and therefore the surgical approach should be individualized.9,10 Ebstein's anomaly is classified among the category of CHDs that requires early and specific health care.7,8 In this context, the present study aimed to describe the experience of a tertiary center in a developing country in managing this complex disease in patients less than 18 years old.
MethodsBased on the records of the Cardiothoracic Center of Clínica Girassol, previously described,11 a retrospective study was performed that included all patients with CHDs over a period of 37 months (March 29, 2011 to April 29, 2014). Data on clinical presentation, chest X-ray, electrocardiography, echocardiographic studies and surgical reports were analyzed. Transthoracic echocardiography and Doppler studies was performed by pediatric cardiologists using a GE Vivid 7 system (GE Healthcare, Milwaukee, WI, USA) with multiple frequency probes (3S-RS, 4C-RS and RS-6S) in accordance with the recommendations of the American College of Cardiology/American Heart Association.12 Only the first echocardiogram was validated. A diagnosis of EA was made when a displacement of the septal and posterior leaflets of the TV was observed of more than 8 mm/m2 body surface area in relation to the position of the mitral valve anterior leaflet.4,6 The surgical indications were the conventional ones: NYHA functional class III or IV; NYHA class I or II with cardiothoracic index (CTI) of 0.65 or greater; progressive right ventricular (RV) dilation; significant cyanosis and polycythemia.9–11 In patients with favorable anatomy cone reconstruction (CR) of the TV was performed as described by Da Silva et al.15 Atrial septal defect or patent foramen ovale, if present, was closed at the time of repair. Cavopulmonary shunt was reserved for patients less than six months old and for those with significant RV dysfunction. The modified Blalock-Taussig (MBT) shunt was reserved for patients with pulmonary artery hypoplasia (PAH). Follow-up was in the first half of June 2014, when all patients underwent clinical, radiological and echocardiography assessment.
A descriptive statistical analysis was performed (absolute and relative frequencies, mean and standard deviation).
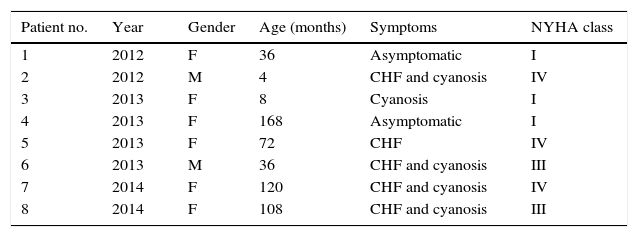
ResultsDuring the study period, 1362 patients under the age of 19 years with a diagnosis of CHD were analyzed, eight (0.6%) of them with Ebstein's anomaly. Demographic data, clinical presentations, and NYHA functional class of the study population are shown in Table 1. Mean age was 69±59 months, ranging from 4 to 168 months. Female gender was predominant, with a female:male ratio of 3:1. Regarding clinical presentation, five patients (62.5%) had signs and symptoms of heart failure, three of them in NYHA functional class IV and two in class III, and four also had cyanosis. Two patients (25%) were referred for a heart murmur and one for cyanosis; these were in NYHA functional class I. Data on X-ray, echocardiography, indications for surgery, type of surgical techniques and complications are presented in Table 2.
Distribution of demographic data, year of diagnosis, clinical presentation and NYHA functional class.
| Patient no. | Year | Gender | Age (months) | Symptoms | NYHA class |
|---|---|---|---|---|---|
| 1 | 2012 | F | 36 | Asymptomatic | I |
| 2 | 2012 | M | 4 | CHF and cyanosis | IV |
| 3 | 2013 | F | 8 | Cyanosis | I |
| 4 | 2013 | F | 168 | Asymptomatic | I |
| 5 | 2013 | F | 72 | CHF | IV |
| 6 | 2013 | M | 36 | CHF and cyanosis | III |
| 7 | 2014 | F | 120 | CHF and cyanosis | IV |
| 8 | 2014 | F | 108 | CHF and cyanosis | III |
CHF: congestive heart failure; F: female; M: male; NYHA: New York Heart Association.
