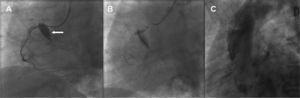
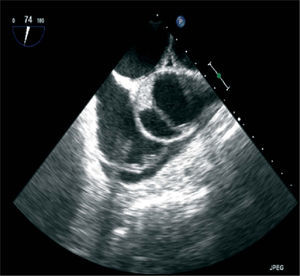
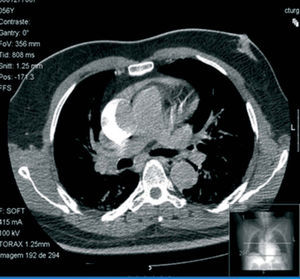
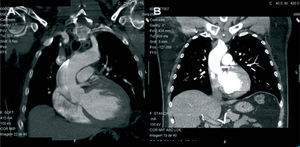
A 56-year-old man was admitted to our hospital for elective coronary angioplasty of a chronic total occlusion (CTO) of the right coronary artery (RCA). After insertion of a right femoral sheath, the RCA was engaged with a 6 French Amplatz AL-2 (Cordis, Miami, Fl, USA) guiding catheter. Recanalization was begun using a 0.014-inch Miracle 3 guidewire (Asahi Intecc, Japan). At this stage, an ostial dissection flap of the RCA with immediate retrograde extension to the ascending aorta was noticed (Figure 1). Stenting of the RCA ostium with a Xience Prime 3.0 × 15mm stent (Abbott Vascular, Santa Clara, California, USA) was performed, followed by a PTFE-covered 3.0 × 19mm Jostent graft (Jomed, Rangendingen, Germany), with apparent success. Transesophageal echocardiography showed a flap in the ascending aorta, extending up to the beginning of the aortic arch, with a partially thrombosed false lumen. No signs of pericardial effusion or aortic insufficiency were noted (Figure 2). A chest computed tomogram (CT) confirmed an ascending thoracic aorta dissection with a thrombosed false lumen 18mm in diameter, sparing the aortic arch (Figures 3 and 4A). The patient was admitted to the coronary care unit with mild chest pain but hemodynamically stable. He was managed conservatively. At the three-month follow-up visit, he was asymptomatic and the chest CT revealed complete resolution of the aorta parietal hematoma (Figure 4).
Iatrogenic aortocoronary dissection during percutaneous coronary intervention in patients with CTO is a rare but well-recognized complication1,2. In a retrospective study, the overall incidence was 0.02%3. It is typically associated with attempts to recanalize the RCA. This artery has a tortuous anatomy and smaller size, which make crossing the lesions more difficult and can predispose to iatrogenic dissection4. Furthermore, the RCA seems to be more prone to retrograde dissection than the left coronary artery, since its periostial wall and sinotubular junction are formed of less smooth muscle cells and a looser matrix of type I collagen fibers5. Other potential risk factors include calcification of the aortic root and the coronary lesion site. The type of catheter can also be implicated. The choice of an Amplatz catheter, which provides superior backup support, must be weighed against the associated higher incidence of coronary dissection.
Management of coronary dissection extending to the ascending aorta is challenging. Immediate recognition of the retrograde propagation is critical in order to protect the RCA ostium by stenting. The decision whether to proceed with surgery depends on clinical and hemodynamic stability. Several case reports describe a conservative approach, but a significant publication bias cannot be excluded6. The decision to proceed surgically is straightforward when there is an unstable clinical condition such as myocardial infarction, aortic regurgitation, hemopericardium or progression of the aortic dissection into the main branches of the aorta. On the other hand, a “watch and wait” strategy is reasonable in the stable patient with expected long-term good results7.
Cardiologists must keep in mind dissection into the aortic root which, although rare, is a life-threatening complication of coronary angioplasty. Minimizing the risk by choosing appropriate catheters is critical. When it occurs, initial ostial stenting is crucial and an opportunity for conservative treatment. If it results in clinical instability, surgery is the only life-saving treatment option.