In December 2019, SARS-CoV-2, was discovered as the agent of COVID-19 disease. Cardiac arrhythmias have been reported as frequent but their incidence is unknown. The aim of this research was to assess the real incidence of cardiac arrhythmias among COVID-19 patients admitted to Portuguese hospitals and to understand the underlying prognostic implications.
MethodsThe Portuguese Association of Arrhythmology, Pacing and Electrophysiology (APAPE) conducted a survey in Portuguese hospitals to assess the occurrence of arrhythmias in COVID-19 patients, their clinical characteristics, the use of experimental therapies and the impact on QT interval.
ResultsTwenty hospitals participated, reporting 692 hospitalized patients. An arrhythmic episode occurred in 81 (11.7%) and 64 (79%) had detailed information on these episodes. New onset arrhythmias occurred in 41 (64%) patients, 45 (70.3%) male, median age 73.5 (61-80.3) years. There were 51 (79.7%) with associated comorbidities, mainly arterial hypertension (41, 64.1%). Of 53 patients (82.3%) on experimental therapy, 7 (10.9%) had an increased QTc interval. Regarding arrhythmias, two patients (3.1%) had ventricular tachycardia, 5 (7.8%) sinus bradycardia, 17 (26.6%) paroxysmal supraventricular tachycardia and 40 (62.5%) atrial fibrillation or flutter. At the time of reporting, there had been no deaths due to arrhythmic syndrome or related complications.
ConclusionsIn a population of COVID-19 patients. The incidence of cardiac arrhythmias is high but not associated with increased cardiac mortality although it does though occur frequently in extremely ill patients and with multiple organ failure. Regardless of the use of experimental drugs, the incidence of ventricular arrhythmias is low and atrial fibrillation and other supraventricular arrhythmias are the most prevalent arrythmias.
Em dezembro de 2019, o SARS-CoV-2 foi descoberto como agente da doença Covid-19. As arritmias cardíacas são reportadas como frequentes, mas a sua incidência é desconhecida. O objetivo deste trabalho foi entender a incidência de arritmias em doentes Covid-19 tratados em hospitais portugueses e entender as suas implicações prognósticas.
MétodosA Associação Portuguesa de Arritmologia, Pacing e Electrofisiologia (APAPE) conduziu um inquérito em hospitais portugueses, documentando a ocorrência de arritmias em doentes com Covid-19, as suas caraterísticas clínicas, o uso de terapêutica experimental e o seu impacto no intervalo QT.
ResultadosParticiparam 20 hospitais, reportando 692 doentes hospitalizados. Ocorreram episódios arrítmicos em 81 (11,7%), 64 (79%) com informação adicional. Documentaram-se arritmias de novo em 41 (64%) doentes, 45 (79%) do sexo masculino, idade mediana 73,5 (61-80,3) anos. Destes, 51 (79,7%) tinham comorbilidades associadas, maioritariamente hipertensão arterial (41, 64,1%). Dos 53 (82,3%) doentes sob terapêutica experimental, 7 (10,9%) tiveram aumento do intervalo QTc. Tiveram taquicardia ventricular 2 (3,1%) doentes, 5 (7,8%) bradicardia sinusal, 17 (26,6%) taquicardia paroxística supraventricular e 40 (7,8%) fibrilhação ou flutter auricular. Nenhum doente teve morte por causa arrítmica ou complicações associadas, à data do registo.
ConclusõesNuma população de doentes com Covid-19, a incidência de arritmias é elevada, mas não associada a aumento de mortalidade cardíaca, apesar da ocorrência mais frequente em doentes graves e com falência multiorgânica. Independentemente do uso de terapêuticas experimentais, a incidência de arritmias ventriculares é baixa e a fibrilhação auricular e outras arritmias supraventriculares são as arritmias mais prevalentes.
In December 2019, an increasing number of cases of patients with pneumonia of unknown origin was detected in the Hubei province in China,1,2 and SARS-CoV-2, a novel coronavirus capable of human infection and transmission, was found to be responsible. The virus led to a pandemic, with more than 53.1 million reported infections and 1.3 million deaths3 to date. However, numbers may be in fact higher due to the virus being highly infectious and asymptomatic patients being capable of transmission.4–6 COVID-19 disease presents with a wide range of symptoms but predominantly as an acute respiratory disease and fever7 leading to hospitalization in about 10-15% of patients and critical intensive care (ICU) in 3-14.2% of patients.7–11 With growing knowledge about the disease, other clinical symptoms are constantly being reported. Respiratory failure, cytokine storm, thromboembolic phenomena and acute fulminant myocarditis are the predominant known causes of death12–14 with a 1.2-7.7% case-fatality rate worldwide to date. However, it may in fact be lower if the presumed asymptomatic undetected cases are accounted for, or higher, as in the elderly or in people with known associated diseases.3,7,10,15,16 In the latter group, cardiovascular comorbidities account for a higher mortality risk (10.5%),11,17,18 as well as diabetes and chronic obstructive pulmonary disease. Cardiac arrhythmias have been reported as a frequent event in this population as the estimates account for 16.7% among hospitalized patients and 44% in ICU patients.19,20 In these patients, the effect of multiorgan damage and cardiac lesion on cardiac rhythm, as well as the effect of experimental therapies for treatment is yet unknown.
