Assessment of coronary lesions by the instantaneous wave free ratio (iFR) has generated significant debate. We aimed to assess the diagnostic performance of iFR and its impact on the decision to use fractional flow reserve (FFR) and on procedural characteristics.
MethodsIn this single-center registry of patients undergoing functional assessment of coronary lesions, FFR was used as a reference for assessing the diagnostic performance of iFR. An iFR value <0.86 was considered positive and a value >0.93 was considered negative.
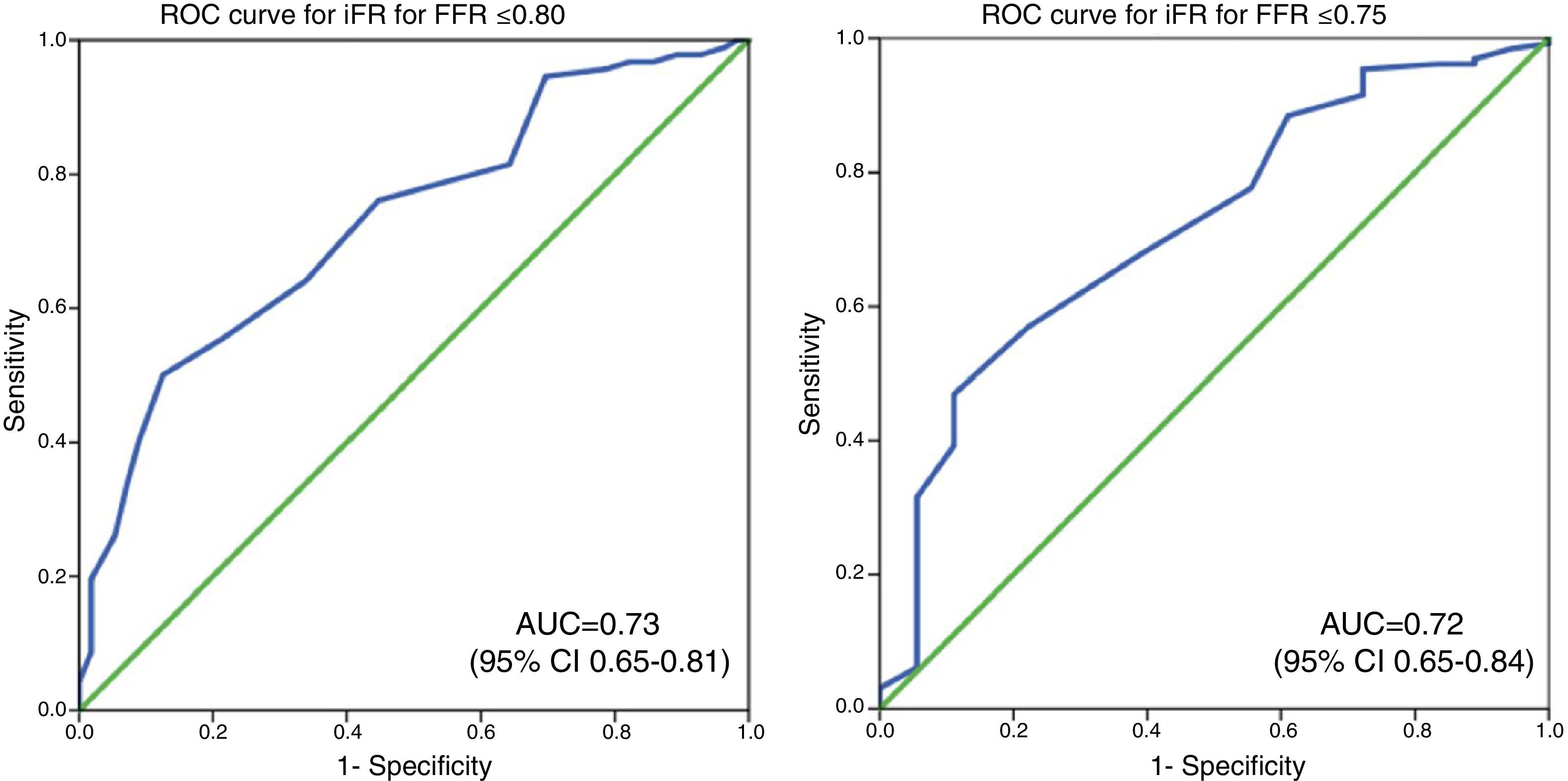
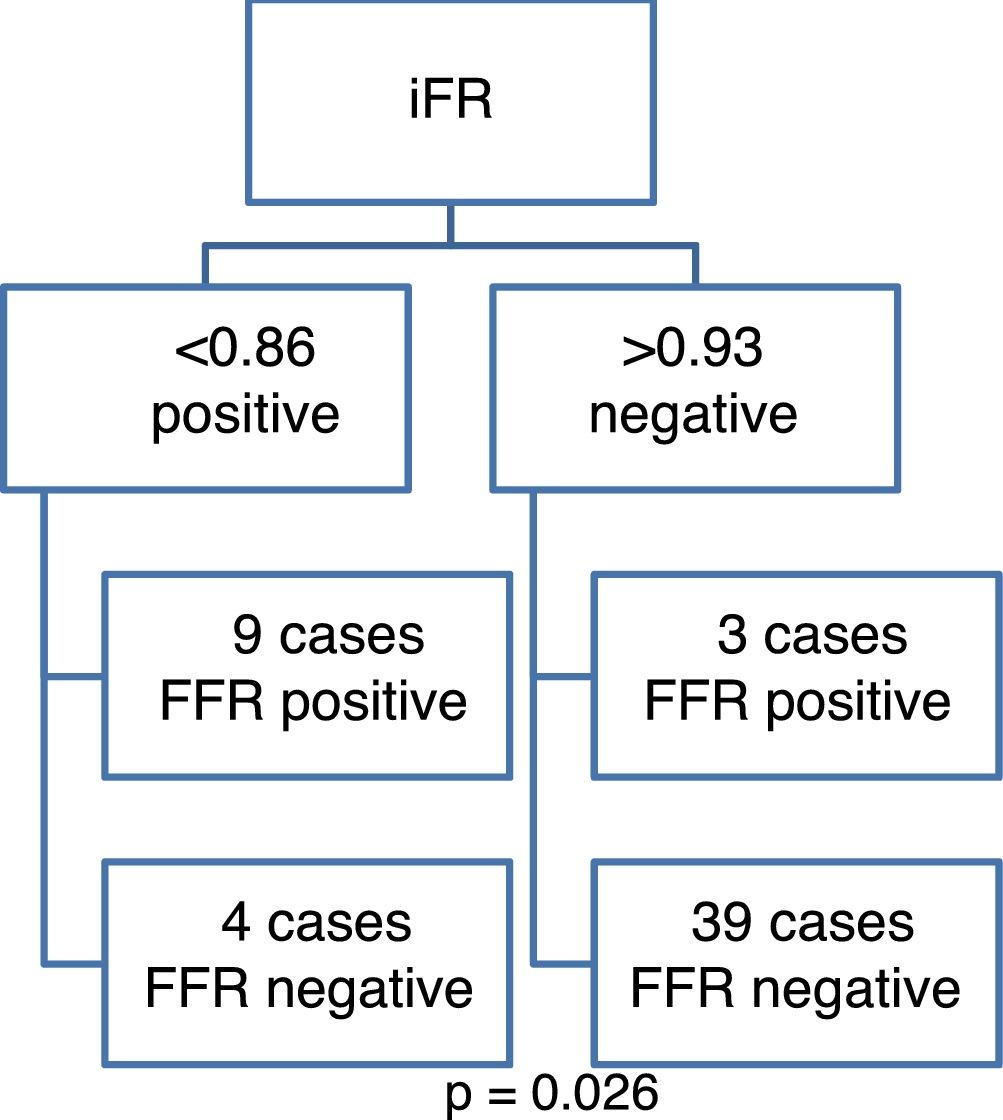
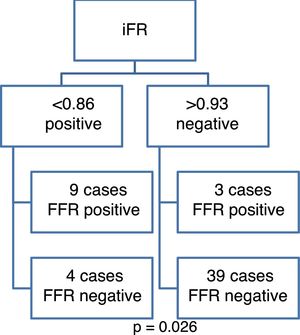
ResultsFunctional testing was undertaken of 402 lesions, of which 154 were assessed with both techniques, 222 with FFR only, and 26 with iFR only. Using a cut-off of ≤0.80 for iFR, the area under the curve was 0.73 (95% CI 0.65-0.81), with an optimal value of ≤0.91. FFR was undertaken in 93 out of 94 lesions with an inconclusive iFR and was performed in 69.1% of the remaining iFR-tested lesions. Concordance between iFR and FFR was 87% (chi-square=22.43; p<0.001). Notwithstanding, there were four out of 13 cases (30.7%) of positive iFR with negative FFR and three out of 42 (7.1%) cases of negative iFR and positive FFR. This difference was significant (p=0.026). iFR had no impact on procedure time, fluoroscopy time or radiation dose.
