Behçet's disease is a chronic relapsing multisystem autoinflammatory condition, in which cardiac involvement is rare, but among the most life-threatening complications. Treatment is largely empirical, and is aimed at suppressing vasculitis. In this role glucocorticoids and colchicine are frequently used.
We present the case of a 42-year-old male with previously diagnosed Behçet's disease presenting to our emergency department with an anterior-inferior STEMI. He presented combined thrombosis of the distal anterior descending coronary artery and proximal right coronary artery, and was treated with sequential primary percutaneous coronary interventions and implantation of drug-eluting stents, but required two interventions due to high thrombotic load.
His clinical course during hospitalization was good, with no systolic dysfunction at discharge. During follow-up, he has so far had no new cardiovascular events.
A doença de Behçet (BD) é uma doença autoimune crónica e recidivante, na qual o envolvimento cardíaco é muito raro, mas encontra-se entre as complicações fatais. O tratamento é em grande parte empírico e destina-se a suprimir a vasculite. Nesse papel, os glicocorticoides e a colchicina são frequentemente utilizados.
Apresentamos o caso de um homem de 42 anos, com diagnóstico prévio de doença de Behçet que recorreu ao nosso serviço de emergência com STEMI anteroinferior. Apresentou trombose simultânea da artéria coronária descendente anterior distal e da artéria coronária direita proximal e foi tratada com intervenção coronária percutânea primária com stent revestido de drogas de forma sequencial, mas necessitando de duas intervenções devido à recorrência trombótica.
Teve boa evolução clínica durante o internamento, não apresentando disfunção sistólica na alta. Durante o seguimento, até à data, não ocorreu novo evento cardiovascular.
Behçet's disease (BD) is a chronic relapsing multisystem autoinflammatory condition, one of a group of heritable inflammatory-mediated disorders characterized by idiopathic attacks of systemic inflammation with a lack of obvious antigen-specific antibodies or immune response.1 BD mostly affects ethnic groups of Mediterranean and Asian origin that have historically settled along the ancient Silk Road. The prevalence of the disease is 80-370/100000 in Turkey, whereas it is 13-20/100 000 in Japan, Korea, Iran, Iraq, and Saudi Arabia.2 Cardiac involvement with frank clinical presentation is rare in BD,3 but is among its most life-threatening complications. These include pericarditis, coronary artery stenosis or aneurysm, myocarditis, cardiomyopathy, congestive heart failure, valve disease, endocarditis, intracardiac thrombosis, and aneurysms of the aorta or its branches.3
Case reportWe present the case of a 42-year-old male diagnosed with BD at the age of 24 years, with only skin and mucosal lesions and currently medicated with colchicine once daily and prednisolone every other day, who developed sudden-onset oppressive chest pain early in the morning. He was attended on the spot by an emergency team, and an electrocardiogram was promptly performed, revealing anterior-inferior ST-elevation myocardial infarction. Aspirin 300 mg, clopidogrel 600 mg and intravenous (IV) enoxaparin 40 mg were administered, and he was immediately referred for percutaneous coronary intervention (PCI).
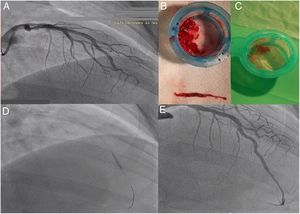
Acute thrombotic occlusion of the distal left anterior descending artery (LAD) was promptly identified (Figure 1A) and aspiration of thrombus was performed (Figure 1B and C), requiring multiple passages, followed by implantation of a 2.75 mm×18 mm Resolute Onyx drug-eluting stent (Figure 1D and E).
Left coronary artery angiography and angioplasty: (A) initial injection showing the left anterior descending coronary artery with acute thrombosis; aspirated material from the coronary territories, showing white (B) and red thrombi (C); (D) placement of a 2.75 mm×18 mm Resolute Onyx stent; (E) final angiographic result.
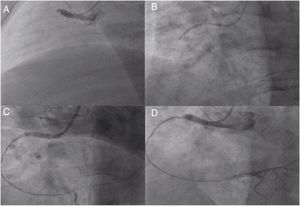
Right coronary artery (RCA) angiography was then performed, and proximal thrombotic occlusion of this artery was also observed (Figure 2A). Successive new aspirations were performed, complemented by balloon angioplasty (Figure 2B). During the procedure, new thrombotic material was formed and therefore IV tirofiban and additional IV heparin was administered. Intracoronary administration of nitrates and adenosine was also required due to no reflow (Figure 2C). Given the high thrombotic load, coronary patency and the high contrast dose already given, the immediate outcome was considered acceptable (Figure 2D) and a new coronary angiography was scheduled. The patient was admitted to the intensive care unit pain-free and clinically stable in Killip class I.