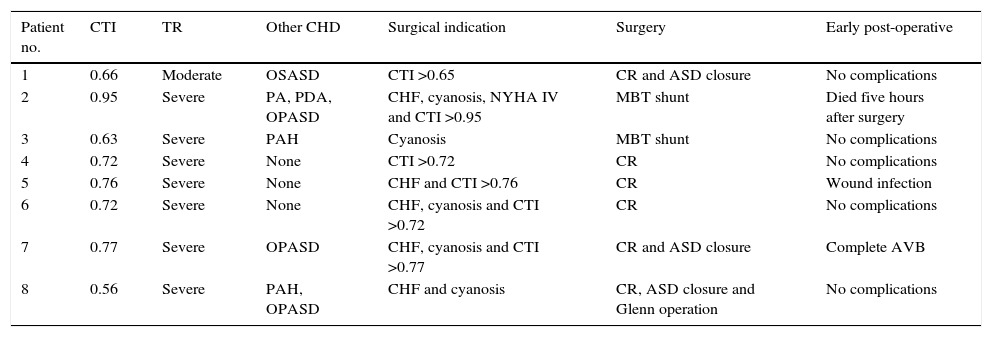
Cardiothoracic index, echocardiographic findings, surgical indications, surgery performed and early post-operative evaluation.
| Patient no. | CTI | TR | Other CHD | Surgical indication | Surgery | Early post-operative |
|---|---|---|---|---|---|---|
| 1 | 0.66 | Moderate | OSASD | CTI >0.65 | CR and ASD closure | No complications |
| 2 | 0.95 | Severe | PA, PDA, OPASD | CHF, cyanosis, NYHA IV and CTI >0.95 | MBT shunt | Died five hours after surgery |
| 3 | 0.63 | Severe | PAH | Cyanosis | MBT shunt | No complications |
| 4 | 0.72 | Severe | None | CTI >0.72 | CR | No complications |
| 5 | 0.76 | Severe | None | CHF and CTI >0.76 | CR | Wound infection |
| 6 | 0.72 | Severe | None | CHF, cyanosis and CTI >0.72 | CR | No complications |
| 7 | 0.77 | Severe | OPASD | CHF, cyanosis and CTI >0.77 | CR and ASD closure | Complete AVB |
| 8 | 0.56 | Severe | PAH, OPASD | CHF and cyanosis | CR, ASD closure and Glenn operation | No complications |
ASD: atrial septal defect; AVB: atrioventricular block; CHD: congenital heart defect; CHF: congestive heart failure; CR: cone reconstruction; CTI: cardiothoracic index; MBT: modified Blalock-Taussig; PA: pulmonary atresia; OPASD: ostium primum atrial septal defect; OSASD: ostium secundum atrial septal defect; PAH: pulmonary artery hypoplasia; PDA: persistent ductus arteriosus; RA: right atrium; RV: right ventricle; TR: tricuspid regurgitation.