ConclusioniFR had a reasonable diagnostic performance. Operators often chose to perform FFR despite conclusive iFR results. iFR and FFR were highly concordant, but a non-negligible proportion of lesions classified as ischemic by iFR were classified as non-ischemic by FFR. iFR had no impact on procedural characteristics.
A avaliação de lesões coronárias pelo instantaneous wave free ratio (iFR) tem gerado debate. Pretendeu-se analisar o desempenho diagnóstico do iFR e o seu impacto na decisão de utilizar o fractional flow reserve (FFR) e nas características do procedimento.
MétodosRegisto unicêntrico de doentes submetidos a avaliação funcional de lesões coronárias. O desempenho do iFR foi aferido utilizando o FFR como referência. Valores de iFR < 0,86 e > 0,93 foram considerados positivos e negativos, respetivamente.
Resultadosavaliaram-se 402 lesões, em 154 casos com ambas as técnicas, em 222 apenas com FFR e 26 apenas com iFR. Utilizando um limiar de FFR ≤ 0,80, a área sob a curva foi de 0,73 (95% IC 0,65-0,81) - valor ótimo de iFR ≤ 0,91. Efetuou-se FFR em 93 de 94 lesões inconclusivas por iFR e em 69,1% dos restantes casos aferidos com iFR. O iFR e o FFR foram concordantes em 87% dos casos (X2=22,43; p<0,001). Não obstante, verificaram-se 4 em 13 casos (30,7%) de iFR positivo e FFR negativo, e 3 em 42 casos (7,1%) de iFR negativo e FFR positivo. Esta diferença foi estatisticamente significativa (p=0,026). O iFR não teve impacto na duração, dose/tempo de radiação do procedimento.
ConclusõesO desempenho diagnóstico do iFR foi razoável. Os operadores habitualmente efetuaram FFR apesar de valores conclusivos de iFR. Verificou-se elevada concordância, mas com uma proporção não negligenciável de lesões classificadas como isquémicas por iFR e não isquémicas por FFR. O iFR não teve impacto nas características do procedimento.
Functional assessment of coronary lesions by fractional flow reserve (FFR) is common practice in percutaneous coronary intervention (PCI) and is formally recommended in the European guidelines.1 Various studies have shown that the use of FFR to guide decision-making helps detect cases in which it is safe not to perform PCI.2–4 A Portuguese multicenter registry recently obtained similar results.5 Nevertheless, there is still no absolute consensus regarding the ideal FFR cutoff for deciding whether to perform PCI. Most trials use a cutoff of ≤0.80,2,3 but the study with the longest follow-up used a value of <0.75 to proceed with PCI.4
In recent years, a new functional assessment technique – the instantaneous wave-free ratio (iFR) – has emerged as an alternative to FFR. Its advantages are that it does not require drugs such as adenosine, and results can be obtained more rapidly than with FFR.6 Various studies have indicated good concordance between iFR and FFR.7,8 Two recent randomized multicenter clinical trials demonstrated the non-inferiority of iFR compared to FFR with regard to outcomes for deciding whether to perform PCI, using a cutoff of ≤0.89 for iFR as an indication to perform the procedure.9,10 Other trials have examined a hybrid strategy, in which PCI is performed with iFR <0.86, a conservative approach is adopted for >0.93, and assessment by FFR is carried out in cases with values between these cutoffs.7 However, there is no consensus regarding the use of iFR only, nor on how to interpret its results.11 FFR is still considered the gold standard for the functional assessment of coronary lesions, including in international guidelines.1,11
We therefore set out to analyze the results of a registry on the use of iFR and FFR to determine (1) the diagnostic accuracy of iFR using FFR as a reference, (2) the effect of using iFR initially on the decision to perform FFR at the discretion of the operator, (3) the degree of concordance between the two techniques, and (4) the effect of using iFR on fluoroscopy time, radiation dose and procedure time.
MethodsStudy characteristicsThis was a single-center registry of all patients who underwent coronary angiography with functional assessment of coronary lesions by FFR and/or iFR over a five-year period (2012-2016). Whether to perform FFR, iFR or both was left to the operator's discretion, as was the decision whether to proceed to revascularization or medical treatment. Patients enrolled in clinical trials involving these techniques were excluded, since they were subject to specific protocols that did not rely on the operator's decision. Demographic, clinical and procedural characteristics were recorded prospectively, including FFR and iFR measurements and their results. This study is a retrospective analysis, since it focused mainly on the subgroup who underwent both measurements, and the registry was not created specifically for the purpose of comparing the two groups.
Measurement of fractional flow reserve and instantaneous wave-free ratioFFR was measured after maximum hyperemia was obtained by central venous administration of adenosine (140 μg/kg/min), using St. Jude Medical (now Abbot) or Volcano (now Philips Volcano) systems. The latter (console and other equipment) was used in all cases when iFR was measured alone or jointly with FFR.
Statistical analysisReceiver operating characteristic curve analysis was used to identify the iFR value with the best diagnostic accuracy, using FFR as a reference with cutoffs of ≤0.80 and <0.75. Bland-Altman plots and Pearson's correlation were used to compare iFR and FFR values.
iFR results were also compared according to the hybrid strategy,7 in which a value between 0.86 and 0.93 was considered inconclusive, <0.86 was considered positive (indicating ischemia and therefore PCI), and >0.93 was considered negative (indicating absence of ischemia, and hence deferral of the procedure). The same assessment was carried out using a cutoff of ≤0.89 in accordance with two recent randomized trials.9,12 Both analyses used a cutoff of ≤0.80 for FFR as a reference.
