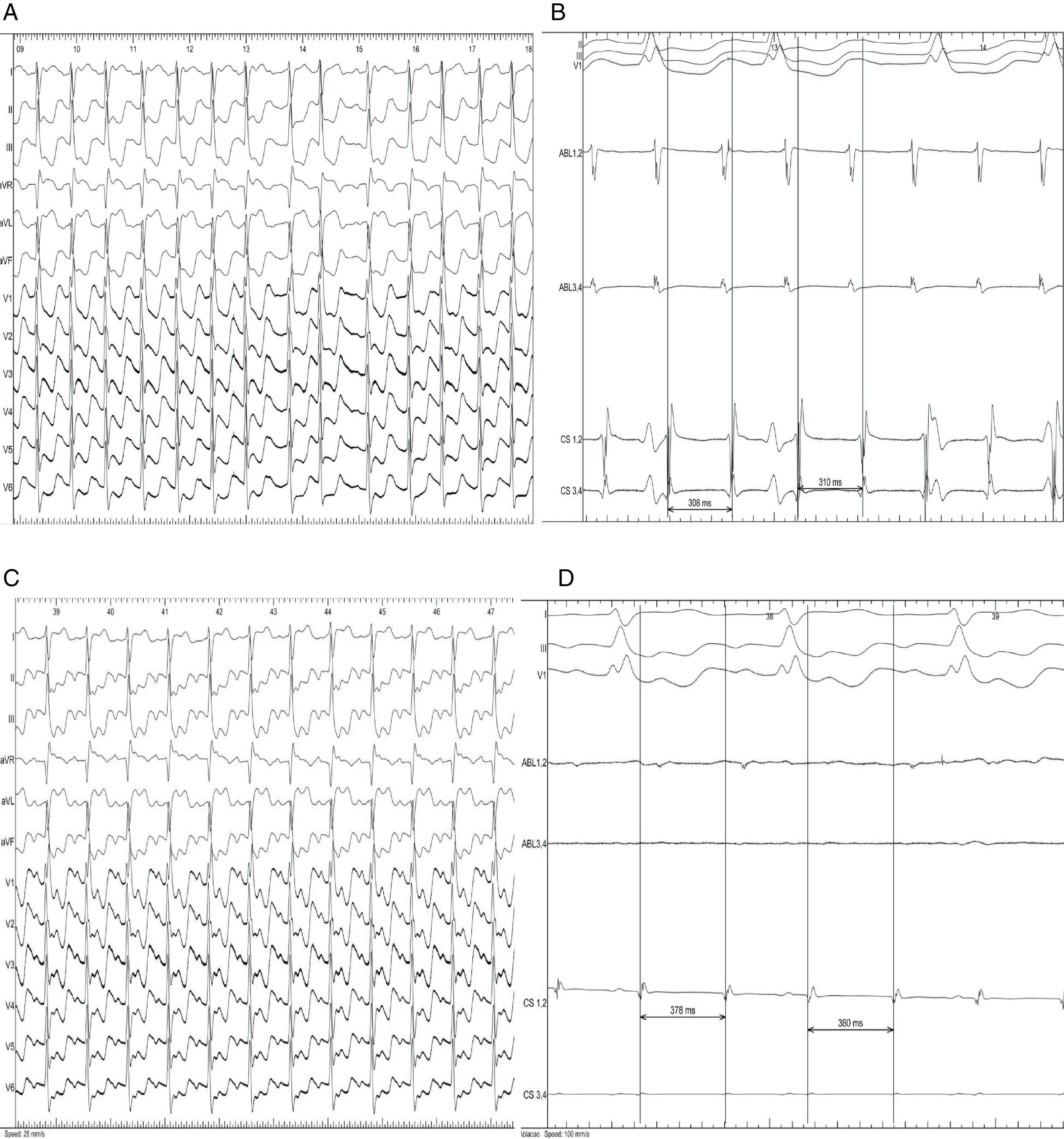
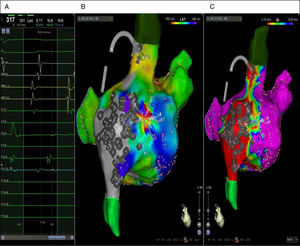
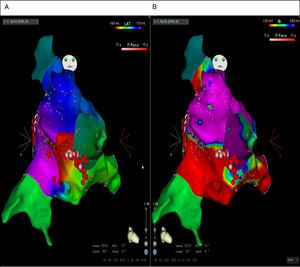
The authors describe the case of a 57-year-old woman with surgically treated superior vena cava sinus-venosus atrial septal defect who underwent an electrophysiology study with the CARTO® 3 mapping system (Biosense Webster, J&J) due to recurrent episodes of tachycardia. The patient was found to be in narrow QRS-complex tachycardia, with a cycle length of 310 ms and concentric activation sequence in the coronary sinus (Figure 1A and 1B), suggesting atrial tachycardia (AT) originating from the right atrium (RA). High-density electroanatomical mapping of the RA was performed using the PentaRay catheter (Figure 2C).