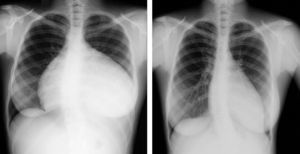
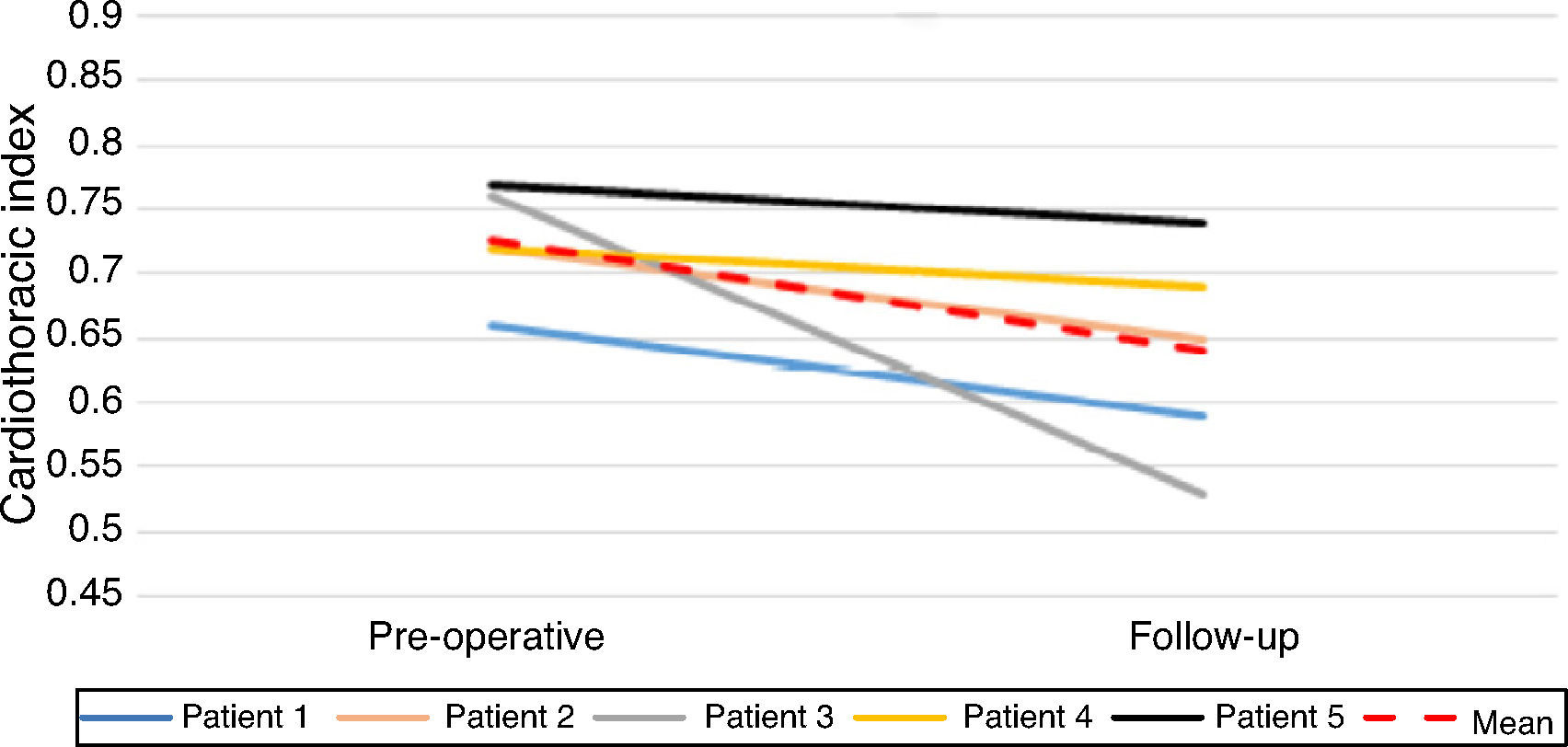
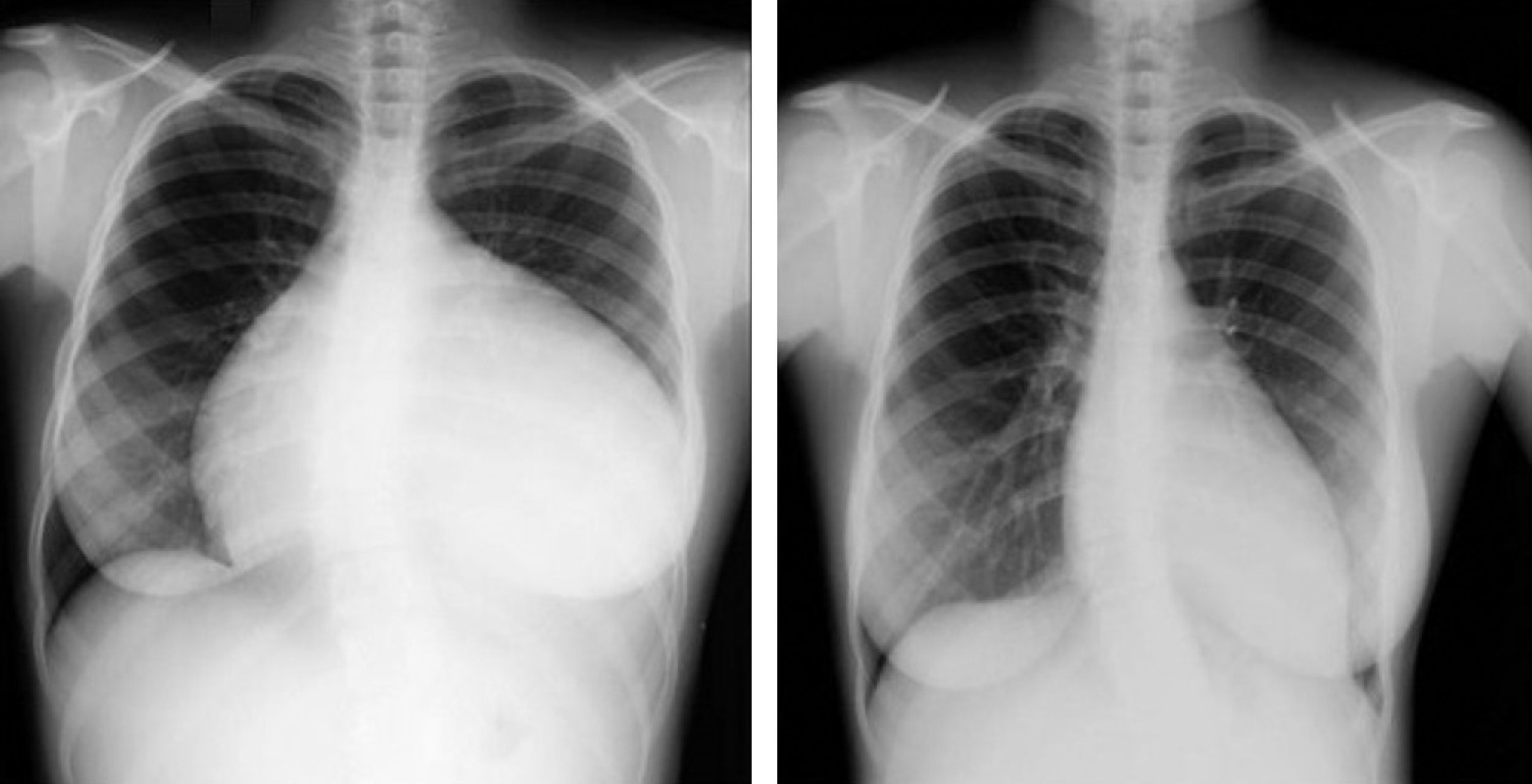
Mean CTI was 0.72, ranging from 0.56 to 0.95. Seven patients (87.5%) had severe tricuspid regurgitation (TR) and five (62.5%) had other CHDs associated with EA. Atrial septal defect (ASD) was the most frequent CHD (n=3; 37.5%). In two cases (25%) EA was associated with PAH. In one of these cases an extremely rare association was found (ostium primum ASD, pulmonary atresia and patent ductus arteriosus [PDA]). No patients with a genetic syndrome or WPW syndrome were found. All patients underwent surgical intervention. The indications for surgery were: heart failure, one patient; heart failure and cyanosis, four patients; cyanosis, one patient; and cardiothoracic index >0.65, in two asymptomatic patients. In five patients CR of the tricuspid valve was performed with 100% immediate success. In these patients, the mean bypass time was 82.8±42.2 minutes (46–148 minutes) with mean aortic cross-clamp time of 56.4±32.3 minutes (27–106 minutes). De Vega annuloplasty was performed concomitantly in two (25%) patients. At the time of CR, ASD closure was performed in two patients. Two patients (25%) had post-operative complications: one wound infection and the other complete atrioventricular block, and a DDD permanent pacemaker was implanted. Mean hospital stay was 10.6±2.7 days. At discharge, in this group two patients had no TR and three had mild TR. The survival rate was 100%. The remaining three patients, in two with PAH an MBT shunt was performed, and in one patient with unfavorable anatomy and severe EA a Glenn operation was performed along with CR of the TV. The patient with the rare association of ostium primum ASD, pulmonary valve atresia and PDA, who was treated by an MBT shunt, died five hours after surgery. The mean follow-up was 1.22±0.6 years. In this period, another patient who underwent an MBT shunt died (12.5%). At the end of the study four patients (80%) were in NYHA functional class I (Figure 1). CTI decreased in all patients, by a mean of 0.72–0.64 (Figure 2). The third patient showed the greatest improvement (Figure 3). Three patients (60%) had mild and two (40%) had moderate TR on the last echocardiogram. The patient with a permanent pacemaker was readmitted five months after surgery for pericardial effusion and minimal right pleural effusion and was discharged in NYHA class II seven days after readmission. The patient who underwent a Glenn procedure along with CR of the TV at the end of the follow-up period was in NYHA class I.