ObjectivesThe aim of this research was to assess the real incidence of cardiac arrhythmias among COVID-19 patients admitted to Portuguese hospitals and to understand the underlying prognostic implications, in order to provide useful knowledge for the management of these patients.
MethodsStudy populationThe Portuguese Association of Arrhythmology, Pacing and Electrophysiology (APAPE) conducted a survey between April 12 and May 10 of 2020 among affiliated Pacing and Electrophysiology laboratories in Portuguese hospitals to assess the occurrence of arrhythmias in patients infected with SARS-CoV-2 and their clinical characteristics. Confirmed COVID-19 patients, with at least one positive reverse transcriptase polymerase chain reaction test for SARS-CoV-2 and non-mild clinical progression that resulted in hospital admission were included, irrespective of the predominant symptoms. In the subgroup of patients with continuous cardiac monitoring, admitted to intensive or intermediate care units, the prevalence of arrhythmias, their type and outcome were assessed.
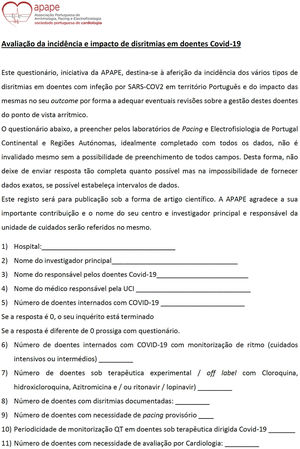
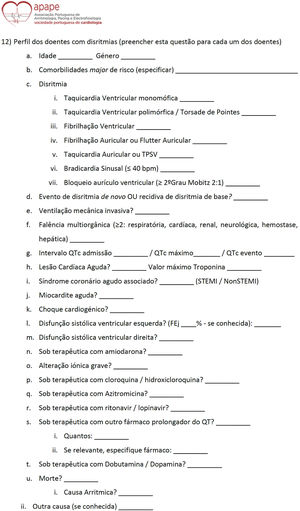
Patient evaluation and survey conductedThe reporting hospitals that agreed to participate were included in the study and were asked to report the number of patients admitted with COVID-19, the use of experimental therapies for the disease and the mode of QT interval monitoring, and the need for cardiologic evaluation (Figure 1). In the event arrhythmic episodes were detected, the investigators at each hospital were invited to report additional information, as detailed as possible (Figure 2). This included, comorbidities, clinical and laboratory evolution, arrhythmia type, new onset arrhythmia versus recurrent arrhythmia, therapy, any major adverse events during hospitalization, death, and its cause.
Statistical analysisAll analysis was performed using version 12 of STATA® (Statistics Data Analysis). Data are presented as median, lower and upper quartiles (Q1-Q3) for continuous variables and as absolute number and percentage for categorical variables.
Ethics disclosureAt each center, data were collected retrospectively using a standardized data collection form (Figures 1 and 2) sent to all the participating hospitals. Patient identification was registered in the participating centers but was not transferred to APAPE, so the compiled data remained anonymous.
This study complies within the Declaration of Helsinki rules.
ResultsStudy populationTwenty hospital centers nationwide participated in the survey. During the study period, there were reports of 692 hospitalized patients with COVID-19. A subgroup of 393 (56.8%) patients was admitted to ICU or had continuous cardiac monitoring. In this subgroup of patients, 81 (20.6%) experienced an arrhythmic episode.
Experimental therapyAmong all hospitalized patients, 443 (64%) were under experimental therapy for COVID-19 (ritonavir/lopinavir, hydroxychloroquine or azithromycin). The QT assessment in these patients was performed daily in ICU or if the QT interval (QTc) were above 450ms and every other 48-72h in the remaining patients. Cardiologic assessment was needed in 65 (9.4%) patients (reasons for evaluation not detailed).
