To assess the association between a comprehensive smoking ban and hospitalization rates for acute myocardial infarction (AMI).
MethodsAn observational study was conducted to assess changes in hospital admission rates for AMI in the Autonomous Community of Valencia, Spain (population 5 million), during the period 1995-2013. Law 28/2005 prohibited smoking in all enclosed spaces (public and private), and Law 42/2010 extended the ban to bars and restaurants as well as children's playgrounds and access areas of schools and hospitals. Data on hospital admissions were obtained from the Hospital Discharge Database (CMBD) of the Autonomous Community. Annual hospital admission rates per 100000 population for AMI (ICD-9-CM code 410) for men and women were calculated.
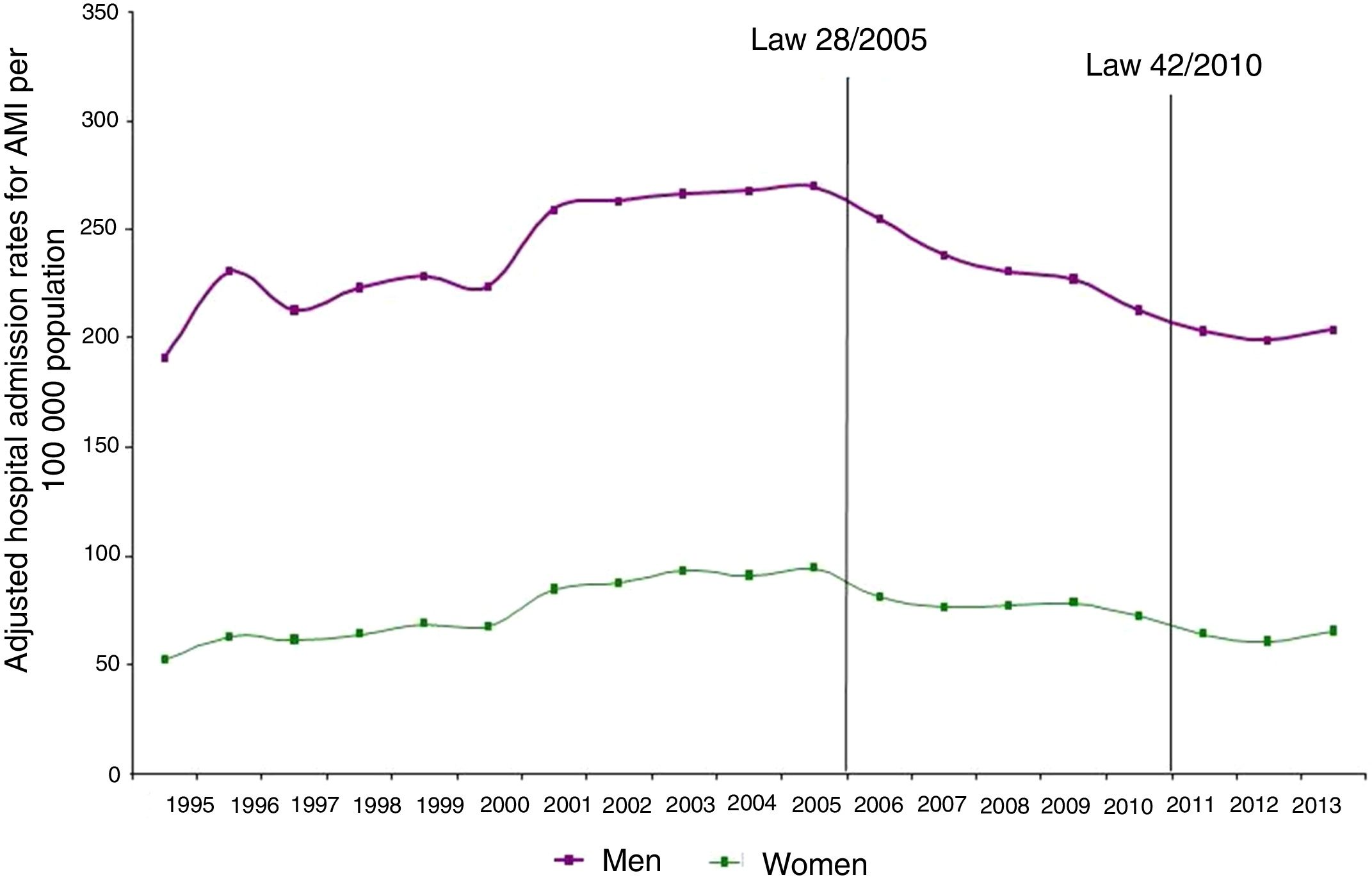
ResultsAdjusted hospital admission rates per 100000 population for AMI decreased markedly from 141.1 in 2005 to 119.2 in 2007, with a further reduction to 102.9 in 2013. Reductions in hospital admission were recorded in both men and women, but the downward trends were stronger in women.