DiscussionThis study revealed that 0.6% of patients with CHDs referred to our center had EA, a similar finding to those reported by other authors.2–8 However, it contrasts with the high frequency of EA (2%) described in a study carried in the Sudanese population.13 In the present study, females had an almost three-fold higher probability of having EA. This result contrasts with those of Anderson9 and Da Silva,15 who report a slight predominance of males, and with other studies that described no predominance of either gender.2–6,8,13,14 In developed countries, the diagnosis of CHD is made in the fetal or neonatal period, enabling an early approach and improving the prognosis of these patients.2,3,8,14 In Africa,13 particularly in Angola, CHDs still tend to be diagnosed later,16 as shown by the mean age (29±36 years) found in the present series. Access to health care services are still a serious problem in our continent, from the prenatal period to old age, which is why we have a small sample without neonates with severe forms of EA and older patients with good functional status. In the present study more than half of the patients were in NYHA functional class III or IV. This result is similar to that reported in a study conducted in Sudan, in which the authors found that half of the patients were symptomatic.13 The mean CTI found in this series was higher than that reported by Arizmendi et al. and Ali and Nimeri, 0.65 and 0.64, respectively.3,13 It should be noted that CTI >0.65 is consistently associated with a worse prognosis,11 and the mean CTI in this study was greater than this cut-off value, suggesting that our patients were at high risk.
Transthoracic echocardiography is the most important diagnostic test for EA, to determine TV morphology and physiology and to assess the cardiac chambers and the presence of other CHD.4,6,14 Severe tricuspid regurgitation in our patients was almost twice as frequent as that reported by Ali and Nimeri (33%).13 Dilation of the right cardiac chambers and therefore of the tricuspid annulus is the most likely cause of the severity of tricuspid regurgitation found in the population studied.6,9,17 EA is frequently associated with other CHDs, in more than 50% of cases, most often ASD.2,3,6,10,14,15 Although in smaller proportions, the results of this study reflect this frequency. On the other hand, Arizmendi et al.3 reported pulmonary valve stenosis as the most frequent CHD (39%). Although associations between EA and certain genetic syndromes have been described, mainly trisomy 21 and WPW syndrome,9,14 these syndromes were not found in the present series. Finally, it is noteworthy that one patient in our series had an extremely rare association (ostium primum ASD, pulmonary atresia and PDA).18
The conventional surgical indications for the correction of EA are NYHA functional class III or IV; NYHA functional class I or II with CTI of 0.65 or greater; progressive RV dilatation; cyanosis (oxygen saturation <90%) and polycythemia.9–11 In the present series the indications for surgery were heart failure and/or cyanosis in six patients and CTI >0.65 in two asymptomatic patients. The complexity of the anatomical and functional changes in EA and the possibility of association with other CHDs mean that the surgical approach should be individualized. Cavopulmonary shunt is reserved for patients with severe RV dysfunction.9,15 The MBT shunt is generally reserved for patients with PAH.19
Various techniques for tricuspid valve reconstruction have been developed in the last 35 years, with different results.20,21 The most recent technique is CR, developed by da Silva et al.,16 which we use in our center. Although the number of patients is small, the present series showed an immediate success rate of 100% for CR, with clinical and echocardiographic improvement in short-term follow-up, in agreement with the good results for this technique reported by other authors.9,15 Da Silva et al. reported that CR was associated with low in-hospital mortality and was an effective and long-lasting repair of tricuspid regurgitation, restoring the functional area of the right ventricle and bringing clinical improvement in most patients in the long term.15 Anderson et al., describing the Mayo Clinic experience with CR, reported difficulties in reconstructing the sepal portion of the TV. Several techniques have been described to avoid this complication.15 Finally, in relation to ASD closure, partial closure of the foramen ovale enables preservation of right-to-left flow.
The low in-hospital mortality and long-term clinical improvement reported by da Silva et al.15 are supported by the Mayo Clinic experience, in which CR in 84 patients with EA aged under 21 years showed a success rate of 98%.9 In our present series also, there was an immediate success rate of 100%, with short-term clinical and echocardiographic improvement. However, the technique could not be applied in two patients for the reasons described above.