Patients with arrhythmiasIn the subgroup of patients with arrhythmias, detailed additional information was available in 64 patients, of whom 45 (70.3%) were male, median age was 73.5 (61-80.3) years. There were 51 (79.7%) patients with associated comorbidities, median of 3 (1-4) (Table 1). Arterial hypertension was the most prevalent comorbidity, in 41 (64.1%) of patients, 23 (36%) patients had dyslipidemia, 22 (34.4%) patients were diabetic and 19 (29.7%) patients had previously diagnosed atrial fibrillation.
Clinical and laboratory characteristics of patients with arrhythmias.
| Clinical and Laboratory characteristics | n=64 |
|---|---|
| Male gender | 45 (70.3%) |
| Age | 73.5 (61-80.25) |
| Previous arrhythmias | 23 (35.9%) |
| Comorbidities | 51 (79.7%) |
| Hypertension | 41 (64.1%) |
| Diabetes | 22 (34.4%) |
| Coronary artery disease | 9 (14%) |
| Cerebrovascular disease | 10 (16%) |
| Heart failure | 7 (10.9%) |
| Dyslipidemia | 23 (36%) |
| Chronic obstructive pulmonary disease | 7 (10.9%) |
| Atrial fibrillation | 19 (29.7%) |
| Chronic kidney disease | 14 (21.9%) |
| Other comorbidities* | 30 (46.9%) |
| Experimental therapy | 53 (82.3%) |
| Lopinavir/ritonavir | 16 (25%) |
| Hydroxychloroquine | 49 (76.6%) |
| Azithromycin | 35 (54.7%) |
| QT prolonging drugs | 49 (76.6%) |
| Lopinavir/ritonavir | 16 (25%) |
| Hydroxychloroquine | 49 (76.6%) |
| Azithromycin | 35 (54.7%) |
| Amiodarone | 19 (29.7%) |
| Metoclopramide | 8 (12.5%) |
| Quetiapine | 12 (18.8%) |
| Olanzapine | 3 (4.7%) |
| Haloperidol | 6 (9.4%) |
| Other drugs | 18 (28.1%) |
| QT prolongation | 7 (10.9%) |
| Severe ionic disturbances | 7 (10.9%) |
| Increased troponin I (pg/L) | 48 (75%) |
| Left ventricle systolic dysfunction | 9 (14.1%) |
| Right ventricle systolic dysfunction | 1 (1.6%) |
| Acute cardiac lesion | 33 (51.6%) |
| Acute coronary syndrome | 4 (6.3%) |
| Acute myocarditis | 1 (1.6%) |
| Hemodynamic instability | 2 (3.1%) |
| Cardiogenic shock | 4 (6.3%) |
| Mechanical ventilation | 35 (54.7%) |
| Multiple organ failure | 33 (52%) |
Among the monitored patients, 9 (14%) had left ventricular systolic dysfunction and one (1.6%) had right ventricular dysfunction. Acute cardiac injury occurred in 33 (51.6%) of the patients, non-ST elevation acute myocardial infarction in four (6.3%) and myocarditis in one (1.6%). Median peak value of cardiac Troponin I was 73.5 (28.9-278.3) pg/L. There were seven (10.9%) patients with significant electrolyte disorder at the time of arrhythmia onset.
There were 35 (54.7%) on mechanical invasive ventilation for respiratory failure and 33 (52%) had multiple organ failure. Only four (6.3%) patients developed cardiogenic shock, three in the setting of acute cardiac injury of unknown cause with new onset left ventricle systolic dysfunction and one after non-ST elevation acute myocardial infarction. Myocardial biopsies and cardiac magnetic resonance were not performed.
In this arrhythmia subgroup, 53 patients (82.3%) were under experimental therapy for COVID-19, of whom 49 (76.6%) received hydroxychloroquine, 35 (54.7%) received azithromycin and 16 (25%) received lopinavir/ritonavir. Additionally, 49 patients (76.6%) were concomitantly taking other drugs that could prolong QT21 (median two, one to three drugs) of whom 19 (29.7%) were also on antiarrhythmic therapy with amiodarone. Only seven patients (10.9%) had an increased QTc interval, minimum 480ms and maximum 596ms.
An arrhythmic episode was a recurrence of a previously existing arrhythmia – atrial fibrillation (AF) – in 23 patients (35.9%) and new onset arrhythmia in 41 patients (64.1%). Regarding arrhythmic episodes, two patients (3.1%) had ventricular tachycardia, five (7.8%) patients sinus bradycardia, 17 (26.6%) paroxysmal supraventricular tachycardia and 40 (62.5%) AF or atrial flutter.
