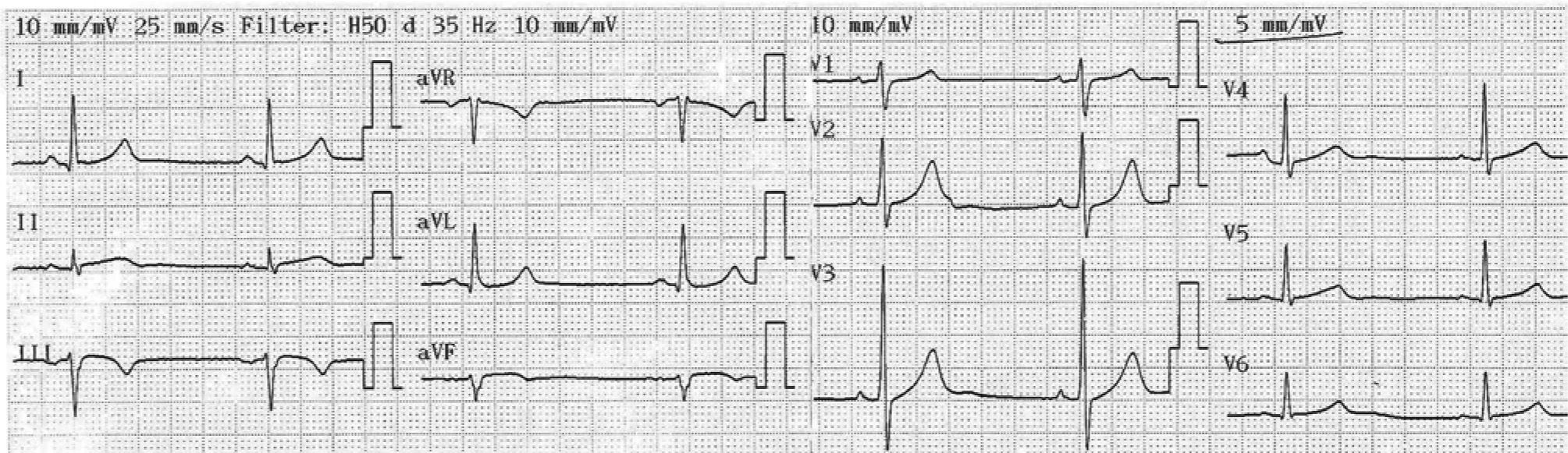
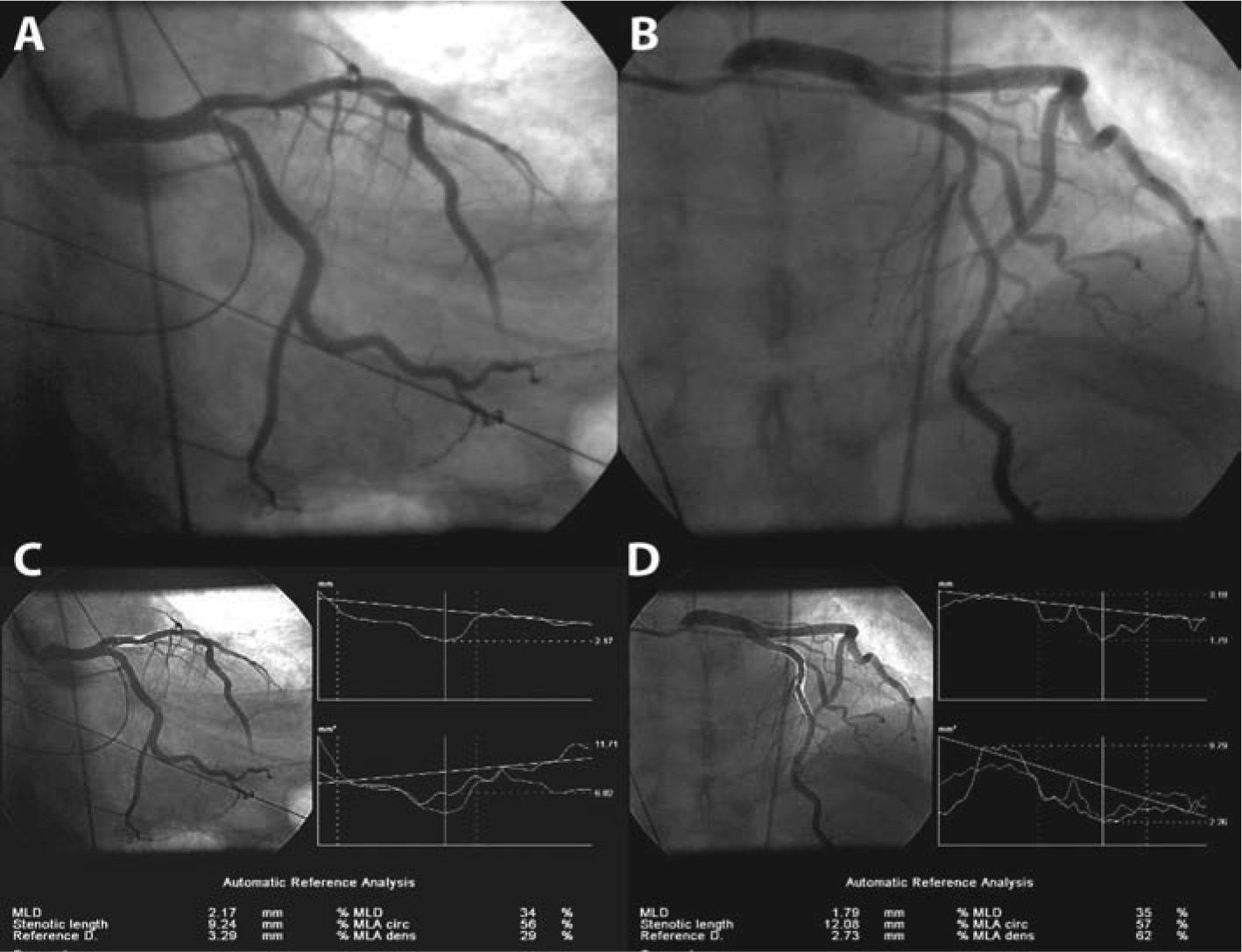
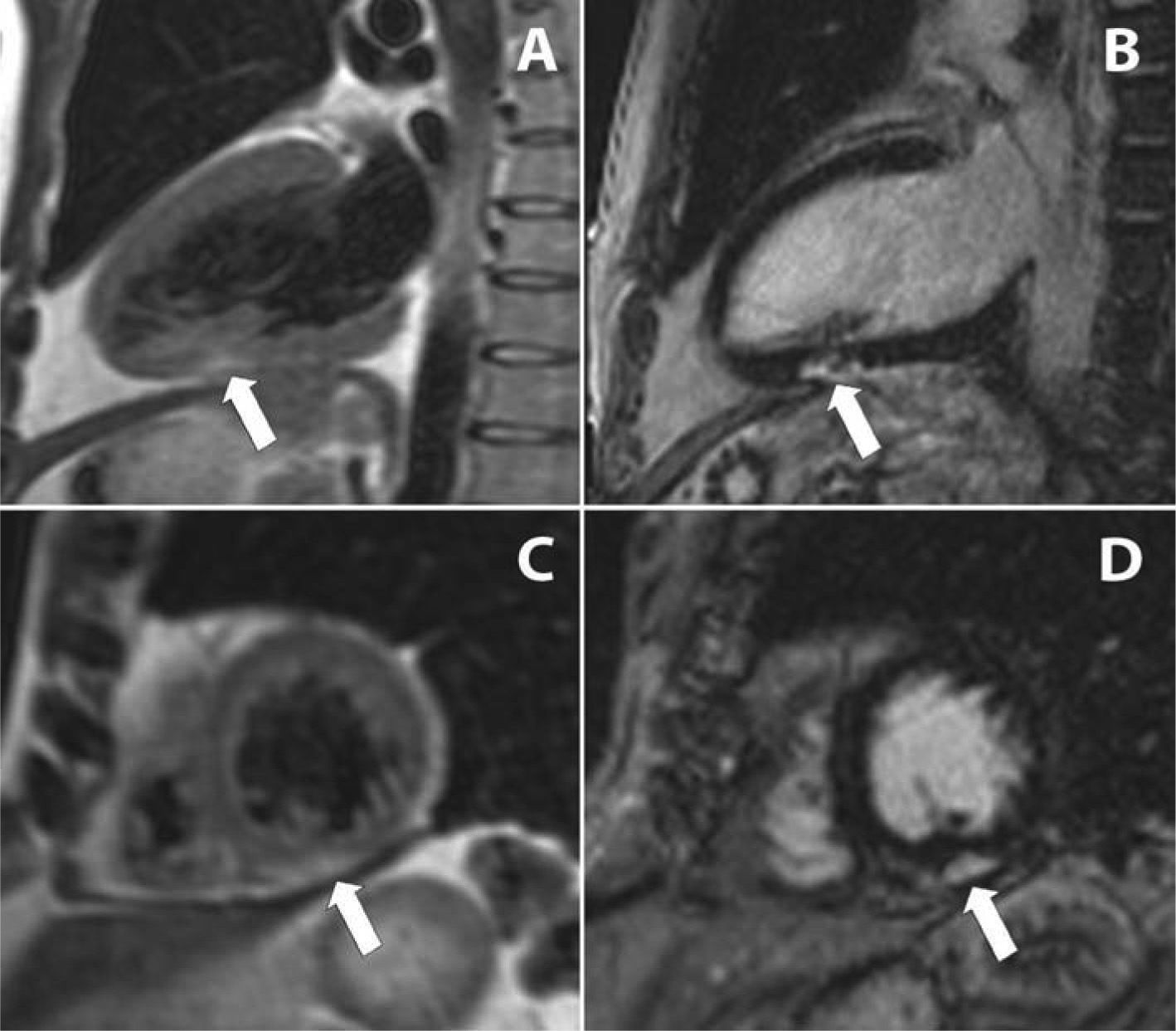
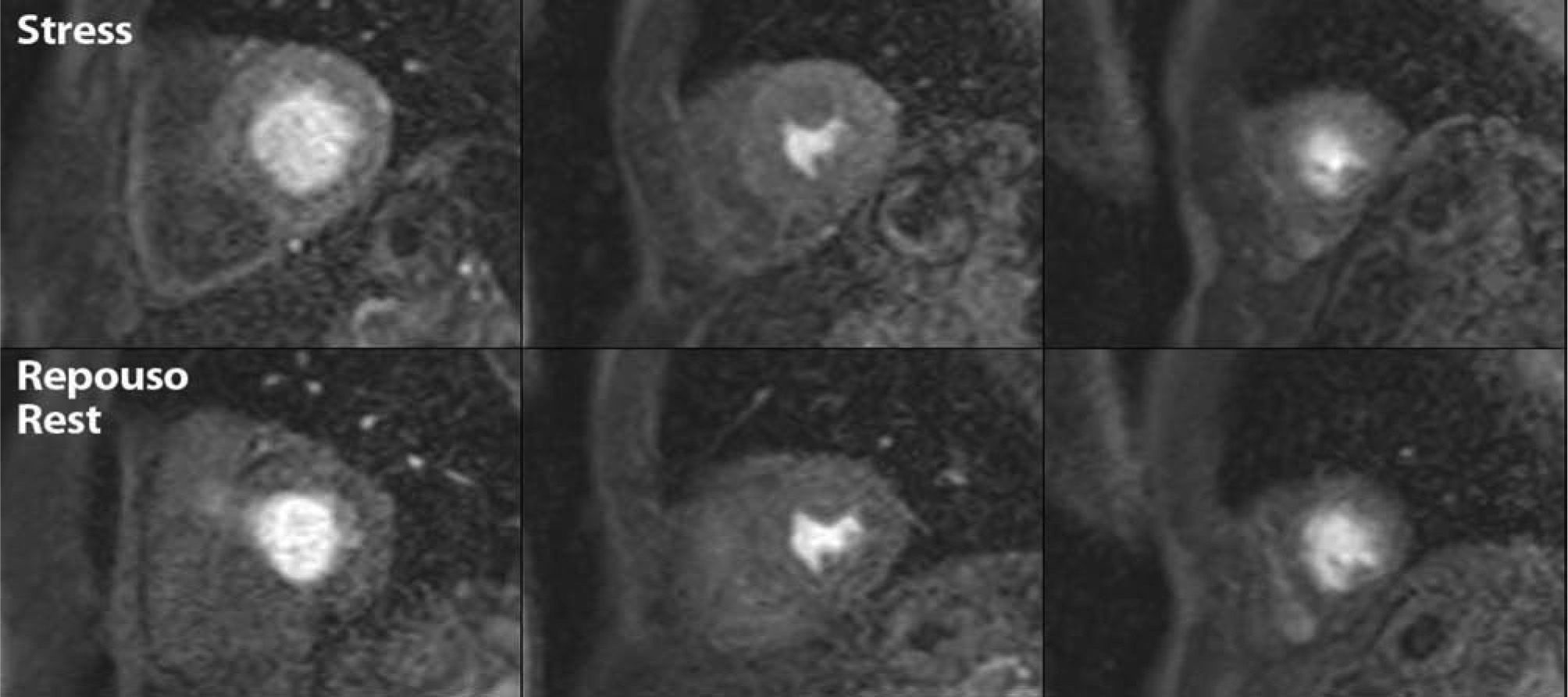
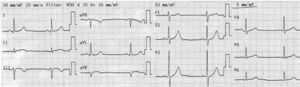
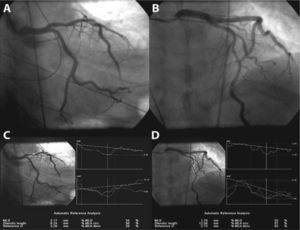
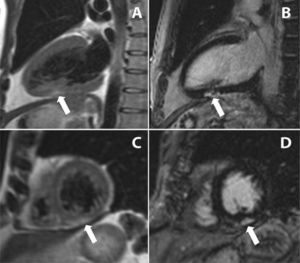
A 51-year-old man, hypercholesterolemic and an ex-smoker, was hospitalized for sudden-onset typical chest pain. The admission electrocardiogram showed slight ST-segment elevation with downward concavity in II, III and aVF (Figura 1). Urgent coronary angiography revealed a large caliber anterior descending artery, with a short proximal lesion and a long lesion in the mid segment, both with around 50% stenosis (Figura 2); there were no significant lesions in the left main, circumflex or right coronary arteries. Laboratory tests showed elevated biomarkers of myocardial necrosis (troponin 11.8μg/l, reference