ConclusionThe Spanish comprehensive smoking ban was associated with a marked reduction in the adjusted rate of hospital admissions due to AMI in the Autonomous Community of Valencia. This decrease in the number of persons requiring in-patient care due to AMI is important from both a health care and a societal perspective.
Avaliar a associação entre a proibição total do tabagismo nas taxas de internação hospitalar por enfarto agudo do miocárdio (EAM).
MétodosFoi feito um estudo observacional para avaliar as mudanças nas taxas de internação hospitalar por IAM na Comunidade Autónoma de Valência, Espanha (população de 5 milhões de pessoas), de 1995-2013. A Lei 28/2005 proibiu fumar em todos os locais fechados (públicos e privados) e culturais e a lei 42/2010 estendeu a proibição ao fumo em bares e restaurantes, bem como em parques infantis e pontos de acesso a escolas e hospitais. Os dados dos internamentos hospitalares foram obtidos a partir do Conjunto Básico Mínimo de Dados Obrigatórios (CMBD) da Comunidade Autónoma. Foram calculadas as taxas anuais de internamento hospitalar por 100.000 habitantes para o IAM (CID-9-MC código 410) para homens e mulheres.
ResultadosAs taxas de internamento hospitalar ajustadas por 100000 habitantes para o EAM diminuíram acentuadamente de 141,1/100000 habitantes em 2005 para 119,2/100.000 habitantes em 2007, com uma redução ainda maior para 102,9/100000 habitantes em 2013. Reduções na admissão hospitalar foram registradas para homens e mulheres, mas as tendências de redução foram maiores nas mulheres.
ConclusãoA proibição abrangente do tabagismo na Espanha foi associada a uma redução notável da taxa ajustada de internamentos hospitalares por 100 000 habitantes devido a AMI na Comunidade Autónoma de Valência. A diminuição do número de pessoas que necessita de atendimento hospitalar por causa do IAM é relevante do ponto de vista da saúde e da sociedade.
Comprehensive smoke-free legislation has been implemented in many countries, with the greatest progress since 2007. However, despite declines in overall smoking prevalence in some regions,1,2 there are alarming trends in tobacco use among youth and in low-income countries.3 The harmful effects of tobacco are not confined to active smokers, but also impact those exposed to secondhand smoke, which is listed as the third leading cause of preventable poor health and premature death in the developed world.4 Despite compelling evidence of the benefits of laws and policies that prohibit smoking in workplaces and other public spaces, only 16% of the world's population is covered by comprehensive smoke-free legislation.5
Reductions in exposure to secondhand tobacco smoke have been shown to diminish the risk for cardiovascular disease, including acute myocardial infarction (AMI).1,6–9 In a recent Cochrane review of 77 studies that reported legislative smoking bans affecting populations, consistent temporal trends were observed with evidence of significant reductions in admissions due to AMI and acute coronary syndrome following the introduction of national smoking bans.2 Cardiovascular benefits following the enactment of smoke-free laws have been consistently reported in other systematic reviews and primary studies carried out in different countries.7,10–17
It may therefore be expected that anti-smoking regulations designed to reduce exposure to secondhand smoke would have a positive effect on decreasing hospital admission rates due AMI in our region. The present observational study was designed to assess changes in hospital admission rates for AMI due to smoking-related disease in the Autonomous Community of Valencia, Spain, between 1995 and 2013.
MethodsThis study was conducted to compare the rates of hospital admission of patients with smoking-related AMI in the Autonomous Community of Valencia before and after implementation of two successive nationwide smoking bans. The Autonomous Community of Valencia is the fourth most populous Spanish region after Andalusia, Catalonia and Madrid, with more than 4.9 million inhabitants (2017 census) and more than 212 people per km2. It is located along the Mediterranean coast in the south-east of the Iberian peninsula, and covers an area of 23 259km2 (4.6% of the country). One third of the population live in the capital city, Valencia, which is Spain's third largest city.
Spain became a party to the WHO Framework Convention on Tobacco Control on April 11, 2005. In 2005, the Spanish government approved Law 28/2005, the primary law governing smoking in public places and tobacco advertising, promotion and sponsorship. This was substantially amended in 2010 by Law 42/2010, which mandated a ban on smoking in indoor public places, indoor workplaces, and public transportation, and repealed provisions that permitted designated smoking areas in hospitality venues. Other preventive measures were adopted: taxes on cigarettes were raised, and more resources were made available for prevention and treatment, as well as information campaigns and an intensive social debate on smoking.
