The authors report the case of a 52-year-old woman with depressive syndrome, treated with lamotrigine for about five months, who went to the emergency department for atypical precordial pain. The electrocardiogram (ECG) revealed a 2-mm downsloping ST-segment elevation and negative T waves in V1 and V2. Due to suspicion of ST-elevation acute coronary syndrome, cardiac catheterization was performed, which revealed normal coronary arteries. The initial ECG was suggestive of type 1 Brugada pattern, but subsequent serial ECGs were less typical. A flecainide test showed the same pattern.
After discontinuation of lamotrigine reversal of the typical Brugada ECG pattern was observed.
Although not currently contraindicated in Brugada syndrome, the antidepressant lamotrigine blocks sodium channels, which are usually inactivated in heart cell membranes in Brugada syndrome, and may be responsible for the expression of type 1 Brugada pattern.
Os autores relatam o caso de uma mulher de 52 anos com síndrome depressiva, medicada com lamotrigina há cerca de cinco meses, que recorre à urgência por dor pré-cordial atípica. Realizou eletrocardiograma (ECG) que revelou supradesnivelamento do segmento ST de 2 mm, em rampa descendente, e onda T negativa em V1 e V2. Por suspeita de síndrome coronária aguda com supradesnivelamento de ST, a doente efetuou cateterismo que revelou coronárias normais. O ECG da entrada era sugestivo de padrão de Brugada tipo 1, mas os ECG seriados eram menos típicos, tendo-se realizado o teste de flecainida, onde se objetivou o mesmo padrão.
Com a interrupção da lamotrigina, houve reversão do padrão eletrocardiográfico típico de Brugada.
Apesar de não estar atualmente contraindicada na síndrome de Brugada, a lamotrigina é um antidepressivo que bloqueia canais de sódio, normalmente inativados na membrana das células cardíacas na síndrome de Brugada, podendo ser responsável por manifestação de padrão de Brugada tipo 1.
Brugada syndrome is a genetic heart disease, autosomal dominant in 50% of cases, which can be caused by over 70 possible mutations, a mutation in the SCN5A gene being found in 20% of patients. It is most common in young men and usually results from accelerated inactivation of sodium channels in heart cell membranes.1,2
Diagnosis is based on clinical and electrocardiographic criteria. Patients normally have a history of syncope or sudden death, due to malignant arrhythmias such as ventricular fibrillation or ventricular tachycardia. There may also be a history of sudden death in young relatives.1–4 Two types of typical electrocardiographic patterns in leads V1-V3 are observed: type 1, more specific, with gradually downsloping ST-segment elevation of ≥2 mm, coved-type or horizontal in relation to the isoelectric line, with a symmetrical negative T wave; and type 2, with R-wave amplitude of ≥2 mm in relation to the isoelectric line, followed by ST elevation of at least 0.05 mV, with positive T waves in V2 and variable T waves in V1.1,3
Brugada ECG pattern can be intermittent and may be observed only in certain situations, such as fever, intoxication, vagal stimulation, electrolyte imbalance, acute myocardial ischemia, pericarditis or myocarditis, or be triggered by certain drugs, particularly sodium channel blockers. This pattern, which may arise from multiple causes and disappear once the cause has been rectified, is termed Brugada phenocopy.1
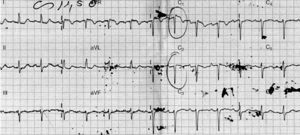
Case reportThe authors describe the case of a 52-year-old woman, with a history of hypertension, dyslipidemia and depressive syndrome, treated with lamotrigine 100 mg for about five months. There was no relevant family history. The patient went to the emergency department for atypical precordial pain (sharp, non-radiating). The admission electrocardiogram (ECG) showed 2-mm downsloping ST-segment elevation in V1 and V2 and negative T waves (Figure 1). This setting in a patient with cardiovascular risk factors was interpreted as myocardial infarction but cardiac catheterization showed normal coronary arteries.