Finally, the effect of iFR on fluoroscopy time, radiation dose, procedure time and use of adenosine was analyzed.
The Student's t test was used to compare quantitative variables and the chi-square test was used to compare qualitative variables. Values are presented as mean ± standard deviation (SD).
ResultsPopulation and procedural characteristicsOver a five-year period, 326 patients (mean age 67±11 years, 68.7% male) underwent functional assessment of moderate coronary lesions.
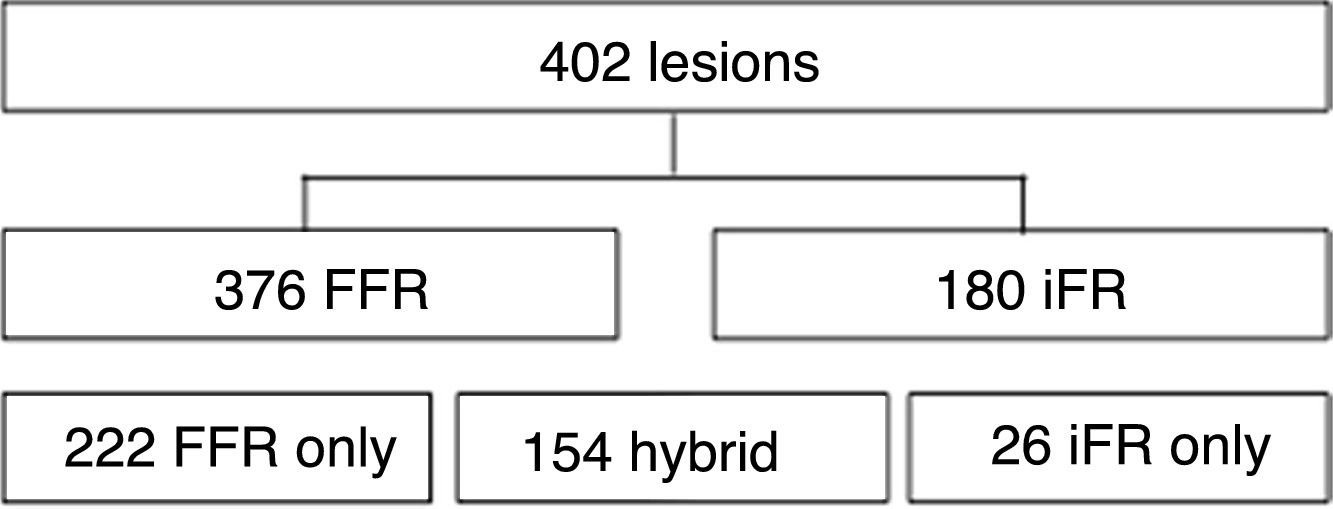
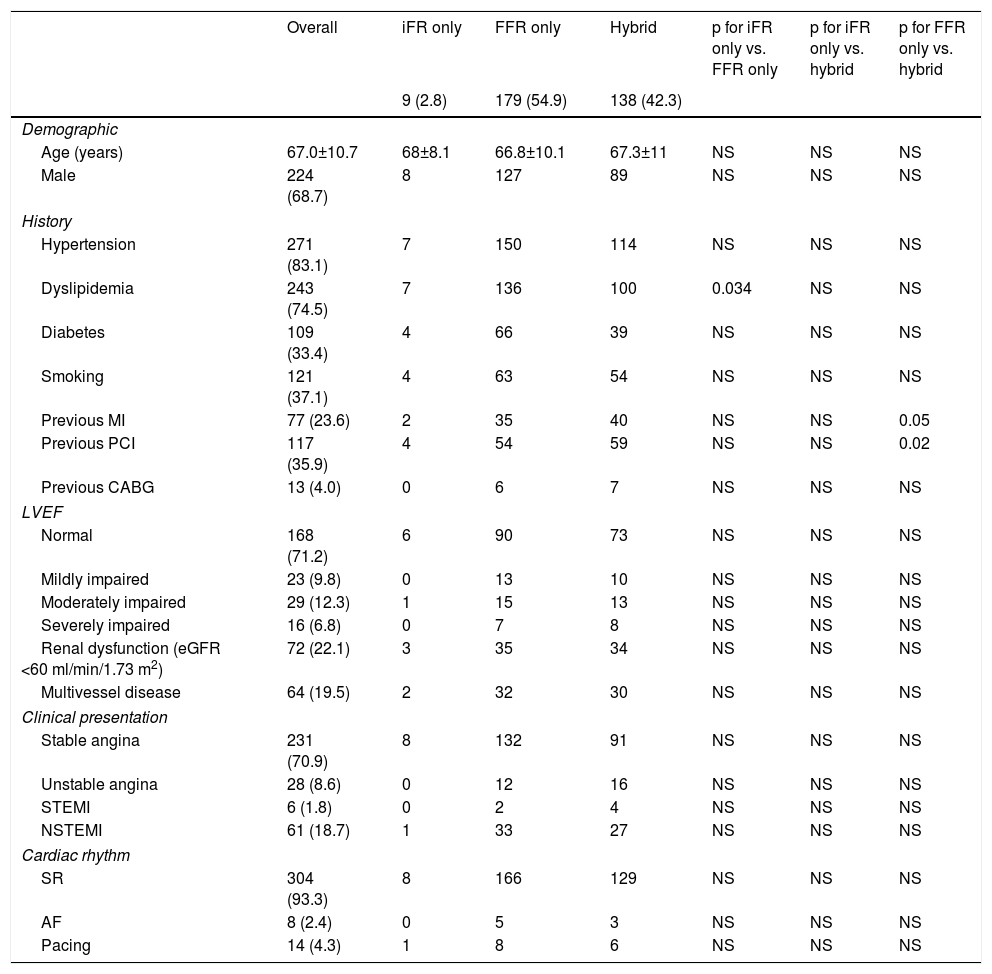
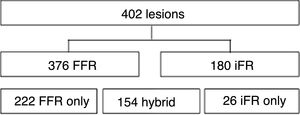
Measurements were taken for 402 lesions. FFR was used to assess 376 (93.5%) lesions and iFR to assess 180 (44.8%), with FFR only used in 222 lesion (55.2%) and iFR only in 26 lesion (6.5%) (Figure 1). There were no complications arising from adenosine use. Table 1 summarizes the main demographic and clinical characteristics of the patients in the overall population and according to the use of FFR, iFR or both techniques. There was a higher prevalence of dyslipidemia in the iFR-only group than in the FFR-only group, and a higher prevalence of previous history of myocardial infarction (almost reaching statistical significance, p=0.05) and previous PCI (p=0.034) in the FFR-only group vs. the group in which both techniques were used. There were no other significant differences between the groups.