ConclusionsThe prevalence of EA found in this series was similar to other centers. Our patients had access to medical care at a critical stage of the disease. CR was performed in the majority of patients with excellent immediate and short-term results.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.




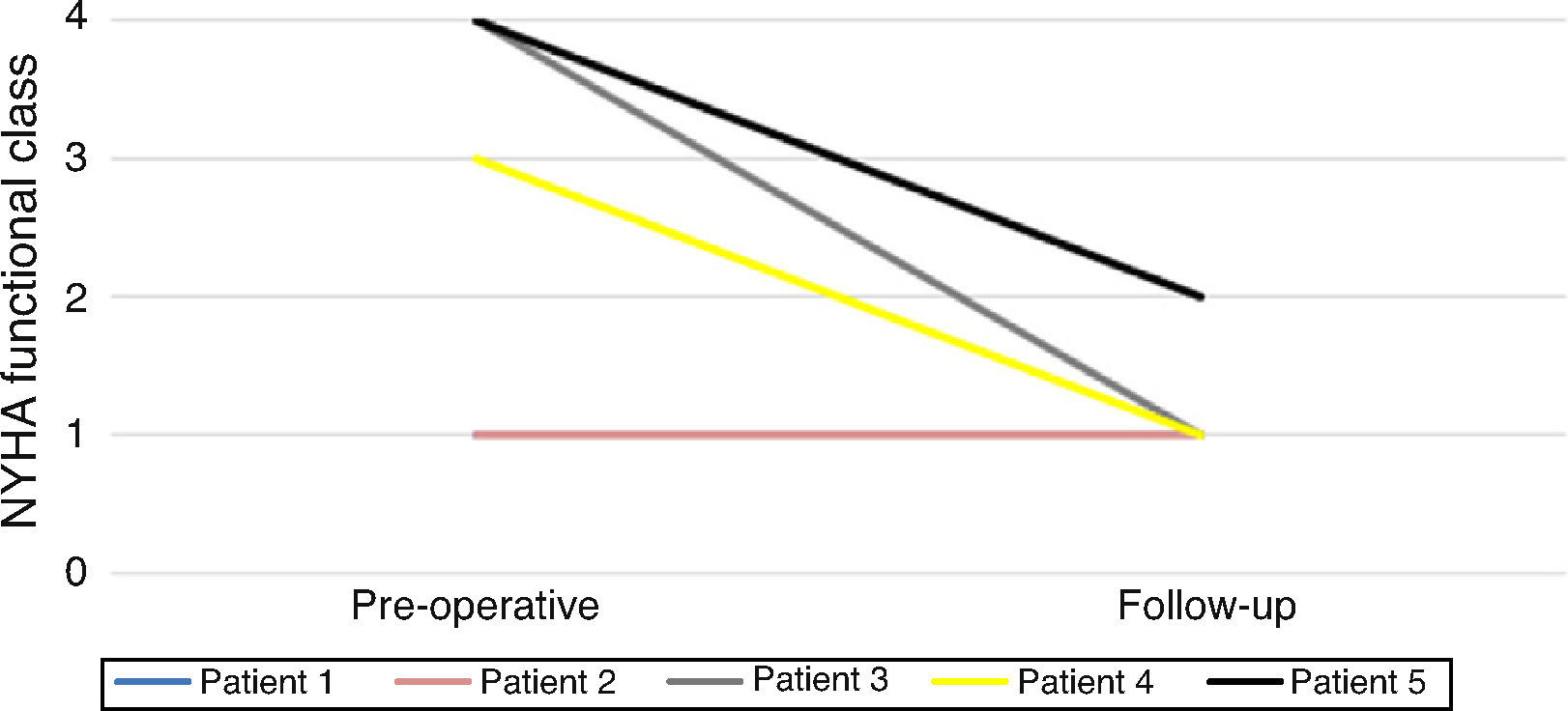
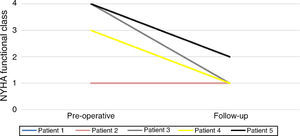 NYHA: New York Heart Association.' title='Evolution of functional class in the five patients undergoing cone reconstruction.
NYHA: New York Heart Association.' title='Evolution of functional class in the five patients undergoing cone reconstruction.