value <0.04μg/l). The echocardiogram showed good global and segmental left ventricular function. Stress cardiac magnetic resonance imaging (MRI) was requested, with a view to aiding differential diagnosis between myocardial infarction with spontaneous reperfusion and myopericarditis, as well as to assess the ischemic repercussions of the lesions in the anterior descending artery. This was performed on the sixth day of hospital stay, and showed focal subepicardial delayed enhancement at the transition between the mid and apical inferior segments, with a slightly increased T2 signal suggestive of edema at this point (Figura 3), and normal perfusion during the first pass of paramagnetic contrast under adenosine stress and at rest (Figura 4). A diagnosis of myocarditis was therefore made, given the absence of stress-induced ischemia. The lack of subendocardial delayed enhancement meant that infarction with spontaneous reperfusion could be definitively excluded. The patient was discharged one week after the acute event and has since remained asymptomatic.
A and C: T2-weighted turbo spin-echo sequences, 2-chamber (A) and short-axis (C) views, showing T2 hyperintense signal at the transition between the mid and apical inferior segments; B and D: same views in T1-weighted double inversion recovery sequences, showing subepicardial delayed enhancement at the same point.
Patients with chest pain and elevated troponin but no obstructive coronary disease present a diagnostic challenge. Possible causes include myocardial infarction with spontaneous reperfusion and acute myocarditis. Cardiac MRI can play an important role in differential diagnosis, detecting and characterizing myocardial delayed enhancement1. Subendocardial delayed enhancement with segmental distribution is highly sensitive and specific to myocardial infarction, reflecting the ischemic wave that occurs when a coronary artery is suddenly occluded2,3. By contrast, subepicardial delayed enhancement, as observed in the present case, suggests a non-ischemic mechanism and is usually found in cases of myocarditis4.
Cardiac MRI has high sensitivity and specificity in the investigation of ischemia through assessment of myocardial perfusion under pharmacological stress5. The diagnostic accuracy of this method appears to be similar or superior to that of myocardial perfusion scintigraphy6, and while little used in Portugal, stress MRI is one of the main indications for cardiac MRI in some European countries7.
The case presented illustrates the versatility of cardiac MRI, since a single exam can answer a variety of clinical questions that have therapeutic implications, thus precluding the need for further exams7.