Baseline characteristics of the study population (n=326).
| Overall | iFR only | FFR only | Hybrid | p for iFR only vs. FFR only | p for iFR only vs. hybrid | p for FFR only vs. hybrid | |
|---|---|---|---|---|---|---|---|
| 9 (2.8) | 179 (54.9) | 138 (42.3) | |||||
| Demographic | |||||||
| Age (years) | 67.0±10.7 | 68±8.1 | 66.8±10.1 | 67.3±11 | NS | NS | NS |
| Male | 224 (68.7) | 8 | 127 | 89 | NS | NS | NS |
| History | |||||||
| Hypertension | 271 (83.1) | 7 | 150 | 114 | NS | NS | NS |
| Dyslipidemia | 243 (74.5) | 7 | 136 | 100 | 0.034 | NS | NS |
| Diabetes | 109 (33.4) | 4 | 66 | 39 | NS | NS | NS |
| Smoking | 121 (37.1) | 4 | 63 | 54 | NS | NS | NS |
| Previous MI | 77 (23.6) | 2 | 35 | 40 | NS | NS | 0.05 |
| Previous PCI | 117 (35.9) | 4 | 54 | 59 | NS | NS | 0.02 |
| Previous CABG | 13 (4.0) | 0 | 6 | 7 | NS | NS | NS |
| LVEF | |||||||
| Normal | 168 (71.2) | 6 | 90 | 73 | NS | NS | NS |
| Mildly impaired | 23 (9.8) | 0 | 13 | 10 | NS | NS | NS |
| Moderately impaired | 29 (12.3) | 1 | 15 | 13 | NS | NS | NS |
| Severely impaired | 16 (6.8) | 0 | 7 | 8 | NS | NS | NS |
| Renal dysfunction (eGFR <60 ml/min/1.73 m2) | 72 (22.1) | 3 | 35 | 34 | NS | NS | NS |
| Multivessel disease | 64 (19.5) | 2 | 32 | 30 | NS | NS | NS |
| Clinical presentation | |||||||
| Stable angina | 231 (70.9) | 8 | 132 | 91 | NS | NS | NS |
| Unstable angina | 28 (8.6) | 0 | 12 | 16 | NS | NS | NS |
| STEMI | 6 (1.8) | 0 | 2 | 4 | NS | NS | NS |
| NSTEMI | 61 (18.7) | 1 | 33 | 27 | NS | NS | NS |
| Cardiac rhythm | |||||||
| SR | 304 (93.3) | 8 | 166 | 129 | NS | NS | NS |
| AF | 8 (2.4) | 0 | 5 | 3 | NS | NS | NS |
| Pacing | 14 (4.3) | 1 | 8 | 6 | NS | NS | NS |
Values are mean ± SD or n (%).
AF: atrial fibrillation; CABG: coronary artery bypass grafting; eGFR: estimated glomerular filtration rate; LVEF: left ventricular ejection fraction; MI: myocardial infarction; NSTEMI: non-ST-elevation myocardial infarction; PCI: percutaneous coronary intervention; SR: sinus rhythm; STEMI: ST-elevation myocardial infarction.
In cases of non-ST-elevation acute coronary syndrome, the measurements taken were of non-culprit lesions and were performed 48-72 hours after symptom onset, while in ST-elevation acute coronary syndrome, six non-culprit lesions were assessed, all during the acute phase. Four of these assessments used both techniques and two used FFR only, with the FFR result used for decision-making. Of the four iFR measurements, three lesions had iFR 0.9 (two cases with positive and one with negative FFR), and the fourth had iFR 0.88 (FFR 0.81).
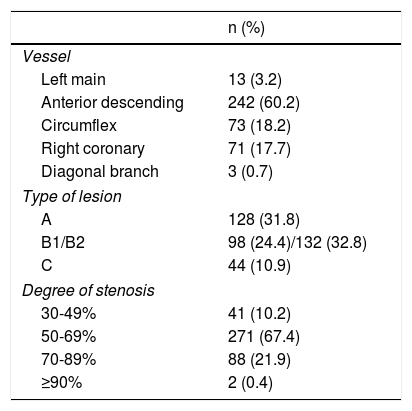
Table 2 shows the characteristics of the lesions assessed.
Characteristics of the coronary lesion assessed (n=402).
| n (%) | |
|---|---|
| Vessel | |
| Left main | 13 (3.2) |
| Anterior descending | 242 (60.2) |
| Circumflex | 73 (18.2) |
| Right coronary | 71 (17.7) |
| Diagonal branch | 3 (0.7) |
| Type of lesion | |
| A | 128 (31.8) |
| B1/B2 | 98 (24.4)/132 (32.8) |
| C | 44 (10.9) |
| Degree of stenosis | |
| 30-49% | 41 (10.2) |
| 50-69% | 271 (67.4) |
| 70-89% | 88 (21.9) |
| ≥90% | 2 (0.4) |
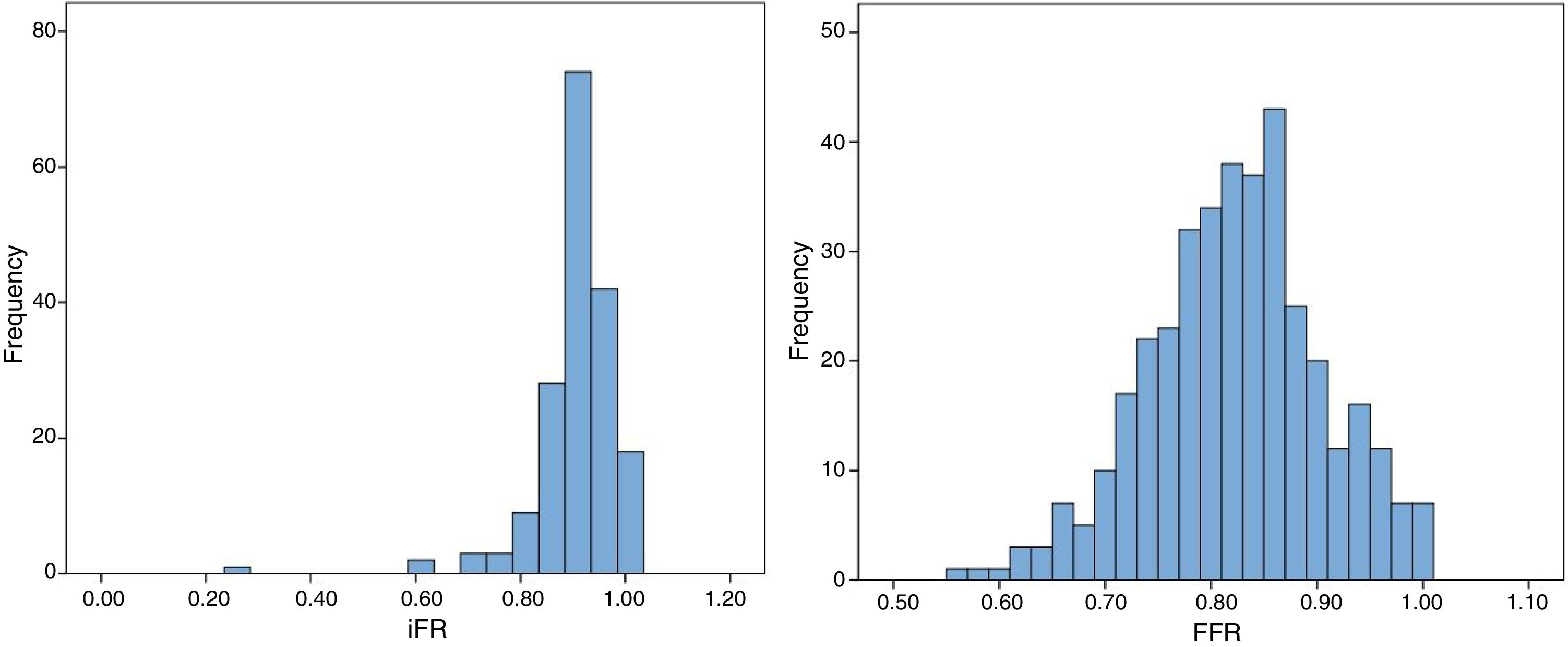
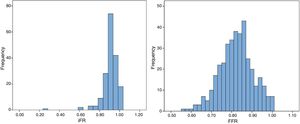
Mean iFR was 0.90±0.1, and was >0.93 in 60 cases (33.3% of all measurements) and <0.86 in 21 cases (11.7% of all measurements). In the iFR-only subgroup, all values were <0.86 or >0.93, so calculating the mean and SD does not represent its true distribution (iFR-only was the only subgroup without a normal distribution); when both techniques were used, mean iFR was 0.9±0.05. Mean FFR in the overall population was 0.82±0.08. No statistically significant differences were found between mean FFR for FFR-only cases (0.81±0.09) and cases in which both techniques were used (0.82±0.07). Figure 2 shows the distribution of overall iFR and FFR values.