Data on hospital admissions were obtained from the Hospital Discharge Database (CMBD) of the Community of Valencia. The Decree of October 8, 1992 of the Regional Council of Health and Consumption established the requirement for all public and private health care centers of the Autonomous Community of Valencia to collect a minimum basic data set for all patients attended for whom at least one admission was recorded. These data include age, gender and the main diagnosis, defined as the pathological condition responsible for the patient's hospital admission and established at hospital discharge. Diagnoses were coded according to the International Classification of Diseases, 9th revision, Clinical Modification (ICD-9-CM). For the purpose of this study, all data from the Hospital Discharge Databases of all hospitals of the Valencian Health Agency from 1995 to 2013 were used. Index admissions with ICD-9-CM code 410 (acute myocardial infarction) as the main diagnosis on hospital discharge were included. General population data by age and gender were obtained from the official census of the Autonomous Community of Valencia published annually by the National Institute of Statistics.
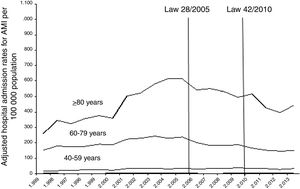
Statistical analysisAnnual hospital admission rates per 100000 population for smoking-related AMI (ICD-9-CM code 410) for men and women were calculated. Standardized rates were computed by the direct method using Epidat 3.1 software and taking the 2000 population as standard. To assess the impact of Law 28/2005 and Law 42/2010, a trend analysis of annual rates of hospital admission for AMI for the period 1995-2013 was performed by the linear least squares regression method. The same analysis was performed for the population age groups of 20-39 years, 40-59 years, 60-79 years and ≥80 years.
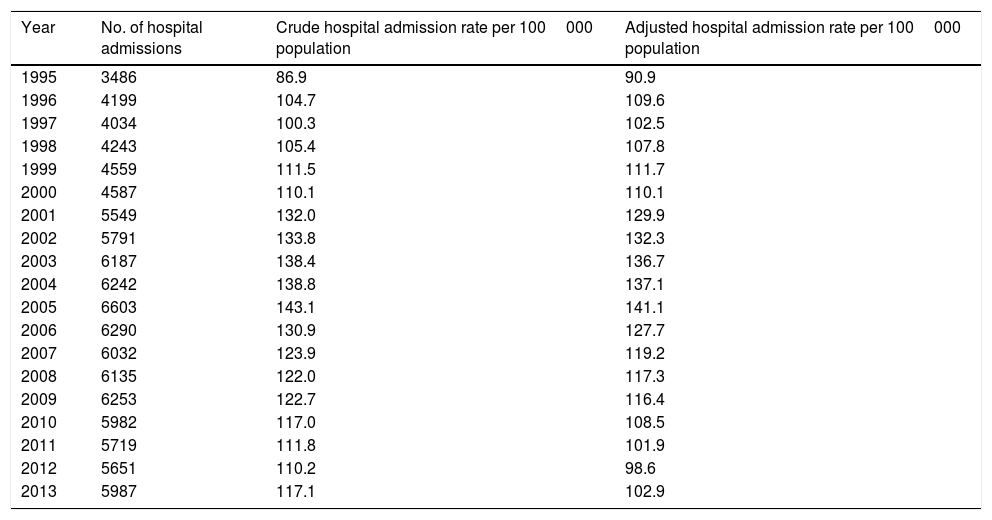
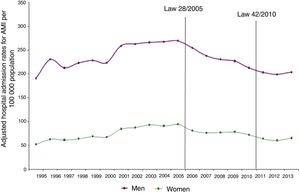
ResultsA total of 22 339 patients over 20 years of age diagnosed with AMI were assessed during an observation period of 19 years. Both crude and adjusted hospital admission rates per 100000 population decreased sharply after the anti-smoking laws (Table 1). The crude hospital admission rate was 143.1/100000 population in 2005, 123.9 in 2007, and 117.1 in 2013, an overall decrease of 18.2%. The adjusted hospital admission rate also decreased from 141.1/100000 population in 2005 to 102.9 in 2013, a reduction of 27%.
Overall hospital admissions and crude and adjusted admission rates per 100000 population for acute myocardial infarction in the Autonomous Community of Valencia.