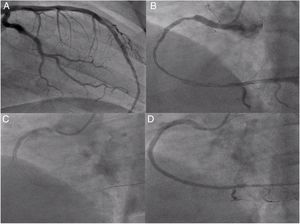
The second coronary angiography, performed after approximately 48 hours, presented a good result from the previous angioplasty of the LAD (Figure 3A) and diffuse disease and distal dissection of the RCA (Figure 3B). We decided to perform RCA angioplasty, initially with balloon, followed by sequential implantation of three Resolute Onyx drug-eluting stents (2.5 mm×38 mm, 3 mm×38 mm and 3.5 mm×38 mm) (Figure 3C), obtaining a good final result (Figure 3D).
Second angiography and angioplasty on day 2 of hospitalization: (A) left coronary artery confirming good outcome; (B) right coronary angiography showing diffuse right coronary artery disease from the proximal segment to the crux, with distal dissection; (C) implantation of the last stent, 3.5 mm×38 mm Resolute Onyx; (D) final result of the second right coronary angioplasty.
Pre-discharge transthoracic echocardiography revealed the left ventricle with normal dimensions and overall systolic function (left ventricular ejection fraction 56%), and hypokinesis of the basal inferior wall. The patient was discharged on the fifth day, medicated with aspirin 100 mg once daily, ticagrelor 90 mg twice daily, atorvastatin 40 mg once daily, ramipril 2.5 mg once daily, ivabradine 5 mg twice daily, colchicine 1 mg once daily and pantoprazole 20 mg once daily.
After discharge the patient was referred for a cardiology consultation in addition to previous medical consultations. Prednisone was introduced three months after the event by the rheumatology team. At the six-month cardiology consultation, the patient presented free of angina with good functional capacity, and no new cardiovascular events have been reported.
DiscussionCoronary artery disease is extremely uncommon in BD, with a reported prevalence of 0.5%.4 As in the case presented, most BD patients with coronary events had previously been diagnosed with the disease and were on regular treatment; less commonly, coronary complications may occur as the first manifestation of the disease.
In young adults with myocardial infarction (MI), non-atherosclerotic etiologies such as embolization, trauma, arteritis, spasm, dissection, and congenital abnormalities should be considered. However, in BD, coronary arteritis has been identified as an independent pathophysiological mechanism for MI.5 BD involves widespread vasculitis with multisystem involvement. The prognosis is extremely variable; some patients present only minor skin and mucosal lesions, while others may have life-threatening central nervous system and gastrointestinal tract involvement and pulmonary artery aneurysms.6,7
Treatment of cardiovascular involvement in BD is largely empirical, and is aimed toward suppressing the vasculitis.8 Glucocorticoids are administered for years in almost any organ involvement in BD, with dramatic response in most cases. However, liberal use can led to severe adverse reactions, and strategies to minimize these side effects have been suggested. Administering the minimum effective dose (not traditional textbook-based doses) tailored for each individual patient is a rational approach to treatment with corticosteroids.5 The other common systemic agent used in BD is colchicine, which reduces neutrophil counts.9
Acute MI can be treated by PCI or surgical revascularization.10 In the case presented, the acute onset and total artery occlusion forced us to choose PCI as the primary strategy. As seen in the literature, our patient presented with severe coronary lesions11 and an unexpected double coronary thrombosis. Initially it was decided to perform combined PCI of both coronary arteries, but as the RCA procedure was complicated by recurrent new thrombus formation, and since adequate coronary flow was established, it was opted not to stent the RCA immediately. This proved to be the right decision. As is the practice in our catheterization laboratory, both procedures were done via the radial artery. This appears to be a sound option, since in BD an inflammatory obliterative endarteritis of the vasa vasorum, most likely brought about by immune deposition, can cause destruction of the media and fibrosis and thus predispose the arterial wall to aneurysm formation that eventually ruptures.12 It is generally accepted that during the acute phase of vasculitis, the inflamed and fragile tissues are difficult to manipulate, with a high frequency of complications encountered.13 This leads to an increased risk of iatrogenic coronary dissection and secondary aneurysms.
To date there are no specific recommendations regarding antiplatelet therapy in BD. PCI in these patients tends to result in an increased rate of stent thrombosis and thrombosis recurrence during long-term follow-up, which may be influenced by traditional and non-traditional risk factors.11 We decided to apply the standard antiplatelet regimen, without adverse events so far, since at the time of writing, the patient had had no new cardiovascular events.
ConclusionThis clinical case presents a rare complication of a rare disease, with important implications for diagnosis, treatment and follow-up. Knowledge of the nuances of DB is essential for the proper treatment of these patients.
Conflicts of interestThe authors have no conflicts of interest to declare.