Patients with supraventricular arrhythmias, as opposed to those with the other types of arrhythmias, presented with more severe disease, being more frequently placed on mechanical ventilation (33, 57.9%), with hemodynamic instability (two, 3.5%) and cardiogenic shock (four, 7.0%) and with multiple organ failure 32 (56.1%) (Table 2), as reflected by higher absolute and relative frequencies. Both patients with ventricular tachycardia had QT prolongation but the clinical course was milder Table 2).
Clinical and laboratory characteristics of patients, according to type of arrhythmias.
| SVT (n=57) | VT (n=2) | Sinus bradycardia (n=5) | |
|---|---|---|---|
| Left ventricle systolic dysfunction | 7 (12.3%) | 1 (50%) | 1 (20%) |
| Hemodynamic instability | 2 (3.5%) | 0 | 0 |
| Acute cardiac lesion | 30 (52.6%) | 0 | 3 (60%) |
| ACS | 4 (7.0%) | 0 | 0 |
| Myocarditis | 0 | 0 | 0 |
| Troponin I (pg/L) | 75 (35.1-309.5) | 10.1 (9-11.1) | 114.9 (65.9-156.5) |
| Mechanical ventilation | 33 (57.9%) | 1 (50%) | 1 (20%) |
| Cardiogenic shock | 4 (7.0%) | 0 | 0 |
| Multiple organ failure | 32 (56.1%) | 0 | 0 |
| Severe ionic disturbances | 6 (10.5%) | 0 | 1 (20%) |
| Prolonged QT interval | 4 (7.0%) | 2 (100%) | 1 (20%) |
Legend: ACS: acute coronary syndrome; SVT: supraventricular tachycardia; VT: ventricular tachycardia.
Concerning outcomes, 20 (31.3%) patients died and the main identified cause was respiratory failure in 12 (60%) and refractory septic shock in four (20%), with only one patient (5%) dying of a direct cardiac cause (cardiogenic shock). None of the patients had arrhythmic death nor was the arrhythmia episode found to contribute to their death.
DiscussionAs SARS-CoV-2 is a newly detected coronavirus capable of infecting humans and causing COVID-19 disease, there is a lot of uncertainty regarding risk factors for disease outcome, as well as the best therapeutic strategies. Although acute pneumonia is the hallmark of the disease, there are several reports of additional direct organ damage from COVID-19, including acute heart failure and cardiac arrhythmias.13,14,22 Whether naturally resulting from the disease or from the treatment, its true incidence is still unknown. Currently, remdesivir and dexamethasone appear to be the most promising therapeutic drugs for treating COVID-19 patients, as they demonstrated a reduction in disease duration and severity.23–27 At the time of data collection for this study, other experimental therapeutic targets for COVID-19 were in use and they have the additional potential of inducing arrhythmias, as is the case of chloroquine/hydroxychloroquine.4,22
In our registry, we aimed to assess the incidence of arrhythmic global events in COVID-19 patients as well as the potential harmful effects of experimental therapies on major cardiac adverse events. These results show that in a population of patients hospitalized for COVID-19 in Portuguese hospitals, with cardiac continuous monitoring and admitted to intermediate or intensive care, there was a preponderance of male patients and a prevalence of older age groups. Likewise, patients with associated comorbidities,8,10,28–31 especially arterial hypertension, dyslipidemia, type 2 diabetes and AF are prone to severe disease.
The majority of patients were on experimental therapy for COVID-19, although not yet proven to be efficacious.22,32 This is particularly dangerous33–38 because a high percentage of these patients were also on other concomitant QT prolonging drugs. In our survey, more than 10% of patients displayed QT prolongation, although there was no evidence of polymorphic ventricular tachycardia, Torsade de Pointes or ventricular fibrillation. The incidence of prolonged QT was high,39,40 when compared with the 6% reported incidence in the normal population but in line with QT prolongation in populations with comorbidities such as diabetes, hypertension and ischemic cardiac disease, as is the case of our population.41 Additionally, this higher QT prolongation was probably due to the extremely high percentage of concomitant drugs (Table 1) and not related to electrolyte disturbances (which were low). This corroborates other studies that report the incidence of QT prolongation in patients taking these drugs.21 Since chloroquine/hydroxychloroquine are drugs that are still in use in COVID-19 studies, there is an increased need for a standardized QT interval monitoring protocol. Overall, the global incidence of arrhythmic events was high (11.7%), characterized mostly by new onset arrhythmias. Most patients with arrhythmias were critically ill patients with respiratory and multiple organ failure. These patients pose a greater challenge in management and had a bad outcome. The most frequent arrhythmic events were paroxysmal supraventricular tachycardia and AF, which can be associated with severe pulmonary disease and multiorgan failure per se, rather than cardiac lesion due to SARS2-CoV-2 and were not responsible for death events. Although patients with ventricular arrythmias had an arrhythmic substrate (either a prolonged QT or severe left ventricle dysfunction) and the mortality rate was high, the cause of death was due to respiratory failure.