| Year | No. of hospital admissions | Crude hospital admission rate per 100000 population | Adjusted hospital admission rate per 100000 population |
|---|---|---|---|
| 1995 | 3486 | 86.9 | 90.9 |
| 1996 | 4199 | 104.7 | 109.6 |
| 1997 | 4034 | 100.3 | 102.5 |
| 1998 | 4243 | 105.4 | 107.8 |
| 1999 | 4559 | 111.5 | 111.7 |
| 2000 | 4587 | 110.1 | 110.1 |
| 2001 | 5549 | 132.0 | 129.9 |
| 2002 | 5791 | 133.8 | 132.3 |
| 2003 | 6187 | 138.4 | 136.7 |
| 2004 | 6242 | 138.8 | 137.1 |
| 2005 | 6603 | 143.1 | 141.1 |
| 2006 | 6290 | 130.9 | 127.7 |
| 2007 | 6032 | 123.9 | 119.2 |
| 2008 | 6135 | 122.0 | 117.3 |
| 2009 | 6253 | 122.7 | 116.4 |
| 2010 | 5982 | 117.0 | 108.5 |
| 2011 | 5719 | 111.8 | 101.9 |
| 2012 | 5651 | 110.2 | 98.6 |
| 2013 | 5987 | 117.1 | 102.9 |
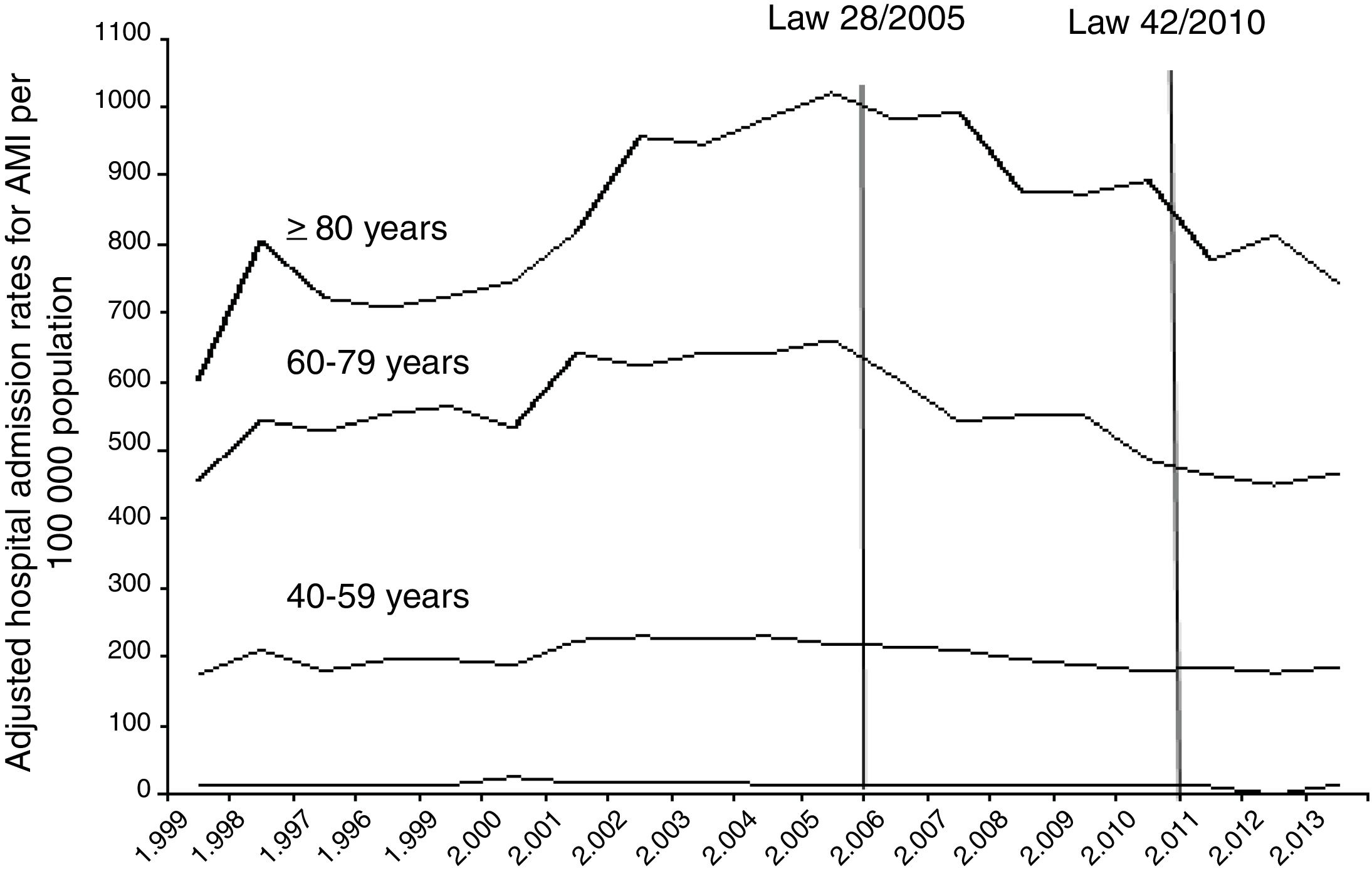
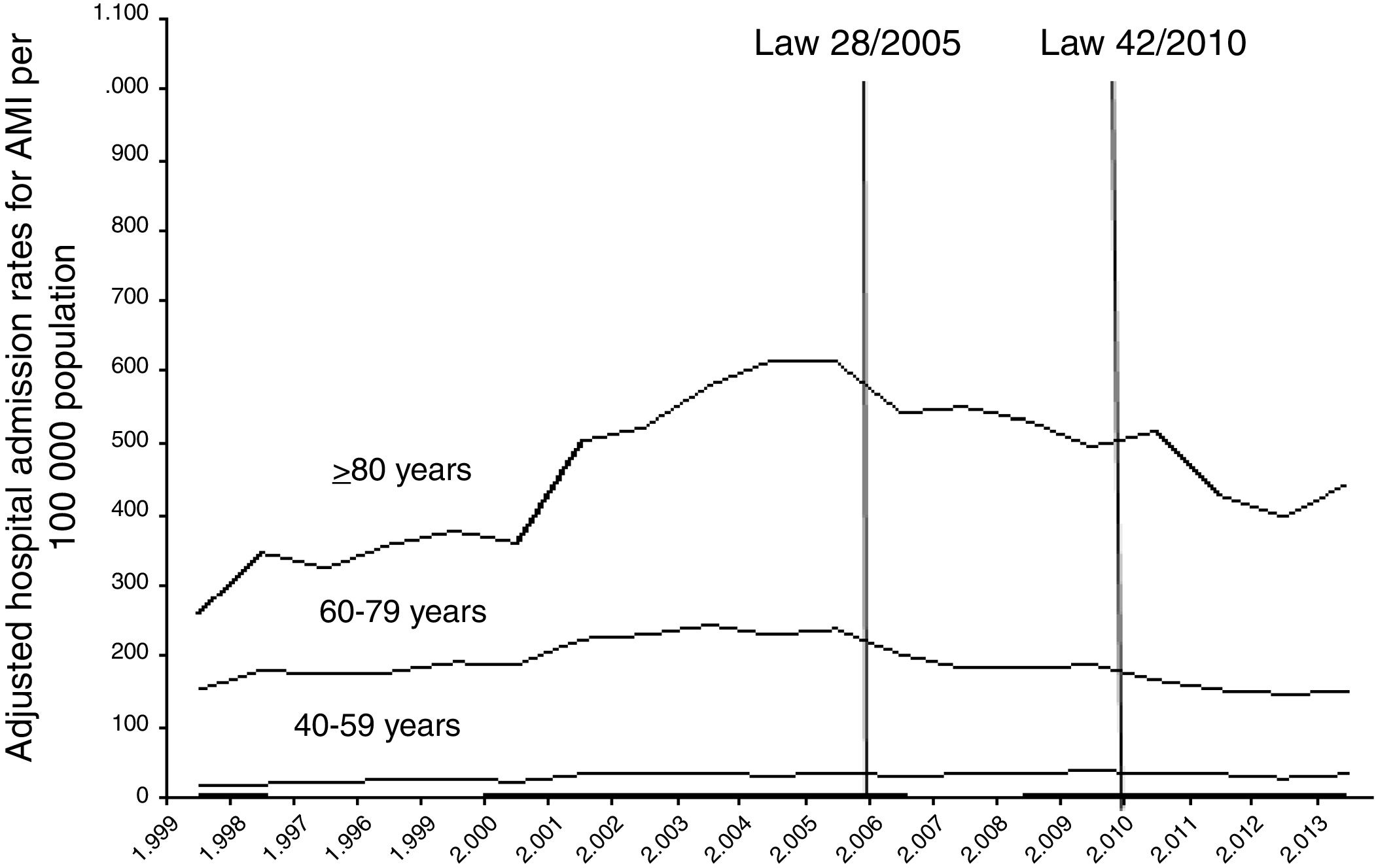
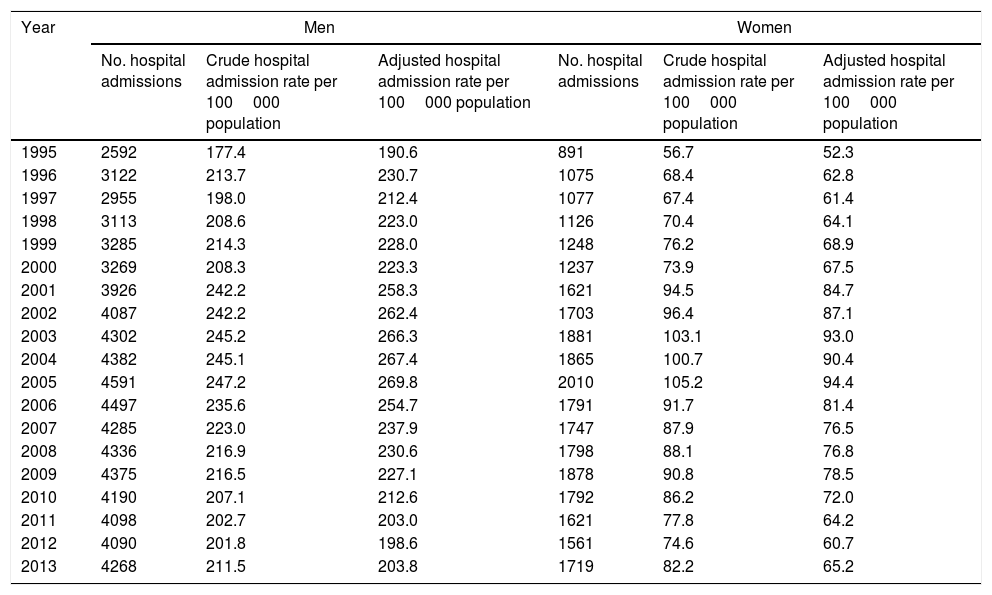
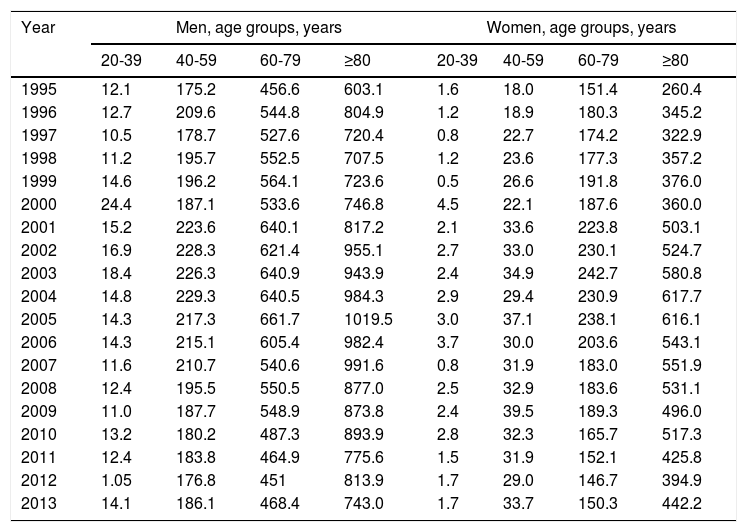
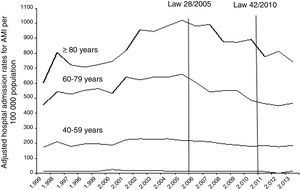
Similar trends were found for men and women, although reductions were more marked among women (Table 2 and Figure 1). Between 2005 and 2010, hospital admission rates per 100000 