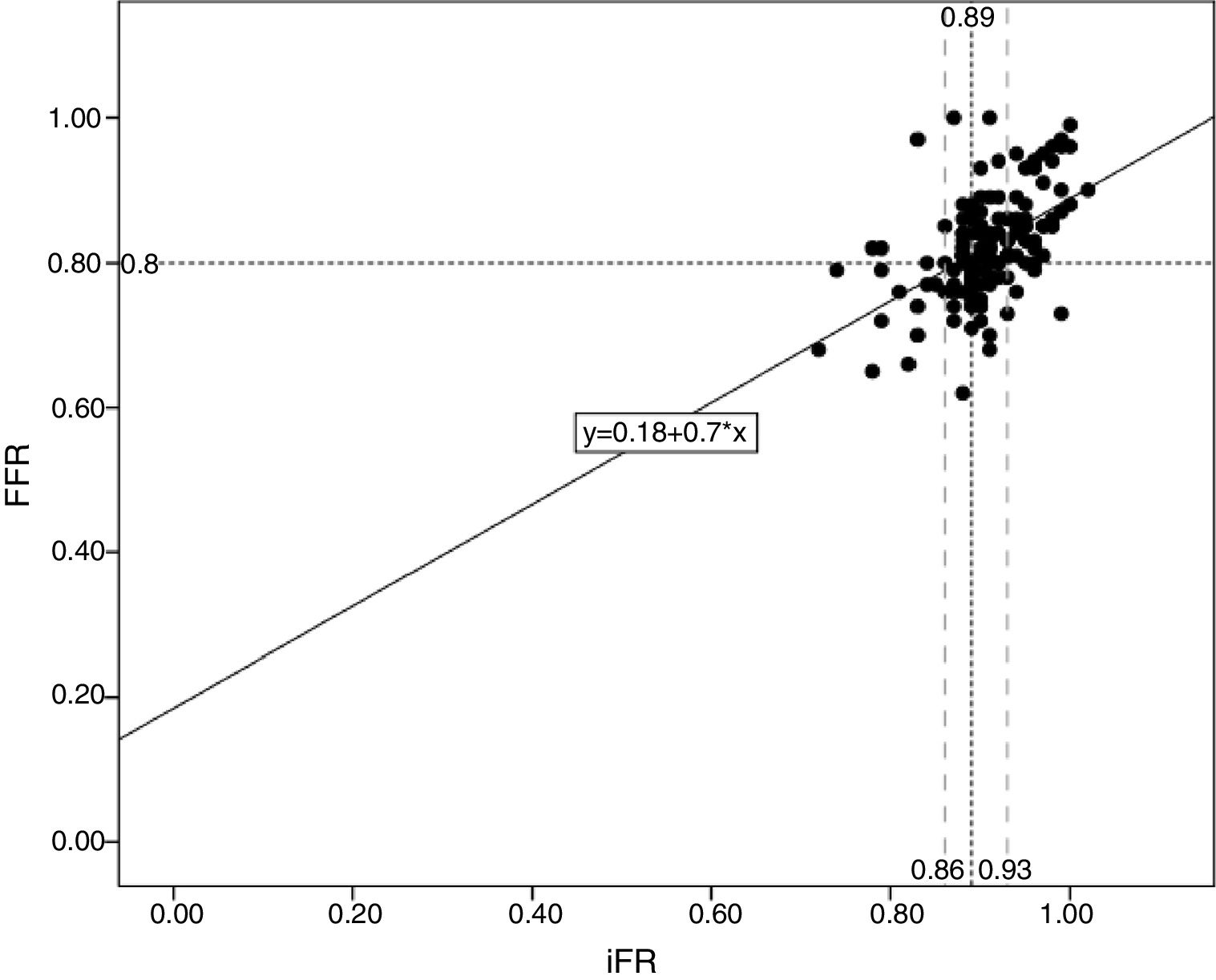
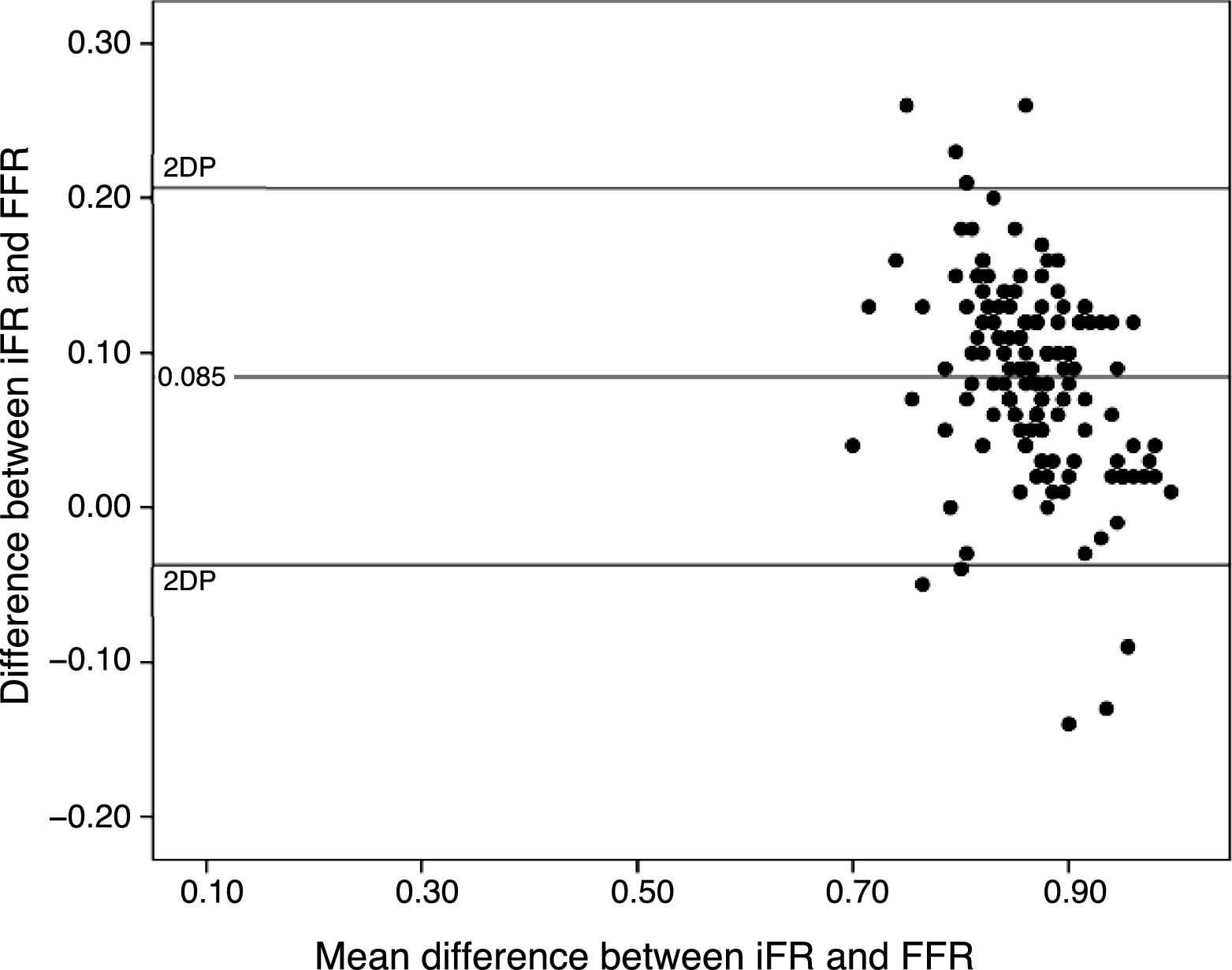
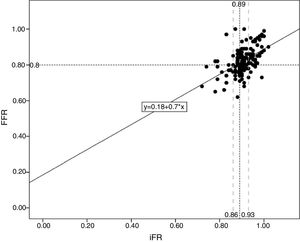
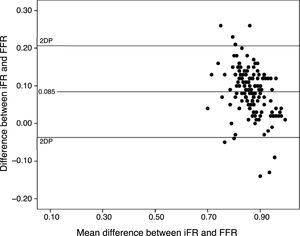
A moderately significant correlation was found between iFR and FFR (R=0.504; p<0.001) (Figure 3), as shown in the scatter plot. Bland-Altman analysis showed good concordance (the mean difference between iFR and FFR was 0.085±0.062) (Figure 4).
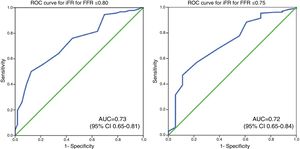
In terms of diagnostic accuracy, the area under the curve (AUC) of iFR was 0.73 (95% CI: 0.65-0.81) and 0.72 (95% CI: 0.60-0.84), using cutoffs of ≤0.80 and <0.75, respectively, for FFR as reference (Figure 5).
The optimal iFR cutoff was found to be ≤0.91 for both FFR ≤0.80 (55% sensitivity, 79% specificity, 52% positive predictive value, 81% negative predictive value) and FFR <0.75 (47% sensitivity, 89% specificity, 19% positive predictive value, 97% negative predictive value). In addition, for FFR ≤0.80, the iFR range with sensitivity and specificity >90% was 0.88-0.94, and for FFR ≤0.75 it was 0.87-0.95.
Effect of instantaneous wave-free ratio measurements on the decision to measure fractional flow reserve and concordance of resultsAn iFR between 0.86 and 0.93 was strongly associated with the decision to perform FFR (chi-square=30.1; p<0.001), which occurred in 93 out of 94 cases. When iFR was not within this range, the decision to assess the lesion by FFR was made in 55 cases (69.1%). No differences were found in the decision to perform FFR in this subgroup between iFR results of <0.86 vs. >0.93 (71.4% vs. 68%; p=0.792). In these cases, a statistically significant concordance of 87.3% was found between iFR and FFR results (chi-square=22.43; p<0.001). However, there was discordance between the two methods in four out of 13 (30.8%) cases of positive iFR with negative FFR, and in three out of 42 (7.1%) cases with negative iFR and positive FFR. This difference was statistically significant (p=0.026) (Figure 6).
