Congenital anomalies of the inferior vena cava (IVC) are rare and very often diagnosed in asymptomatic patients during computed tomography performed for other purposes. These anomalies can have significant clinical implications, for example if electrophysiology procedures are needed. Diagnostic and ablation procedures are difficult since catheter manipulation and positioning are more complex. We present here a case of successful atrioventricular nodal reentrant tachycardia ablation in a patient with unexpected IVC agenesis, using an azygos route.
As anomalias congénitas da veia cava inferior são raras e são, muitas vezes, diagnosticadas em pacientes assintomáticos como achados de tomografia computorizada realizada com outros objetivos. Estas anomalias podem ter implicações clínicas importantes, nomeadamente quando estão programados estudos eletrofisiológicos. Os procedimentos de diagnóstico e de ablação são difíceis, uma vez que o manuseamento e posicionamento do cateter é mais complexo. Apresentamos o caso bem-sucedido de uma ablação de taquicardia por reentrada nodal auriculoventricular num doente com agenesia da veia cava inferior, utilizando uma via trans-ázigos.
Congenital anomalies of the inferior vena cava (IVC) are rare and very often diagnosed in asymptomatic patients during computed tomography performed for other purposes. These anomalies can have significant clinical implications, for example if electrophysiology procedures are needed. Diagnostic and ablation procedures are difficult since catheter manipulation and positioning are more complex. We present here a case of successful atrioventricular nodal reentrant tachycardia (AVNRT) ablation in a patient with unexpected IVC agenesis, using an azygos route.
Case reportA 62-year-old woman was referred to our center for an electrophysiological study (EPS) and catheter ablation of a documented narrow QRS complex tachycardia. Written informed consent was obtained. Antiarrhythmic drugs were discontinued for more than five half-lives before the study. The initial ECG showed sinus rhythm with a normal PR interval and no delta waves.
A 6F quadripolar catheter and a 6F quadripolar deflectable diagnostic catheter (Xtrem, ELA Medical) were inserted via the right femoral vein and advanced through the IVC. When the catheters reached the cardiac silhouette, only far-field electrical activity could be recorded. The catheters were advanced further and eventually reached the right atrium via the superior vena cava (SVC) after making a loop outside the cardiac silhouette. The catheter routes suggested the absence of an IVC and the presence of an azygos vein joining the SVC. This diagnosis was confirmed by failure to advance the catheters retrogradely from the right atrium to the IVC.
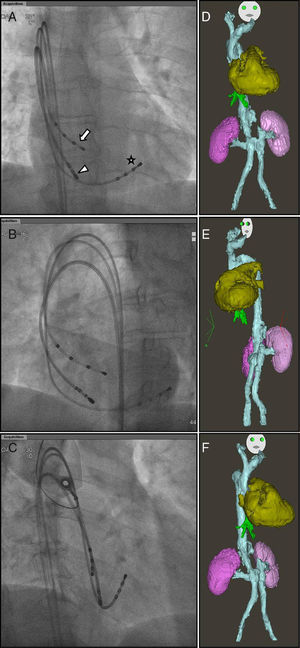
The catheters were then positioned in the His bundle and the coronary sinus, and a 4 mm tip standard radiofrequency ablation catheter (Cordis Webster, Baldwin Park, CA, USA) was successfully advanced through the azygos vein and positioned in the atria. Dual atrioventricular node conduction was exhibited and a supraventricular tachycardia compatible with AVNRT was reproducibly induced. The ablation catheter was then positioned in the posterior part of the triangle of Koch (Figure 1) and two 90 s radiofrequency lesions were performed (60°, 30 W). A stable junctional rhythm developed during the second energy application, and after ablation, no tachycardia could be induced at baseline or after isoproterenol infusion.
Fluoroscopic images in (A) anteroposterior (AP), (B) left anterior oblique (LAO) at 35°, and (C) right anterior oblique (RAO) at 30° views, showing the positioning of the His (arrow), coronary sinus (star) and ablation (arrowhead) catheters. Three-dimensional reconstructions were obtained after the procedure, showing suprarenal inferior vena cava agenesis, draining into the superior vena cava (blue), hepatic veins (green), heart (gold) and kidneys (purple), in AP, LAO and RAO views (D, E and F, respectively).
A computed tomography scan was performed after the procedure to better understand the patient's venous anatomy. Suprarenal IVC agenesis was confirmed and the infrarenal IVC continued as the azygos vein and joined the SVC at its normal location within the right paratracheal space. The hepatic veins drained directly into the right atrium. The patient was discharged from the hospital the following day without any medication and remained free of symptoms during a 12-month follow-up.
DiscussionAfter the eighth week of gestation the normal adult inferior vena cava (IVC) is complete. The development of the IVC is a complex process resulting from anastomoses between three pairs of embryonic veins that appear and regress: the posterior cardinal veins, the subcardinal veins, and the supracardinal veins. The final adult IVC is formed of four segments: hepatic (from the vitelline vein); suprarenal (from the subcardinal-hepatic anastomosis); renal (from the right supracardinal-subcardinal anastomosis); and infrarenal (from the right supracardinal vein).1 Several anomalies of the IVC can occur: (1) left IVC results from the regression of the right supracardinal vein and persistence of the left supracardinal vein. This variant occurs in 0.2-0.5% of the population and may be misdiagnosed as left para-aortic lymphadenopathy; (2) double IVC results from the persistence of the right and left supracardinal veins. It is one of the most common anomalies of the IVC, affecting 1-3% of the population. Usually, the left IVC ends at the level of the left renal vein and crosses over behind the aorta to drain into the right IVC; (3) azygos and hemiazygos continuation of the IVC is related to regression of the vitelline vein, which constitutes the hepatic segment of the IVC. Its prevalence is 0.6% of the population. In this case, the IVC ends above the renal veins and venous blood flows directly into the azygos or hemiazygos veins. The azygos vein then drains into the superior vena cava and finally into the right atrium. Independently, the hepatic veins empty directly into the right atrium.2 These anomalies may be isolated or associated with other congenital diseases such as polysplenia, dextrocardia, single ventricle or atrium, and cyanotic or acyanotic congenital heart disease. For patients with isolated interruption of the IVC and no clinical manifestations, no treatment is needed.2–4
In this report, we describe a case of successful radiofrequency catheter ablation of AVNRT in a patient with interruption of the IVC and azygos continuation. In the presence of such an anomaly, access to the right atrium by a femoral approach is still possible, through the azygos vein and the superior vena cava. As a result, manipulation and positioning of the catheters may more difficult due to the longer and more tortuous course of the catheters, but access to the different cardiac structures is achievable, allowing mapping and ablation of different supraventricular and ventricular arrhythmias. However, this approach is often associated with increased fluoroscopy radiation exposure and may cause patient discomfort, the catheter frequently being caught in the azygos vein.5 There are a few reported cases of ablation of arrhythmias in patients with IVC interruption, including AVNRT,6 accessory pathways,7 common atrial flutter,5 atrial fibrillation,8 and right ventricular ectopies.9 Other routes have been described in the literature to access cardiac structures in patients with interruption of the IVC, including a superior approach via the jugular or subclavian vein10 or a percutaneous transhepatic venous approach.11 Electroanatomical mapping systems may also help to perform ablations safely in such patients.6
ConclusionInterruption of the IVC is uncommon but may be encountered during electrophysiology procedures. Ablation of cardiac arrhythmias, including AVNRT as shown in this case, can be safely performed using an azygos route through the femoral approach.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.