population for AMI showed a 24.5% decrease in men vs. 30.9% in women. Also, when men and women admitted for AMI were stratified by age group (Table 3), decreasing trends were observed in all age groups in both men and women between 2006 and 2009 after Law 28/2005, but after Law 42/2010, admission rates increased slightly in men in all age groups except for older people (≥80 years), in whom admission rates decreased from 813.9/100000 population in 2012 to 743.0 in 2013 (Figure 2). In contrast, changes in admission rates for AMI after 2011 in women showed a slightly increasing trend in all age groups, particularly 60-79 years and ≥80 years (Figure 3).
Overall hospital admissions and crude and adjusted admission rates per 100000 population for acute myocardial infarction in men and women during the study period.
| Year | Men | Women | ||||
|---|---|---|---|---|---|---|
| No. hospital admissions | Crude hospital admission rate per 100000 population | Adjusted hospital admission rate per 100000 population | No. hospital admissions | Crude hospital admission rate per 100000 population | Adjusted hospital admission rate per 100000 population | |
| 1995 | 2592 | 177.4 | 190.6 | 891 | 56.7 | 52.3 |
| 1996 | 3122 | 213.7 | 230.7 | 1075 | 68.4 | 62.8 |
| 1997 | 2955 | 198.0 | 212.4 | 1077 | 67.4 | 61.4 |
| 1998 | 3113 | 208.6 | 223.0 | 1126 | 70.4 | 64.1 |
| 1999 | 3285 | 214.3 | 228.0 | 1248 | 76.2 | 68.9 |
| 2000 | 3269 | 208.3 | 223.3 | 1237 | 73.9 | 67.5 |
| 2001 | 3926 | 242.2 | 258.3 | 1621 | 94.5 | 84.7 |
| 2002 | 4087 | 242.2 | 262.4 | 1703 | 96.4 | 87.1 |
| 2003 | 4302 | 245.2 | 266.3 | 1881 | 103.1 | 93.0 |
| 2004 | 4382 | 245.1 | 267.4 | 1865 | 100.7 | 90.4 |
| 2005 | 4591 | 247.2 | 269.8 | 2010 | 105.2 | 94.4 |
| 2006 | 4497 | 235.6 | 254.7 | 1791 | 91.7 | 81.4 |
| 2007 | 4285 | 223.0 | 237.9 | 1747 | 87.9 | 76.5 |
| 2008 | 4336 | 216.9 | 230.6 | 1798 | 88.1 | 76.8 |
| 2009 | 4375 | 216.5 | 227.1 | 1878 | 90.8 | 78.5 |
| 2010 | 4190 | 207.1 | 212.6 | 1792 | 86.2 | 72.0 |
| 2011 | 4098 | 202.7 | 203.0 | 1621 | 77.8 | 64.2 |
| 2012 | 4090 | 201.8 | 198.6 | 1561 | 74.6 | 60.7 |
| 2013 | 4268 | 211.5 | 203.8 | 1719 | 82.2 | 65.2 |
Adjusted admission rates per 100000 population for acute myocardial infarction in men and women according to age during the study period.