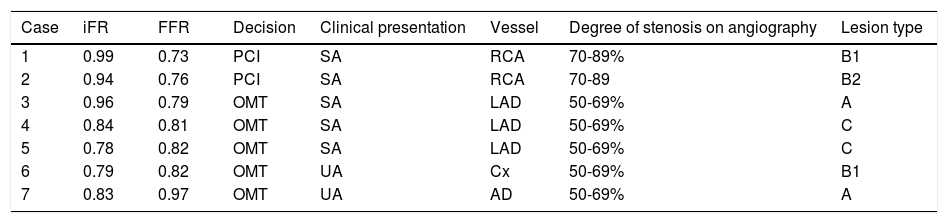
These discrepancies are detailed in Table 3. Four of them were in measurements of the left anterior descending artery (16% of a total of 25 measurements in this artery), two in the right coronary artery (14% of 14 measurements) and one in the circumflex artery (6.7% of 15 measurements). There was only one measurement using both techniques in the left main, with no discordance. As can be seen, in cases of negative iFR and positive FFR, the operators chose to follow the FFR indication when the measurement was clearly less than 0.80. In case 3, the presence of a borderline value led the operator to defer the procedure. In cases of positive iFR, the operators followed the indication given by FFR.
Characterization of discordances between results of instantaneous wave-free ratio and fractional flow reserve.
| Case | iFR | FFR | Decision | Clinical presentation | Vessel | Degree of stenosis on angiography | Lesion type |
|---|---|---|---|---|---|---|---|
| 1 | 0.99 | 0.73 | PCI | SA | RCA | 70-89% | B1 |
| 2 | 0.94 | 0.76 | PCI | SA | RCA | 70-89 | B2 |
| 3 | 0.96 | 0.79 | OMT | SA | LAD | 50-69% | A |
| 4 | 0.84 | 0.81 | OMT | SA | LAD | 50-69% | C |
| 5 | 0.78 | 0.82 | OMT | SA | LAD | 50-69% | C |
| 6 | 0.79 | 0.82 | OMT | UA | Cx | 50-69% | B1 |
| 7 | 0.83 | 0.97 | OMT | UA | AD | 50-69% | A |
LAD: left anterior descending artery; CX: circumflex artery; FFR: fractional flow reserve; iFR: instantaneous wave-free ratio; OMT: optimal medical therapy; PCI: percutaneous coronary intervention; RCA: right coronary artery; SA: stable angina; UA: unstable angina.
Using an iFR cutoff of 0.89, 56 lesions (36.4%) were positive (≤0.89) and 98 (73.6%) were negative (>0.89). A statistically significant concordance of 72.1% (p<0.001) was found between the two techniques, while no significant differences were found between cases of positive iFR with negative FFR (20 out of 43 cases; 46.5%) and negative iFR with positive FFR (23 out of 43 cases; 53.5%).