12-lead electrocardiogram (A) and intracavitary electrogram (B) of the clinical tachycardia. The tachycardia cycle length is 310 ms with a concentric activation sequence in the coronary sinus (CS 3-4 → CS 1-2). 12-lead electrocardiogram (C) and intracavitary electrogram (D) in counterclockwise atrial flutter. The baseline tachycardia cycle length is 380 ms. ABL: ablation catheter; CS: quadripolar catheter in the coronary sinus.
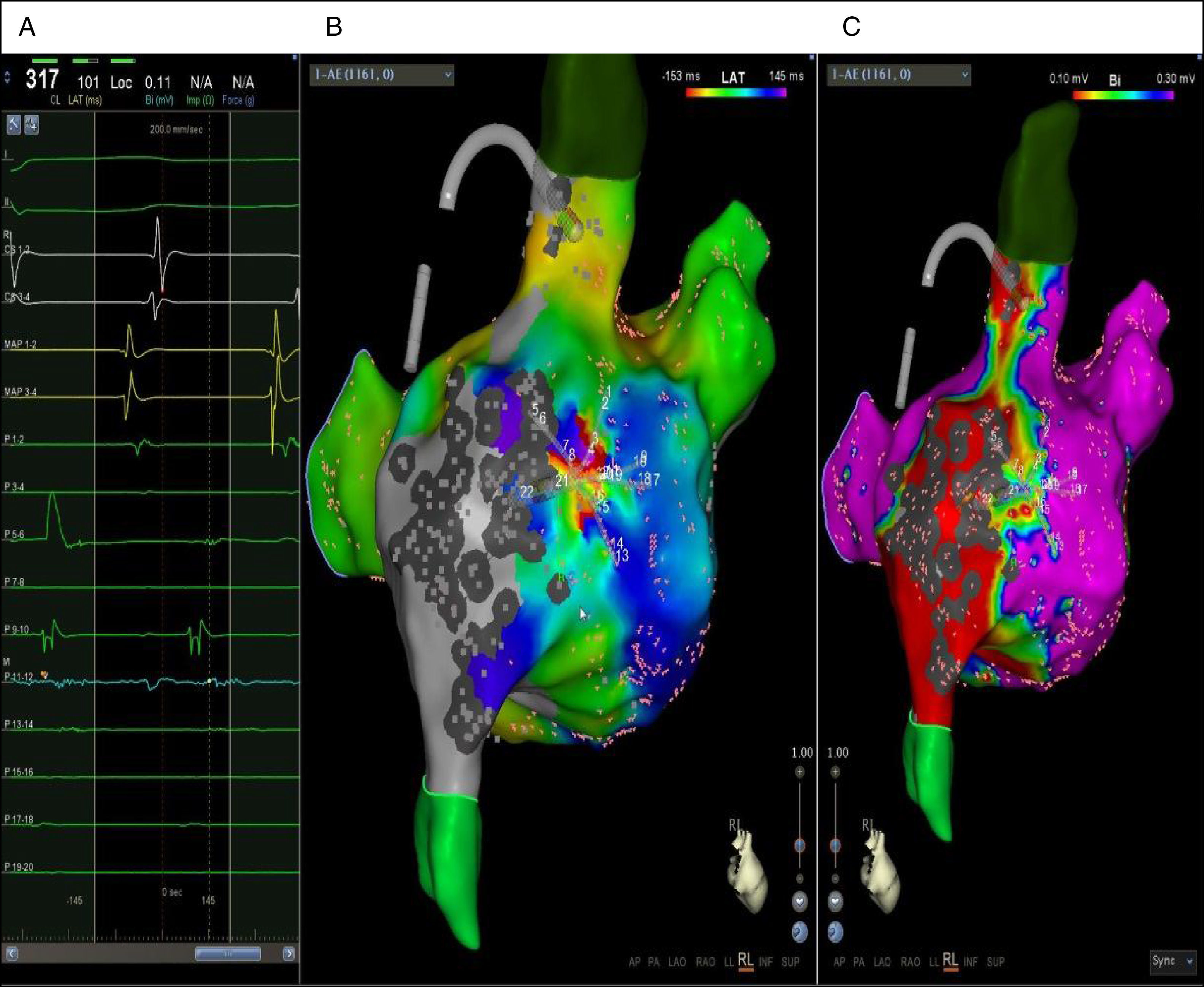
Intracavitary electrograms in the coronary sinus catheters (CS 1-2 and CS 3-4), mapping catheters (P 1-2 to P 19-20) and SmartTouch ablation catheters (MAP 1-2 and MAP 3-4) (A). PentaRay mapping catheter revealed ≥75% of the tachycardia cycle (from bipole P 1-2 to bipole P 11-12), compatible with a micro-reentry circuit. RA anatomy was mapped using the pentapolar PentaRay catheter (Biosense Webster, J&J), which enables faster anatomy mapping due to its 20 electrodes. A SmartTouch ablation catheter (Biosense Webster, J&J) with contact sensor was selected to ensure good contact with the dilated right atrium. Both the activation (B) and voltage (C) maps of the clinical atrial tachycardia were acquired using Confidence software, which automatically records points. The locations with voltage ≤0.1 mV were defined as scar (colored red) in the voltage map (C).
The AT activation map (Figure 2B) indicated micro-reentry and centrifugal activation mainly on the lateral RA wall (Figure 2B), coinciding with the border zone of the scar (Figure 2C) and reveals ≥75% of the tachycardia cycle on the PentaRay catheter (Figure 2A). Radio frequency was applied with the SmartTouch ablation catheter in the initial activation region, resulting in conversion to sinus rhythm (SR).