| Year | Men, age groups, years | Women, age groups, years | ||||||
|---|---|---|---|---|---|---|---|---|
| 20-39 | 40-59 | 60-79 | ≥80 | 20-39 | 40-59 | 60-79 | ≥80 | |
| 1995 | 12.1 | 175.2 | 456.6 | 603.1 | 1.6 | 18.0 | 151.4 | 260.4 |
| 1996 | 12.7 | 209.6 | 544.8 | 804.9 | 1.2 | 18.9 | 180.3 | 345.2 |
| 1997 | 10.5 | 178.7 | 527.6 | 720.4 | 0.8 | 22.7 | 174.2 | 322.9 |
| 1998 | 11.2 | 195.7 | 552.5 | 707.5 | 1.2 | 23.6 | 177.3 | 357.2 |
| 1999 | 14.6 | 196.2 | 564.1 | 723.6 | 0.5 | 26.6 | 191.8 | 376.0 |
| 2000 | 24.4 | 187.1 | 533.6 | 746.8 | 4.5 | 22.1 | 187.6 | 360.0 |
| 2001 | 15.2 | 223.6 | 640.1 | 817.2 | 2.1 | 33.6 | 223.8 | 503.1 |
| 2002 | 16.9 | 228.3 | 621.4 | 955.1 | 2.7 | 33.0 | 230.1 | 524.7 |
| 2003 | 18.4 | 226.3 | 640.9 | 943.9 | 2.4 | 34.9 | 242.7 | 580.8 |
| 2004 | 14.8 | 229.3 | 640.5 | 984.3 | 2.9 | 29.4 | 230.9 | 617.7 |
| 2005 | 14.3 | 217.3 | 661.7 | 1019.5 | 3.0 | 37.1 | 238.1 | 616.1 |
| 2006 | 14.3 | 215.1 | 605.4 | 982.4 | 3.7 | 30.0 | 203.6 | 543.1 |
| 2007 | 11.6 | 210.7 | 540.6 | 991.6 | 0.8 | 31.9 | 183.0 | 551.9 |
| 2008 | 12.4 | 195.5 | 550.5 | 877.0 | 2.5 | 32.9 | 183.6 | 531.1 |
| 2009 | 11.0 | 187.7 | 548.9 | 873.8 | 2.4 | 39.5 | 189.3 | 496.0 |
| 2010 | 13.2 | 180.2 | 487.3 | 893.9 | 2.8 | 32.3 | 165.7 | 517.3 |
| 2011 | 12.4 | 183.8 | 464.9 | 775.6 | 1.5 | 31.9 | 152.1 | 425.8 |
| 2012 | 1.05 | 176.8 | 451 | 813.9 | 1.7 | 29.0 | 146.7 | 394.9 |
| 2013 | 14.1 | 186.1 | 468.4 | 743.0 | 1.7 | 33.7 | 150.3 | 442.2 |
This observational study shows that two successive anti-smoking laws implemented in 2005 and 2010 were associated with a marked reduction in crude and adjusted hospital admission rates for AMI in the fourth most populous autonomous community in Spain. Crude and adjusted hospital admission rates for men and women were also analyzed, and showed marked decreases in women. Decreasing trends in men and women stratified by age were found between 2006 and 2009, although after 2011 slightly increasing trends in both men and women were observed, except for the oldest old age group. The reason for this decreasing trend in people aged ≥80 years following the more restrictive 42/2010 smoking ban is difficult to ascertain. The report by the US Department of Health and Human Services on 50 years (1964-2014) of changes in the health consequences of smoking16 presents a review of the evidence (using nonrandomized comparisons including interrupted time series analysis18) of the impact of smoke-free laws on acute cardiovascular events. Studies reporting results stratified by age found no significant decline in AMI among older patients (median cutoff 70 years of age) following the implementation of comprehensive smoke-free laws. However, the observed reductions in AMI hospitalization rates following implementation of smoke-free laws were very similar for males and females.16 Interestingly, no progressive reduction in AMI risk associated with increasing time since a smoke-free law was implemented was observed.16 In the 2010 report of the Committee on Secondhand Smoke Exposure and Acute Coronary Events of the US Institute of Medicine,19 an analysis of 11 key epidemiological studies showed remarkable consistency, with decreases in the rate of AMI after implementation of smoking bans, ranging from about 6% to 47%, depending on the study and the form of analysis. Also, an analysis of admission rates for acute coronary events in 20 Italian regions from January 2002 to November 2006 found a reduction in hospital admissions in both men and women aged under 70 in the two years following the introduction of a comprehensive smoking ban in Italy.20 The spread of strict non-smoking policies provides evidence that both direct smoking and passive smoking are important targets for reducing AMI-related hospital admissions. Although there have been consistent improvements in secular trends for long-term survival and outcomes after AMI, survivors remain at higher risk than the general population, particularly if they have additional risk factors such as older age, hypertension, or diabetes, all of which lead to worse outcomes.21
A national smoking ban implemented in 2005 in Denmark was associated with a significant reduction in the number of AMI admissions only one year after implementation and after adjustment for the incidence of type 2 diabetes.22 Numerous studies have shown a decrease in the incidence of AMI after implementation of smoking bans,9,23–25 which has been confirmed by systematic reviews and meta-analyses.1,10,16,26