Results of the assessment and treatment decisionsThe decision whether to proceed with revascularization was taken by each operator individually for each patient.
In the 26 cases in which iFR only was performed, all values were outside the gray area (seven cases <0.86, all others >0.93), and the decision on revascularization was made according to the iFR result.
When FFR only was performed, the treatment decision was made according to the FFR result (cutoff 0.80) in 97.7% of cases. In the other 2.3%, the operator decided not to act on the FFR value due to other relevant data, such as lesion characteristics, symptoms, or results of non-invasive ischemia tests.
When both techniques were performed, the operators followed the results whenever there was concordance between the two techniques. Cases in which there was discordance are described above (Table 3).
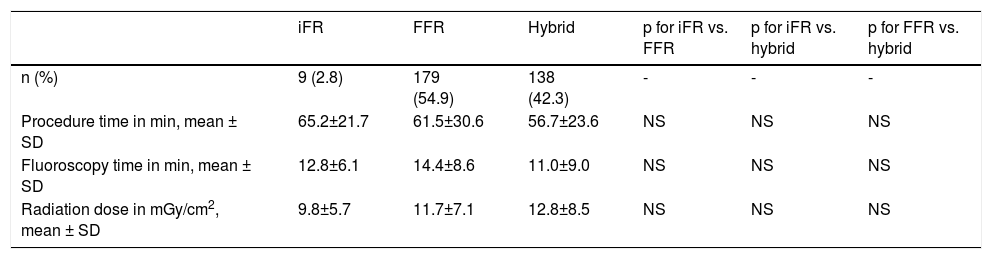
Effects of the method used on fluoroscopy time, radiation dose and procedure timeNo statistically significant differences were found in fluoroscopy time, radiation dose or procedure time between patients who underwent iFR only and those who underwent FFR only, or between those who underwent both iFR and FFR and those who underwent only one technique (Table 4).
Overall procedure characteristics according to the assessment method used (n=402).
| iFR | FFR | Hybrid | p for iFR vs. FFR | p for iFR vs. hybrid | p for FFR vs. hybrid | |
|---|---|---|---|---|---|---|
| n (%) | 9 (2.8) | 179 (54.9) | 138 (42.3) | - | - | - |
| Procedure time in min, mean ± SD | 65.2±21.7 | 61.5±30.6 | 56.7±23.6 | NS | NS | NS |
| Fluoroscopy time in min, mean ± SD | 12.8±6.1 | 14.4±8.6 | 11.0±9.0 | NS | NS | NS |
| Radiation dose in mGy/cm2, mean ± SD | 9.8±5.7 | 11.7±7.1 | 12.8±8.5 | NS | NS | NS |
FFR: fractional flow reserve; iFR: instantaneous wave-free ratio; SD: standard deviation.
Considering only patients who underwent iFR only or both iFR and FFR (a total of 147), 55 (37.4%) of them had all lesions assessed and had a conclusive iFR measurement (outside of the 0.86-0.93 range). With the hybrid strategy, the use of adenosine in these patients would have been avoided.
DiscussionPerformance of instantaneous wave-free ratio with fractional flow reserve as the gold standardIn this registry, iFR showed reasonable diagnostic accuracy and concordance with FFR, although there were some differences from previous publications. The best cutoff in this sample was slightly higher than that published in other studies (0.91 vs. 0.897,13), regardless of the FFR value used as standard. In addition, its diagnostic accuracy was inferior to that of some other studies, in which the AUC ranged from 0.86 to 0.90,7,13,14 but better than in the VERIFY study.15 The correlation between iFR and FFR was also lower than in previous studies (0.504, compared to 0.81 in ADVISE II7). These results may reflect a sample-size effect, since our population was smaller than in the other studies, or selection bias, since the study was based on a registry. Operators may have chosen to use both measurements in particularly borderline cases, as can be seen by the fact that the mean iFR value was very similar to the diagnostic value used in DEFINE-FLAIR9 and iFR-SWEDEHEART12 (0.89). Furthermore, when iFR was performed first and the result was then confirmed using FFR, not only was the value borderline, the SD was also very small (0.05).
Concordance between instantaneous wave-free ratio and fractional flow reserve and implications for daily practiceWhen the hybrid strategy was used, iFR showed high concordance within the diagnostic range (<0.86 and >0.93). This is similar to the results of the study by Escaned et al. that properly classified 91.6% of stenoses,7 which was slightly higher than in our case (87%). When a cutoff of 0.89 was used, the degree of concordance was also lower than in Escaned et al. (72.1% vs. 82.5%7), because this cutoff did not have the highest diagnostic accuracy in this sample (which limits the extent to which this result can be generalized), as well as the above-mentioned limitations.
Notwithstanding the good results from the hybrid approach in this registry, the degree of discrepancy between the two techniques was not negligible. When iFR and FFR gave different indications, operators tended to follow current international guidelines1 and use FFR as the gold standard. Discordance predominantly involved positive iFR and negative FFR, as in other studies.7 Thus, it may particularly important for the operator to proceed with FFR in borderline cases, especially when iFR is positive.
The recently published results of DEFINE-FLAIR9 and iFR-SWEDEHEART10 have for the first time provided solid evidence in favor of decision-making based only on iFR ≤0.89. At the same time, despite the unfavorable results of the FUTURE trial,16 the experience gained with FFR and the extensive literature on this technique cannot be ignored. Thus, if there are to be large multicenter randomized trials on the use of both techniques, two key issues must be addressed: what to do if the FFR and iFR results do not agree, and whether only one of the techniques should be used and, if so, which.
In the absence of agreement on the answers to these questions, certain points should be taken into consideration in order to arrive at the best decision in each case.
Firstly, the operator must ensure that the technique is performed correctly, with appropriate caliber, type and positioning of the catheter, to avoid attenuation or distortion of the pressure curves, and that pressures are correctly calibrated to ensure that the curves overlap in time and in quantity, synchronized with the electrocardiogram. Although both techniques are influenced by these factors, faults in execution may distort one measurement more or less than the other. For example, in iFR, failure to synchronize with the electrocardiogram can mean that the timing of the distal coronary pressure to aortic pressure ratio (Pd/Pa) reading is inaccurate, leading to non-diastolic or partially diastolic values being incorporated into the result. Another problem to consider is pressure drift; to correct this, the operator should confirm that the pressure curves overlap before ending the procedure and, if necessary, reposition the pressure wire proximally. Finally, it should be noted that the only iFR systems currently available are from Volcano Philips, and so all iFR measurements in our study were performed using this equipment; any measurement taken using other systems remains off-label. It should borne in mind that in our registry, the centers and all its operators were thoroughly experienced in the use of FFR, so we can assume that the error rate was low. Nevertheless, the possibility of inaccuracies in iFR measurements cannot be completely excluded, especially while the new technique was being introduced. Furthermore, although confirmation of the absence of pressure drift is routine practice at our site, no record was kept of this. Similarly, although measurements in which the electrocardiographic tracing was suboptimal were rejected and iFR was rarely used in patients with atrial fibrillation or flutter (in none of whom discordance between the two techniques was observed), the possibility that cardiac rhythm influenced some of the results cannot be completely ruled out.
