The incidence and prevalence of hypertensive emergency have been little addressed in the literature. However, over the last decade increasing numbers of young patients with different forms of hypertensive crisis have been observed in emergency departments. We performed this study to ascertain the clinical and epidemiological characteristics of patients aged ≤45 years admitted with a diagnosis of hypertensive emergency.
MethodsWe conducted an observational, descriptive, cross‐sectional prospective study of 123 patients hospitalized for hypertensive emergency in the Hospital do Prenda, Luanda, between May 2011 and June 2012.
ResultsMean age was 36.62±5.49 years, and most were male (52.85%). The main risk factor was hypertension (65.9%), with 17.3% complying with therapy. The most frequent forms of presentation were hypertensive encephalopathy and hemorrhagic stroke (9.8% and 82.1%, respectively). The main drugs used were diuretics, angiotensin‐converting enzyme inhibitors and calcium channel blockers. Mortality during hospitalization was 25.2% (31 patients), hemorrhagic stroke being the most common cause. There was a significant association between age and in‐hospital mortality.
ConclusionsOf patients admitted with hypertensive emergency, 30.1% were aged ≤45 years. Hemorrhagic stroke was the most common presentation. There was a significant relationship between mode of presentation, age and in‐hospital mortality.
A incidência e prevalência da emergência hipertensiva têm sido pouco abordadas na literatura. No entanto, tem‐se observado ao longo da última década um aumento da chegada aos centros de urgências de pacientes jovens com diferentes formas de crise hipertensiva. Realizamos este estudo a fim de conhecer as características clínicas e epidemiológicas dos pacientes de idade até 45 anos internados com o diagnóstico de emergência hipertensiva.
MétodoFoi realizado um estudo observacional, descritivo, transversal e proletivo a 123 pacientes internados com emergências hipertensivas no Hospital do Prenda, de maio de 2011 a junho de 2012.
ResultadosA idade média foi de 36,62 ± 5,49 anos, principalmente sexo masculino (52,85%). O principal fator de risco foi a hipertensão arterial (65,9%), com uma adesão de 17,3%. Formas de apresentação fundamentais: encefalopatia hipertensiva e acidente vascular cerebral hemorrágico (9,8 e 82,1%, respetivamente). As principais drogas utilizadas foram os diuréticos, inibidores da ECA e antagonistas de cálcio. Trinta e um pacientes morreram durante o internamento para uma mortalidade de 25,2%, com acidente vascular cerebral hemorrágico, a causa mais comum. Existiu associação significativa entre idade e mortalidade durante o internamento.
Conclusões30,1% dos pacientes internados com emergência hipertensiva eram jovens de idade até 45 anos. O acidente vascular cerebral hemorrágico foi a apresentação mais comum. Há relação significativa entre o modo de apresentação, a idade e mortalidade durante o internamento.
Hypertension (HTN) is a known cardiovascular risk factor and one of the most common diseases encountered in clinical practice, in outpatient, hospital and emergency department settings.1
One form of presentation of complications in HTN is hypertensive crisis, defined as an inappropriate, rapid and symptomatic rise in blood pressure (BP), with or without potential acute damage to target organs (brain, heart, kidneys and arteries) that can be life‐threatening. The definition includes diastolic BP over 120 mmHg, but lower values can also lead to serious damage, as in acute glomerulonephritis and eclampsia.2,3
Hypertensive crisis can be classified as urgency or emergency. Hypertensive emergencies are distinguished from hypertensive urgencies by the presence of acute target‐organ damage that is immediately life‐threatening, and thus require BP to be lowered within an hour through intravenous drug therapy.2
The incidence and prevalence of hypertensive emergencies have been rarely addressed in the literature. It is estimated that around 1% of the general population may suffer a hypertensive crisis. With the advent of new antihypertensive drugs, the incidence of malignant HTN with papilledema has fallen from 7% to 1%.4 However, over the last decade increasing numbers of young patients with different forms of hypertensive crisis have been observed in emergency departments. Most of these patients have already been diagnosed with HTN, but are either untreated or uncontrolled.5
Even though the condition is clearly defined, as above, diagnosis and treatment of hypertensive emergencies are the subject of disagreement, but are of the utmost importance in order to prevent the serious damage that can result from the condition.
