Hepatocellular carcinoma with extension or metastasis to the right atrium is an uncommon form of cardiac malignancy.
The authors report the case of a 51-year-old patient with hepatocellular carcinoma and thrombi in the portal and mesenteric veins, which histopathology revealed to be metastatic. Echocardiography showed a right atrial mass which in this context has to be considered as a possible cardiac metastasis.
O carcinoma hepatocelular com extensão ou mestástases para a aurícula direita é uma forma de doença cardíaca maligna pouco frequente.
Os autores relatam o caso de um doente de 51 anos de idade a quem foi diagnosticado carcinoma hepatocelular com trombos a nível das veias porta e mesentérica, cuja análise histopatológica revelou ser compatível com metástases. O ecocardiograma revelou uma massa na aurícula direita que, neste contexto, deve ser considerada como possível metástase cardíaca.
Cardiac tumors can be primary or secondary (metastatic), the latter being more common. Cardiac metastases of hepatocellular carcinoma (HCC) are rare (0.67-3%) and usually appear in advanced stages of the disease1–3.
HCC is the most common primary neoplasm of the liver, accounting for 4.6% of all new cancer cases annually. Cirrhosis is present in around 95% of cases, of which 15-20% are due to hepatitis C infection. Diagnosis of HCC can be by anatomopathological study or, in patients with cirrhosis, it can be based on noninvasive criteria: imaging studies that show a hypervascular nodular lesion of more than 2cm with wash-out, or elevation of alpha-fetoprotein (>200ng/ml). Bones, lungs and adrenal glands are the main sites of metastasization4.
While rare, HCC is the fourth most common tumor that metastasizes to the right atrium (RA), after kidney, thyroid and testicular cancer5–7.
Echocardiography plays a crucial role in such cases as it is invaluable for the evaluation of intracardiac masses. It can determine the characteristics, location, shape, size and mobility of the mass, and is noninvasive, making it a practical diagnostic modality. Taken together with the clinical context, it can usually distinguish between the three main types of intracardiac masses: tumor, thrombus and vegetation8.
The authors report the case of a patient with HCC and thrombi with cancer cells in the portal and mesenteric veins, in whom an intracardiac mass was detected on echocardiography. They also review the literature, clinical aspects and the various diagnostic exams that can be used for this rarely encountered and documented entity.
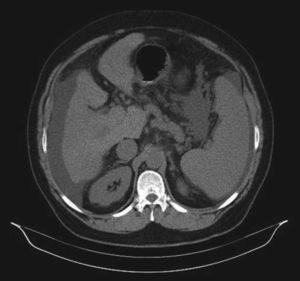
Case reportThe case presented is of a 51-year-old male patient, white, with a personal history of cirrhosis of the liver due to hepatitis C virus, which he had had for around 25 years (initially diagnosed as non-A, non-B hepatitis). Cardiovascular risk factors included smoking and overweight, but no previously known cardiovascular disease. He was regularly followed in internal medicine and hepatology consultations, and had been hospitalized on several occasions in the previous five years for decompensated liver disease. The patient's baseline clinical status, despite optimized pharmacological therapy and regular paracentesis, included dyspnea on moderate exertion, mild to moderate lower limb edema, and ascites. During the previous hospitalization, for worsening edema and marked anorexia and asthenia, he underwent abdominal computed tomography (CT), which revealed nodular lesions in the liver and extensive thrombosis of the portal vein, extending up to the superior mesenteric vein (Figure 1). Cytological analysis of the hepatic lesions showed they were compatible with HCC, and needle biopsy of the portal vein thrombus revealed cancer cells characteristic of HCC. The patient underwent radiofrequency ablation of the nodules after stabilization and clinical discharge.
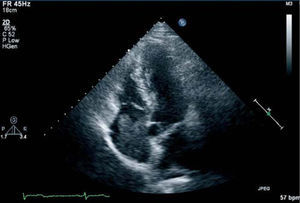
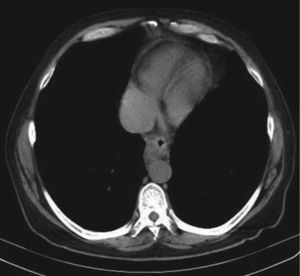
However, approximately two months later, he presented progressive worsening of exertional dyspnea, together with dyspnea at rest and orthopnea, as well as worsening lower limb edema and ascites. Echocardiography was accordingly performed, which showed a hyperechogenic structure measuring 5 × 3.2cm adhering to the lateral wall of the RA (Figure 2). Thoracic CT also showed an image suggestive of an intracavitary thrombus in the RA, extending proximally to the vena cava (Figure 3). The cardiac lesion was interpreted as secondary to HCC. In view of the history and findings and after weighing the risks and benefits (a high-risk patient unsuitable for surgery), no further study was undertaken. The patient died shortly after diagnosis of the cardiac lesion.
Few cases have been reported of cardiac metastases in patients with HCC. Intracavitary involvement is rare, usually resulting from cardiac extension via the venae cavae, and is rarer still when the latter are not involved, with only 16 patients in the literature showing this type of metastasization3,7,9. Right atrial involvement is found on autopsy in 2.6% of patients with HCC of non-cirrhotic origin and 1.6% of those with cirrhosis. Clinical diagnosis is often difficult, since symptoms are frequently absent or are masked by the underlying disease3. Two-dimensional echocardiography plays a crucial role in the diagnosis of cardiac tumors, particularly in these cases3,8–10.
As with other types of cancer, cardiac metastasis of HCC has a poor prognosis, since surgical resection is usually impossible or incomplete. Surgery generally has disappointing results and should therefore be reserved for cases in which there is acute and severe cardiovascular distress7,9,11.
Both diagnosis and treatment of the case presented were the subject of multidisciplinary discussion with internal medicine and hepatology specialists. Palliative medical therapy was optimized and achieved clinical stability, but given the very poor preoperative prognosis and high risk, it was decided not to operate, which would have provided a specimen for histological diagnosis of the lesion.
After a review of the literature and bearing in mind the clinical context and the results of imaging and histological studies, the RA lesion was interpreted as a metastasis of HCC. Imaging studies, particularly echocardiography and CT (which showed the continuity between the RA lesions and the inferior vena cava), when duly contextualized, were shown to be valuable and practical non-invasive diagnostic techniques.
ConclusionThis case shows the evolution of HCC metastasizing to the RA via the inferior vena cava, documented by two-dimensional echocardiography and CT. It illustrates the complexity of systemic diseases like cancer, in which the heart is occasionally affected, leading to decompensation of the underlying disease and rapid clinical deterioration. The authors also wish to highlight the importance of a range of data for the diagnosis of a disease that should not be defined by, or depend on, a particular diagnostic exam, such as histological analysis of the lesion itself. This is not always possible or even advisable, as seen in diagnosis of hepatocellular carcinoma, which is often based on laboratory and imaging criteria alone.
AcknowledgementsThe authors are grateful to Dr. Presa Ramos of the Hepatology Unit of the Internal Medicine Department at Hospital de Vila Real.