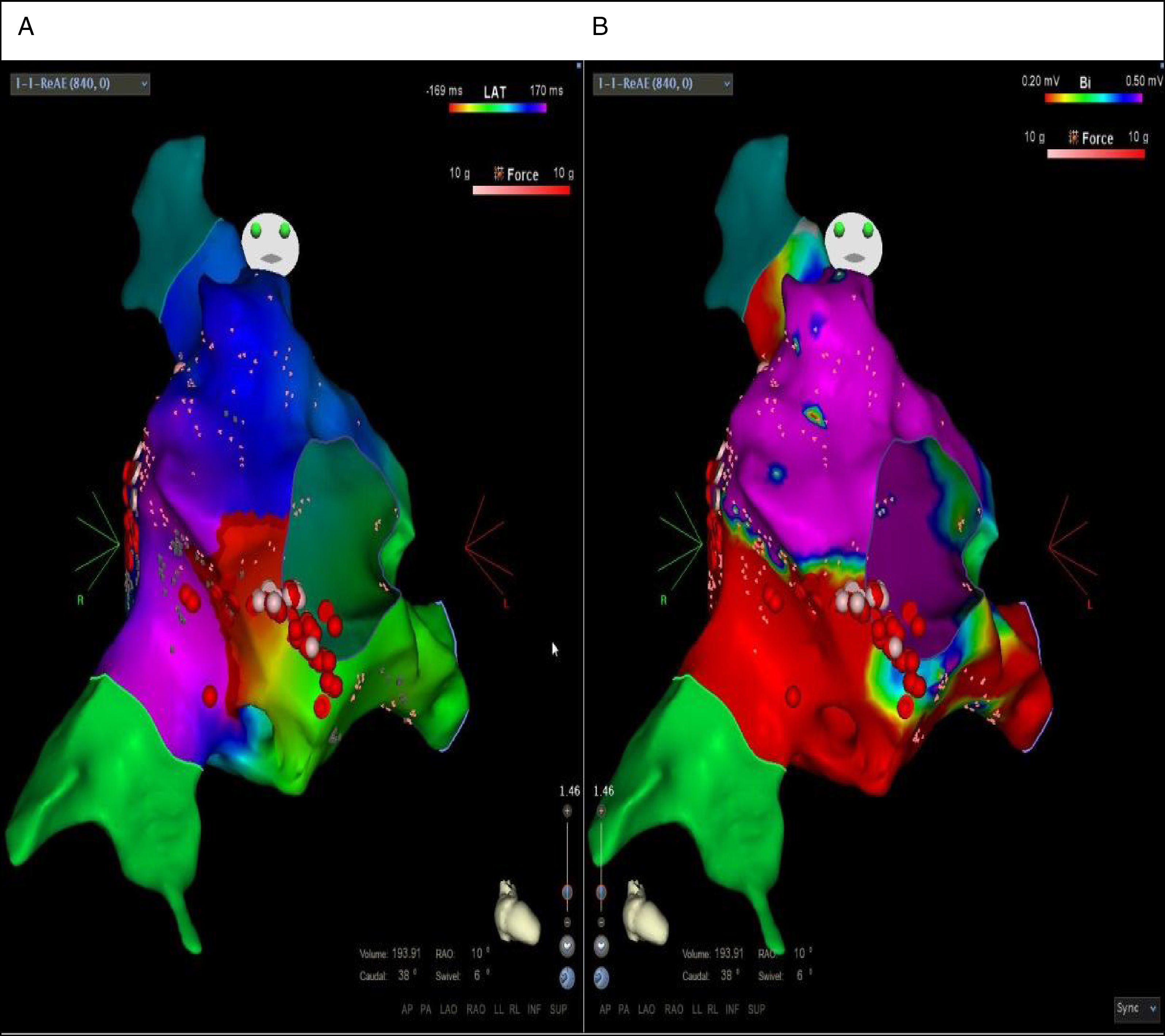
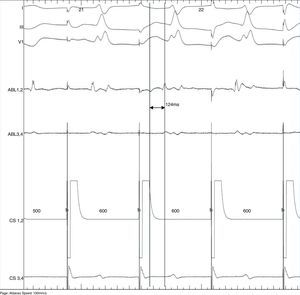
Under rapid atrial pacing, tachycardia was again induced, with a surface electrocardiogram indicative of counterclockwise atrial flutter with a cycle length of 380 ms (Figure 1C and 1D) confirmed by activation and voltage remapping (Figure 3A and 3B).