In light of the above, we set out to ascertain the prevalence of hypertensive emergencies in young patients aged ≤45 years admitted to our hospital.
MethodsThis was an observational, descriptive, cross‐sectional prospective study of patients aged ≤45 years admitted with hypertensive emergencies in the Hospital do Prenda, Luanda between May 1, 2011 and May 31, 2012.
A total of 409 patients were hospitalized for hypertensive emergencies during the study period. The patients’ medical records were reviewed and any missing data were collected directly from patients or their relatives. All those aged ≤45 years were included in the study. This was a convenience sample, which after application of the inclusion criteria, consisted of 123 patients, 30.1% of the overall population.
Clinical variablesCardiovascular risk factors were analyzed, including age, gender, smoking, HTN, diabetes, dyslipidemia, obesity, previous stroke and alcohol abuse. Laboratory tests included hemogram, with anemia defined as hemoglobin <10×109/l and leukocytosis as white blood cell count >10×109/l; urea, considered elevated when >50.0 mg/dl; blood glucose, with hyperglycemia defined as >126 mg/dl and hypoglycemia as <40 mg/dl; creatinine, considered elevated when >1.1 mg/dl; and transaminases, considered elevated when oxaloacetic transaminase >37.0 U/l and glutamic pyruvic transaminase >42.0 U/l.
Statistical analysisThe data were processed using Minitab 15 statistical software (State College, Pennsylvania). Univariate analysis of the variables was performed, using the Student's t test for quantitative variables and the chi‐square test and Fisher's exact test for qualitative variables. The degree of association between qualitative and quantitative variables was determined by ANOVA. The level of statistical significance used was p<0.05, with 95% confidence intervals. The results were expressed as percentages and means.
ResultsThe study population consisted of 123 patients, 30.1% of all hypertensive emergencies during the period under analysis. Mean age was 38.62±5.49 years. The sample included 65 men and 58 women (52.85% and 47.15%, respectively), and most patients of both sexes were aged >41 years (Table 1).
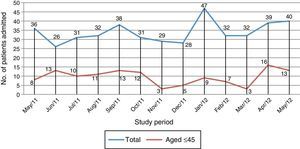
Figure 1 shows the total number of patients and those aged ≤45 years admitted for hypertensive emergency during the study period.
HTN was the most prevalent cardiovascular risk factor (65.9% of patients), followed by alcohol abuse (8.9%), as shown in Table 2; previous stroke was the next most common (nine patients).
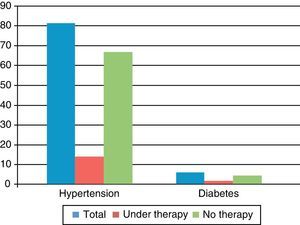
Poor compliance with therapy was found in both hypertensive and diabetic patients, only 17.3% of hypertensives and 33% of diabetic patients being under therapy at admission (Figure 2).
The most common diagnosis on admission was hemorrhagic stroke (82.1%), followed by hypertensive encephalopathy (9.8%) (Table 3). This finding is important, since hemorrhagic stroke causes severe sequelae that significantly reduce productivity, with serious repercussions for society.
With regard to diagnostic exams, 85% of patients underwent laboratory tests in the emergency department, including complete hemogram, urea, blood glucose, creatinine and thick blood film for malaria. Most patients were within normal ranges for blood cell counts, blood glucose, creatinine, transaminases and urea (Table 4).
Diagnostic exams and findings.
