A 56-year-old man had been referred to our department in 1978 at age 22 with a diagnosis of congenital cyanotic heart disease, and had undergone ventricular (VSD) and atrial septal defect (ASD) closure and repair of pulmonary valve stenosis. The chest X-ray showed mesocardia. He began to experience signs and symptoms of heart failure in 1992, with a systolic murmur audible over the left sternal border. Serial transthoracic echocardiography (TTE) showed a residual high VSD. Cardiac magnetic resonance imaging (MRI) in 1999 detected transposition of the great vessels but no VSD or ASD.
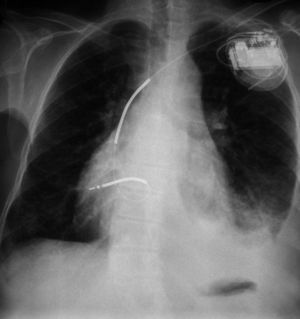
In 2005, the patient received an implantable cardioverter-defibrillator (ICD) due to syncopal ventricular tachycardia (Figure 1).
In 2011, he was hospitalized in Luxembourg for fever, headache, nausea and non-focal neurological alterations (stupor). Brain computed tomography revealed a cerebral abscess in the left medial frontal region, and transesophageal echocardiography (TEE) identified vegetations on the defibrillator lead. Blood cultures were positive for Streptococcus constellatus and Micromonas micros.
Apyretic for two weeks under antibiotic therapy, he was transferred to our department with the diagnoses of lead endocarditis and cerebral abscess, with corrected tetralogy of Fallot without ASD or VSD.
Following repeat TTE and TEE, the diagnosis of the underlying congenital heart disease was changed to congenitally corrected transposition of the great vessels and low ASD (Figures 2–5). The ICD system was removed. Since the patient had presented periods of third-degree atrioventricular block and was highly pacing-dependent during follow-up ICD consultations prior to hospitalization, and we wished to use the minimum amount of intravascular prosthetic material, a dual-chamber epicardial pacemaker and a subcutaneous ICD were implanted. He was discharged clinically stable.
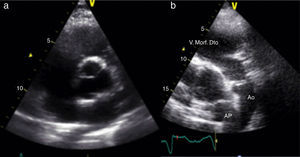
Transthoracic echocardiography: (a) anatomically normal image in parasternal short-axis view; (b) parasternal short-axis view showing parallel great vessels and morphologically right ventricle in anterior position in continuity with the aorta, also in anterior position (Video 1). Ao: aorta; AP: pulmonary artery; V. Morf. Dto: morphologically right ventricle.
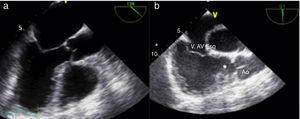
Transesophageal echocardiography: (a) anatomically normal image; (b) corresponding image showing absence of continuity between the aortic valve and left atrioventricular (morphologically tricuspid) valve through an infundibulum (asterisk); morphologically right ventricle in left position and aortic valve in normal continuity with systemic circulation (aorta) (Video 2). V Ao: aortic valve; V.AV Esq: atrioventricular valve in left position.
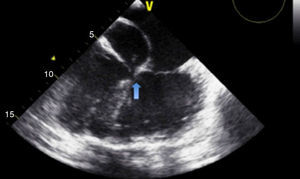
Transesophageal echocardiography showing insertion of the atrioventricular valves in the same plane (arrow), consistent with congenitally corrected transposition of the great vessels and atrioventricular septal defect, an association that occurs in 75% of cases2 (Video 3).
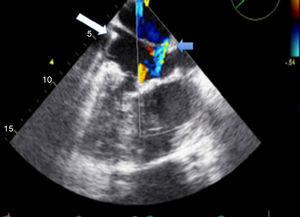
Transesophageal echocardiography showing right atrium receiving two venae cavae; morphologically mitral atrioventricular valve in right position; lead (white arrow) identifying the superior vena cava and morphologically left ventricle in right position; atrial septal defect with residual low shunt (blue arrow) (Videos 4 and 5).
It was concluded that the corrective surgery performed in 1978 resulted in a residual low ASD with a systemic-pulmonary shunt, detected by TTE but not confirmed by MRI, which was revealed to be the mechanism behind paradoxical systemic embolization.
Although it was not possible to obtain the surgical report from the patient's medical records, we found a case report1 published by the surgeon in 1979, which describes anatomical L-transposition of the great vessels, supporting the current diagnosis.
We highlight the importance of TTE and TEE study in the diagnosis of congenital heart disease (Table 1), particularly to identify residual shunts, which may not be detected by MRI. Identification of the residual shunt in this case was the determining factor in modifying the therapeutic approach.
Imaging features for a diagnosis of congenitally corrected transposition of the great vessels with double discordance: atrioventricular and ventriculo-arterial.
| Great vessels parallel to the aorta in anterior position (Figure 2). |
| Morphologically right ventricle (trabeculated), associated with morphologically tricuspid AV valve in left position in continuity with the aortic valve and thoracic aorta (Figures 2 and 3). |
| Insertion of a morphologically tricuspid AV valve in left position lower than or in the same plane as the AV valve in right position (Figure 4). |
| Morphologically left ventricle (without infundibulum), associated with an atrium receiving two venae cavae. In the present case, the course of the lead can be seen in both chambers (Figure 5). |
AV: atrioventricular.
The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Cardoso G, Abecasis J, Ribeiras R, et al. Transposição de grandes vasos congenitamente corrigida e endocardite de electrocateter. Rev Port Cardiol. 2014;33:577–579.