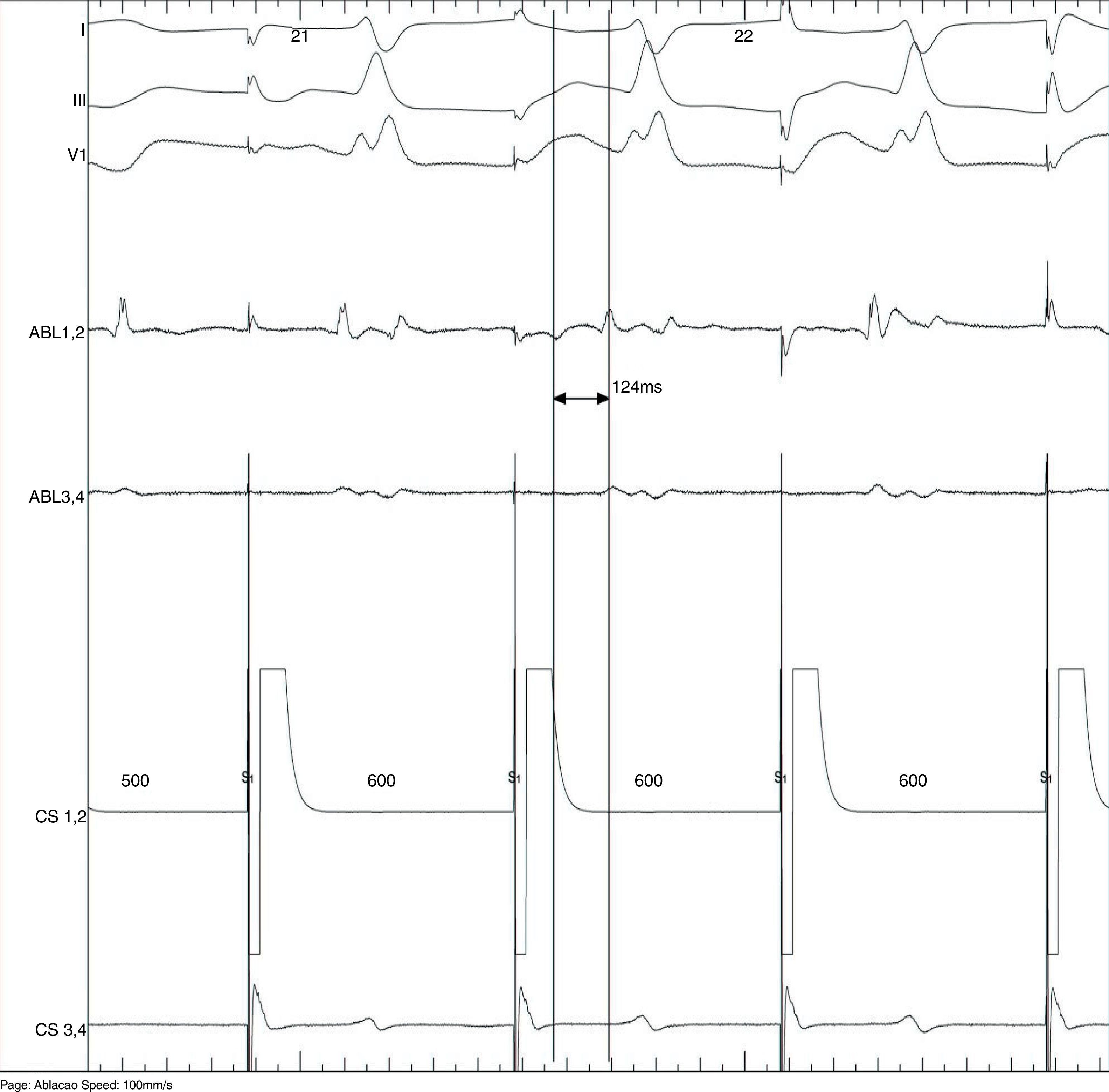
Cavotricuspid isthmus (CTI) ablation was performed resulting in conversion to SR. Bidirectional block and the presence of double potential along the CTI line (Figure 4) were confirmed.
This case shows the advantages of using mapping in patients with congenital heart disease, given that fibrosis in this context enables having several tachycardia circuits.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Amaral ME, Sousa PA, António N, et al. Ablação de taquicardia auricular em cardiopatía congénita operada. Rev Port Cardiol. 2018;37:271–275.