Regarding the impact of COVID-19 on other cardiovascular outcomes, in our study population, acute myocarditis had a low incidence, contrary to the previously reported information,8,13,42 as well as myocardial infarction. On the other hand, acute cardiac lesion occurred in more than half of the patients with severe disease with a non-despicable incidence (14.1% of patients) of left ventricle systolic dysfunction. Nevertheless, this did not lead to a significant impact on mortality since the leading cause of death was respiratory failure and septic shock. Direct cardiac causes of death in our population were low (cardiogenic shock or arrhythmias).
LimitationsOur study has limitations. First, although most hospitals reported for the survey, we do not have full coverage across the country and there may be biases associated with differences between centers that report or do not report data to the survey. Second, as in all large-scale surveys, some data were missing and additionally, the complete information was not mandatory due to the high workload health care providers face due to the COVID-19 pandemic. Therefore, there was only information available on arrhythmias in the subgroup of monitored patients (56.8% of the population) and detailed information was limited to 79% of this subset.
ConclusionsIn a population of COVID-19 patients admitted to Portuguese hospitals, the incidence of cardiac arrhythmias is high and occurred mostly in extremely ill patients, who were either ventilated or had multiple organ failure, but was not associated with increased cardiac mortality. Regardless of the widespread use of experimental drugs to target SARS2-CoV-2 with the potential for QT prolongation, the incidence of ventricular arrhythmias is low. Atrial fibrillation and other supraventricular arrhythmias were the most prevalent arrythmias in COVID-19 patients.
FundingNo funding was received for this study.
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors wish to congratulate all healthcare professionals involved in the management of COVID-19 patients, for their effort in spite all the difficulties a new pandemic disease imposes.
José Araújo, Hospital Beatriz Ângelo, Loures E.P.E.; Adilia Rebelo and Miguel Alves Pereira, Hospital de Braga E.P.E.; Bruno Bragança, Alice Castro and Maria Campelo, Centro Hospitalar Tâmega e Sousa E.P.E.; Daniel Caeiro, João Primo, Tiago Teixeira and Paula Castelões, Centro Hospitalar de Vila Nova de Gaia/Espinho E.P.E.; Alberto Leite, Hospital Cuf Porto; Mário Oliveira, Hospital Cuf Porto and Hospital de S. José, Centro Hospitalar de Lisboa Central, E.P.E.; Pedro Ponce, Hospital Cuf Infante Santo; Nuno Germano, Hospital de Curry Cabral, Centro Hospitalar de Lisboa Central E.P.E.; António Fontes, Alexandra Almeida Carreiro and Humberto Costa, Hospital do Divino Espirito Santo de Ponta Delgada; Ana Rita Rocha, Francisco Dias Cláudio, Francisco Azevedo, Chantre Lima and Regina Henriques, Hospital Espírito Santo Évora; Pedro Azevedo, Rui Pereira and Daniel Nuñez, Hospital de Faro, Centro Hospitalar Universitário do Algarve; Luis Brandão, Hospital Garcia de Orta E.P.E.; Alexandra Horta and António Messias, Hospital da Luz, Lisboa; David Roque, Hospital Prof. Doutor Fernando Fonseca E.P.E.; Joana Brito, João de Sousa and João Ribeiro, Hospital de St.ª Maria, Centro Hospitalar de Lisboa Norte E.P.E.; Virgilio Scheider, Hospital Santo Espirito de Angra do Heroísmo; Rita Marinheiro, Maria Lima and Rosa Ribeiro, Hospital de S. Bernardo, Centro Hospitalar de Setúbal E.P.E.; Pedro Póvoa and Pais Martins, Hospital de S. Francisco Xavier, Centro Hospitalar de Lisboa Ocidental E.P.E.; Luis Bento, Hospital de S. José, Centro Hospitalar de Lisboa Central E.P.E.; Carlos Mateus, Carmélia Rodrigues and José Caldeiro, Unidade Local de Saude Alto Minho E.P.E.; Joana Cunha and Francisco Esteves, Hospital de Vila Real, Centro Hospitalar de Trás os Montes e Alto Douro, E.P.E.