It is also true that significant reductions in AMI risk may be partially attributable to reduced smoking prevalence. In a systematic review and meta-analysis of epidemiological studies examining how legislation prohibiting smoking in indoor public places impacts the risk of acute coronary events, in areas where reductions in smoking prevalence post-legislation were above the mean there was a 14% reduction in events compared to 10% in areas below the mean.10 However, according to a recent Cochrane review,2 although evidence of an impact of smoking bans on smoking prevalence and tobacco consumption is inconsistent, there is robust evidence that the introduction of a legislative smoking ban does lead to improved health outcomes through reduction in secondhand smoking for countries and their populations, with the clearest evidence observed in reduced admissions for acute coronary syndrome.
Interestingly, in our study reductions in hospitalization rates were greater in women than in men. This finding is consistent with a study carried out in in Lexington, Kentucky, USA, after the passage of a smoke-free law, in which hospitalizations for AMI among men and women 40 months prior to and 32 months after enactment of the law were assessed.27 Among women, hospitalizations declined by 23% after the law took effect, whereas the rate of AMI among men did not change significantly. The authors attributed the difference to over-representation of women in the hospitality industry and a disproportionate number of men working in manufacturing facilities and government worksites not covered by the law.27 It has been suggested that smoke-free laws may be more protective for women, given the possibility that they may be more sensitive than men to tobacco smoke.28,29 The exact mechanisms involved in gender differences are unclear, but the anti-estrogenic effect of tobacco smoke has been implicated.29
Our data were not adjusted for confounders and secondhand smoke exposure was not assessed, but they do show changes that occurred in a large population of a Spanish Autonomous Community associated with the implementation of partial and complete smoking bans over a six-year period. The prevalence of tobacco consumption was not assessed and this is a limitation of the study. Also, adjustment for other major risk factors for AMI such as dyslipidemia, hypertension, diabetes, or obesity was not carried out. In a serial cross-sectional study from 2003 to 2009 performed in 21 primary health care centers in Madrid, a statistically significant rising trend for prevalence of diagnosed hypertension was found.30 Moreover, the percentage of hypertensive patients receiving pharmacological treatment who reached blood pressure targets increased over the period 2003-2009. These changes occurred at the same time as the nationwide implementation of the first smoking ban in 2005. In our study, there are no data on consequent reductions in smoking prevalence that would support the effect of smoking bans on the incidence of AMI.
In summary, the Spanish comprehensive smoking ban was associated with a marked reduction in the adjusted rate of hospital admissions due to AMI in the Autonomous Community of Valencia. The decrease in the number of persons requiring in-patient care due to AMI is important and may be viewed as an improvement in public health. However, comprehensive approaches to reduce the prevalence of smoking should be pursued in order to increase public awareness of the harmful effects of tobacco use.
Patient consentNot requiredContributors: F.C-V. conceived the study, collected data and wrote the manuscript. J.Q-I: contributed to the study design and collected data. C. González-Monte conducted the statistical analysis and contributed to the interpretation of data. F. Taberner-Alberola contributed to the study design and collected data. J.A. Lluch-Rodrigo contributed to the study design and collected data. All authors reviewed the manuscript and approved the final draft.
What this paper adds- •
Reduced admissions for acute coronary syndrome have been consistently documented after implementation of nationwide anti-smoking policies.
- •
As a result of this study carried out in Valencia, the fourth most populous Autonomous Community in Spain, it is clear that the comprehensive smoking ban was associated with a marked reduction in the adjusted rate of hospital admissions due to AMI.
- •
The decreasing trends were observed in both men and women, although reductions were more marked among women.
- •
The reduction in the number of individuals requiring in-patient care because of AMI is important and may be viewed as an improvement in public health as a result of implementation of smoke-free laws.
The authors have no conflicts of interest to declare.
The authors thank Marta Pulido, MD, for editing the manuscript and for her editorial assistance, and Renan Devita, MD, for his translation of the abstract into Portuguese. No funding for this study was received.