| n | % | |
| Brain CT | 85 | 69 |
| Hemorrhage | 75 | 88.2 |
| Ischemia | 4 | 4.7 |
| No alterations | 5 | 5.9 |
| Other diagnoses | 1 | 1.2 |
| Not performed | 38 | 31 |
| Hemogram | 110 | 89.4 |
| Normal | 62 | 56.4 |
| Anemia | 8 | 7.3 |
| Leukocytosis | 40 | 36.4 |
| Not performed | 13 | 10.6 |
| Urea | 97 | 78.9 |
| Elevated | 20 | 20.1 |
| Not performed | 26 | 21.1 |
| Blood glucose | 103 | 83.7 |
| Hyperglycemia | 5 | 4.9 |
| Hypoglycemia | 1 | 0.97 |
| Normal | 97 | 94.2 |
| Not performed | 20 | 16.3 |
| Creatinine | 101 | 82.1 |
| Elevated | 19 | 18.8 |
| Not performed | 22 | 17.9 |
| Transaminases | 23 | 18.7 |
| Elevated | 9 | 39.1 |
| Not performed | 100 | 81.3 |
| Thick blood film | 103 | 83.7 |
| Positive | 4 | 3.9 |
| Not performed | 20 | 16.3 |
| HIV | 60 | 48.9 |
| Positive | 5 | 8.3 |
| Not performed | 63 | 51.1 |
CT: computed tomography; HIV: human immunodeficiency virus.
Brain computed tomography was performed in 70.8% of patients diagnosed with stroke or hypertensive encephalopathy, and revealed that 88.2% had suffered cerebral bleeding.
With regard to therapy during hospital stay, angiotensin‐converting enzyme (ACE) inhibitors were administered in 94.3%, diuretics in 97.6%, calcium channel blockers in 49.6%, and antibiotics in 25.2%. Other antihypertensive drugs were used intravenously in 26% of patients, most commonly hydralazine (Table 5).
Drug treatment during hospital stay.
| n | % | |
| Beta‐blockers | 6 | 4.9 |
| IV nitrates | 1 | 0.8 |
| Oral nitrates | 5 | 4.1 |
| Calcium channel blockers | 61 | 49.6 |
| Heparin | 0 | 0 |
| Aspirin | 3 | 2.4 |
| ACE inhibitors | 116 | 94.3 |
| Diuretics | 120 | 97.6 |
| Antibiotics | 31 | 25.2 |
| Other IV therapy | 32 | 26.0 |
ACE: angiotensin‐converting enzyme; IV: intravenous.
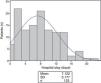
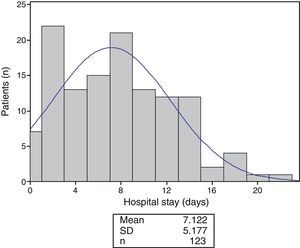
Mean hospital stay was 7.12±5.2 days, the highest proportion being hospitalized for two days (Figure 3).
In‐hospital mortality was 38.1% (31 patients), all with a diagnosis of hemorrhagic stroke, a mortality rate of 25.2% of hypertensive emergencies.
There was a significant association (p=0.003) between form of presentation of hypertensive emergency and outcome (Table 6). No correlation was found between either gender or risk factors and outcome (Tables 7 and 8).
Correlation between form of presentation and outcome.
| Outcome | ||||||
| Survived | Died | Total | ||||
| n | % | n | % | n | % | |
| Unstable angina | 1 | 100 | 0 | 0 | 1 | 0.8 |
| Hemorrhagic stroke | 70 | 69.3 | 31 | 30.7 | 101 | 82.1 |
| Acute pulmonary edema | 3 | 100 | 0 | 0 | 3 | 2.4 |
| Hypertensive encephalopathy | 12 | 100 | 0 | 0 | 12 | 9.8 |
| Subarachnoid hemorrhage | 5 | 100 | 0 | 0 | 5 | 4.1 |
| Renal failure | 1 | 100 | 0 | 0 | 1 | 0.8 |
| Total | 92 | 74.8 | 31 | 25.2 | 123 | 100 |
p=0.0033.
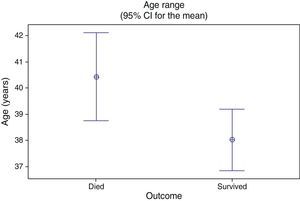
Finally, a significant association was observed between older age and in‐hospital mortality (p=0.034), as shown in Figure 4.
DiscussionThere have been few studies analyzing the characteristics of patients, especially young patients, with hypertensive emergency admitted to hospitals, despite the known seriousness of the condition. A review of the literature found no study of this entity in Angola, and so we only cite studies performed in the USA and Europe.