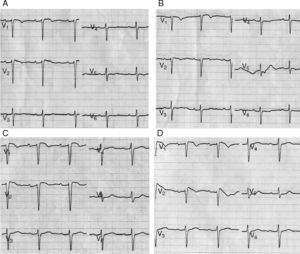
Following exclusion of infarction requiring urgent intervention, it was noted that the admission ECG was suggestive of type 1 Brugada pattern. There was no history of syncope and the echocardiogram was normal. Subsequent serial ECGs were less typical, and so a flecainide test was performed. ECGs with leads V1 and V2 positioned successively over the fourth, third and second intercostal spaces were performed before administration of the sodium channel blocker. Flecainide was then administered, the dose adjusted to the patient's weight, followed by ECGs with leads V1 and V2 positioned successively over the fourth, third and second intercostal spaces. All ECGs before administration of flecainide (Figure 2A and B) and those performed with leads V1 and V2 over the fourth (Figure 2C) and third intercostal spaces after administration of the drug showed no typical Brugada pattern; however, the ECG with leads V1 and V2 over the second intercostal space did show type 1 Brugada pattern (Figure 2D) following administration of flecainide.
ECGs performed during the first flecainide test, with the patient medicated with lamotrigine: (A) leads V1 and V2 over the fourth intercostal space, before administration of flecainide; (B) leads V1 and V2 over the second intercostal space, before administration of flecainide; (C) leads V1 and V2 over the fourth intercostal space, after administration of flecainide; (D) leads V1 and V2 over the second intercostal space, after administration of flecainide, with 2-mm downsloping ST-segment elevation and negative T waves – type 1 Brugada pattern.
The link between various psychoactive drugs and malignant arrhythmias in Brugada syndrome and type 1 Brugada phenocopy is well known. Lamotrigine is a sodium channel blocker, as are class I antiarrhythmic drugs such as flecainide. The possibility was therefore considered that lamotrigine could have triggered the Brugada pattern, and the drug was discontinued.
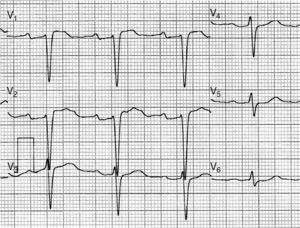
When the patient was observed again around two weeks after discontinuation of lamotrigine, she was asymptomatic, medicated with topiramate 25 mg. A further flecainide test was performed using the same protocol, and no type 1 Brugada pattern was observed on any ECG, including that with leads V1 and V2 over the second intercostal space after administration of the drug (Figure 3).
DiscussionVarious psychoactive drugs such as lithium, amitriptyline, nortriptyline, oxcarbazepine and clomipramine are contraindicated in patients with Brugada syndrome as they are associated with malignant arrhythmias, syncope and sudden death.5 Class I antiarrhythmic drugs, including flecainide, propafenone, procainamide, ajmaline and pilsicainide, which inhibit the beginning of the cardiac action potential by blocking sodium channels, are also contraindicated in Brugada syndrome for the same reason.5,6 Lamotrigine is not contraindicated in Brugada patients, but it acts through blocking voltage-dependent sodium channels in the cerebral cortex, thereby inhibiting the release of neurotransmitters.5,7 It is thus a potential trigger of type 1 Brugada pattern.
In some cases, the pattern is only evident in the upper precordial leads (V1 and V2 in the second or third intercostal spaces) since abnormal electrical activity is confined to the area of the right ventricular outflow tract. This is the principle behind the flecainide test.1
ConclusionThe case presented describes a female patient with type 1 Brugada pattern on ECG triggered by lamotrigine, which is not currently contraindicated in Brugada syndrome. The drug was discontinued due to the risk of malignant arrhythmias. However, the situation would not have been identified without knowledge of the drug's mechanism of action and of the pathophysiology of the Brugada pattern, for which the flecainide test played a fundamental role.
The case highlights the importance of familiarity with how drugs act and alertness to their potential secondary effects, which were crucial to correct diagnosis in this patient.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Rodrigues R, Amador P, Rassi L, et al. Padrão de Brugada em doente medicada com lamotrigina. Rev Port Cardiol. 2013;32:807–810.