Secondly, even if there are no technical failures, the physiology of what is being measured is relevant. Since FFR is dependent on maximal hyperemia, response can be affected by the drug used (some centers use vasodilators other than adenosine) and its administration route,17 the vasodilatory effect of the contrast itself,18 the presence of concomitant microcirculatory dysfunction,19,20 and adenosine's systemic vasodilatory effect. The response to the drug, at the level of both small and large coronary arteries as well as systemically, is also known to vary between individuals, especially in acute coronary syndrome.
Finally, it should be noted that steady-state FFR often does not match the nadir value, and so the former should be used,21 as in this registry. In our study, there were only five cases of discordance when the hybrid strategy was used in stable angina and two in acute coronary syndrome (both unstable angina), and so the clinical context likely had little effect on discordance.
The limitations governing the use of iFR should also be taken into account. Although iFR is not considered to be limited by hyperemia, Berry et al. dispute this and also claim that its diagnostic accuracy is lower than observed in other studies.15 In addition, recent randomized trials had few events and were non-inferiority studies in which the non-inferiority margin was relatively wide, as the authors acknowledged.9,10
Some authors suggest that the discrepancy between the two methods is greater in lesions involving the anterior descending artery,22 especially in its proximal segment.23 Given the low number of discordant findings in each vessel in our registry, it is not possible to draw conclusions about the effect of the vessels or segments involved. Even in the anterior descending, there were only four cases of discrepancy, a similar rate to that in the right coronary.
The results from our registry, together with findings in the literature, thus suggest that iFR and FFR are in fact complementary methods for the assessment of coronary lesions, and are not mutually exclusive. Initial assessment by iFR only appears to be the most sensible strategy, given its simplicity and speed of execution. However, the limitations of the above-mentioned studies suggest that caution is in order and that in doubtful cases operators should consider FFR as well. Concordance between the two values is a strong indicator when deciding whether to proceed with revascularization. Understanding the cause of any discrepancy is crucial in order to decide if one of the results is more valid for an individual lesion and patient. If the cause is unclear, the additional use of invasive and/or non-invasive imaging methods should be considered before reaching a final decision, especially as iFR and FFR have mainly been validated for stable coronary artery disease.
Effect of instantaneous wave-free ratio on fluoroscopy time, radiation dose and procedure timeIn addition to not requiring adenosine, one of the theoretical advantages of iFR is that it may reduce procedure time. However, there is little evidence in the literature to support this. Although the DEFINE-FLAIR study9 reported a significant reduction of 4 min 30 s min with iFR compared to FFR, the reduction was not significant in the iFR-SWEDEHEART study.10 As in the latter study, in our registry the technique did not affect this or other parameters (radiation dose and fluoroscopy time). This may be explained by the significant differences between the patients studied, with the operator opting for a simpler technique in more severe cases. Nevertheless, there were few statistically significant differences between the groups: absolute and relative differences were small and had little statistical significance or clinical relevance, and appeared to be unrelated to the operators’ decisions. In addition, few patients underwent iFR only, which also limits comparisons between groups. Furthermore, in each group, in some cases more than one lesion was assessed. This may have contributed to the numerical differences between the groups, although these were not statistically significant.
Finally, the apparent discrepancy (not statistically significant) between radiation dose and procedure time (longer procedure time but lower radiation dose in the iFR group) resulted from the use of different frame rates by different operators, so the radiation dose did not always correspond to the fluoroscopy duration. Between groups, it was found that longer fluoroscopy duration was not associated with increased radiation dose. This is why we opted to present data on both groups.
Effect of instantaneous wave-free ratio on adenosine useIn this registry, iFR was used at the operator's discretion, and especially in the early stages of its implementation, both techniques were commonly used, which resulted in a high rate of adenosine use. As pointed out in the Results section, if the hybrid strategy had been followed, the use of adenosine could have been avoided in almost 40% of patients. This figure is still lower than in other studies, particularly the ADVISE II study,7 in which the hybrid strategy led to 65.1% of patients not being administered adenosine. The difference between these figures is related to the observational nature of our study, in which there were no set criteria for selecting techniques, and which could have led to selection bias in cases with borderline iFR values.
LimitationsDifferences between the results of our study and of others may result partly from the study characteristics, as this was a registry and not a randomized clinical trial, and thus the decision to use iFR or FFR was entirely at the operator's discretion. Registries also do not have the same methodological rigor as clinical trials, and so some results may have been affected by technical failings, especially during the initial stage of implementation of the iFR technique, as mentioned above.
Furthermore, analysis using the cutoff of 0.89 proposed in DEFINE-FLAIR9 and iFR-SWEDEHEART10 was limited by the fact that this was not the cutoff with the best diagnostic accuracy in our study, due to the sample size and possible selection bias, as pointed out above.
Finally, patients with acute coronary syndrome were included, and this may have affected the results. However, measurements in patients with non-ST-elevation acute coronary syndrome were performed 48-72 hours after symptom onset, as in other studies,9,12 which makes it less likely that our results were affected. In patients with ST-elevation myocardial infarction (STEMI), six measurements were taken in the acute phase. Although there is a high level of evidence from a recent randomized trial in favor of FFR in this context,24 there is still no consensus on its use (during our registry, the only evidence in favor of FFR was observational and its advantages were only theoretical), and the use of iFR in STEMI remains off-label. Nevertheless, in our study the borderline results of iFR did not constitute cases of discordance according to the hybrid strategy. They were a very small proportion of the total sample in both absolute and relative terms, and the indication provided by FFR was always followed, not treating lesions for which intervention was not indicated (bearing in mind that FFR tends to underestimate lesion severity). We therefore do not consider that the cases of acute coronary syndrome significantly affected our results.
ConclusioniFR showed reasonable diagnostic accuracy and concordance with FFR, although not as good as in most other studies. The cut-offs with the best diagnostic accuracy were similar to those in the literature, although slightly higher. The use of an FFR cutoff of <0.75 instead of ≤0.80 had a negative impact, albeit a very small one, on the diagnostic performance of iFR.
iFR was frequently inconclusive when the hybrid strategy was applied. In conclusive cases, there was good concordance between iFR and FFR results. However, the proportion of cases of discordance was significant, especially in assessments classified as positive by iFR and negative by FFR.
The use of iFR did not have a significant effect on fluoroscopy time, radiation dose or procedure time, but it could have resulted in a significant reduction in the use of adenosine if the hybrid strategy had been applied.
Although iFR is simple to perform and useful, data from our registry suggest that its results should be interpreted with caution, and the use of FFR should not be completely abandoned. Both methods can in fact have significant gray areas in which interpretation of their results is ambiguous, so other invasive or non-invasive methods for assessing coronary artery disease should always be considered.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Nobre Menezes M, Francisco AR, Carrilho Ferreira P, Jorge C, Torres D, Cardoso P, et al. Análise comparativa do fractional flow reserve (FFR) e do instantaneous wave-free ratio (iFR): resultados de um registo de 5 anos. Rev Port Cardiol. 2018;37:511–520.