Patients with hypertensive emergency represent 4.3% of all cases seen in the emergency department. This is higher than the results of the SUHCRIHTA study, in which the prevalence was 0.41%.6 The Argentinian REHASE study showed a prevalence of 1.17%, while Vilela et al. reported a 0.6% prevalence of hypertensive crisis among patients seen in emergency departments in Brazil.7,8 The higher prevalence in our study population may be explained by a lower proportion of patients with a previous diagnosis of HTN, as well as poor compliance with prescribed therapy.
With regard to gender distribution, there was a predominance of male patients, but without statistical significance. This is in agreement with the results of the SUHCRIHTA and REHASE studies and a Spanish study by Cerrillo et al.6,7,9 Only a study by Curbelo et al. showed a significant predominance of men,10 which may be related to their greater access to health care services.
While none of the studies to date have sought specifically to assess the prevalence of hypertensive emergency among young patients, some divided their study populations into age‐groups that can be compared with our sample. For example, in the study by Curbelo et al. there was a predominance of patients in the 40-49 age‐group,10 while Vilela et al. found a higher proportion of patients of both sexes aged 41-50.8 Comparison of these studies with ours reveals a similar pattern, that the older the patient the greater the risk of target‐organ damage to the vascular system.6–10
Previous HTN, alcohol abuse and diabetes were the main risk factors in our population, which is in agreement with other studies in which over 50% of patients were hypertensive.6–10 We would highlight the low rate of compliance with antihypertensive therapy in our sample (17.3%), far lower than in other studies. For example, Cerrillo et al. reported 87.4% compliance,9 while in the SUHCRIHTA and REHASE studies only 18.9% and 17% of patients, respectively, had abandoned treatment.6,7 This shows how much remains to be done in educating Angolans on the need for continuous treatment of HTN in order to prevent target‐organ damage, and the need for policies at the governmental level to improve access to drugs by reducing prices, possibly including free distribution to the poorest sections of society.
Smoking is a risk factor for hypertensive emergency in most studies in the literature,6–10 but this was not the case in our study, in which no patient was a smoker or ex‐smoker. This may be related to the young age of the study population and the low rate of smoking among the Angolan population.
Cerebral bleeding was the most common form of presentation in our population, in agreement with various studies, including the SUHCRIHTA study and those of Vilela et al. and Curbelo et al.6,8,10 In others, acute coronary disease was the main form of presentation7,9; however, this may be related to the countries and regions where these studies were performed, since most were European or American, and populations in Africa, particularly Angola, have a low incidence of coronary disease. In addition, our patients were younger than in other studies, and ischemic heart disease is found mainly in individuals aged over 50; this may explain the low incidence of acute coronary syndrome in our sample.
Most of the studies reviewed did not include among their objectives analysis of the diagnostic exams performed during hypertensive emergencies, and so any comparison is difficult. In our study, brain computed tomography was performed in most patients with suspected stroke or hypertensive encephalopathy, essentially to exclude both diagnoses. All blood tests were normal.
The drugs most frequently administered in our study population were diuretics (mainly furosemide), ACE inhibitors and calcium channel blockers, as in other studies.6,9
None of the previous studies assessed mortality or correlations between variables, being limited to descriptions of the phenomenon. Mortality in our study was 25.2% and showed a significant association with both form of presentation and age.
To summarize, our study is the first on the prevalence of hypertensive emergency in Angola, and is relevant to medical emergencies, associated risk factors and the most common types of target‐organ damage.
The main limitation of our study is that it was performed in a single hospital, and so its results are only applicable to a selected proportion of the population. However, the study period was longer than in the similar studies mentioned above.
ConclusionsOf the patients admitted with hypertensive emergencies in the Hospital do Prenda during the study period, 30.1% were aged ≤45 years. The main risk factor was a previous diagnosis of HTN, and only 17.3% were complying with therapy at the time of admission. Hemorrhagic stroke was the most common form of presentation.
The main drugs administered were diuretics, ACE inhibitors and calcium channel blockers.
In‐hospital mortality was 25.2%, and there was a significant association between form of presentation, age and outcome.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Martínez G, Miúdo V, da Graça Alves C, et al. Caracterização dos pacientes com menos de 46 anos internados com emergência hipertensiva no Hospital do Prenda. Rev Port Cardiol. 2014;33:19–25.