Antiphospholipid syndrome (APS) is an autoimmune coagulation disorder that manifests clinically as venous and arterial thrombosis, and may affect any tissue or organ. Coronary artery involvement, however, is very rare. Case reports in the literature describing patients with coronary acute syndrome and APS treated with coronary angioplasty show conflicting results.
We report an adult male patient with APS who presented with an acute myocardial infarction. Given the high risk of thrombosis in these patients, he was treated percutaneously with thrombectomy and abciximab. We review the few cases of coronary angioplasty in patients with APS reported to date. To our knowledge, this is the first case in which acute myocardial infarction due to thrombotic coronary occlusion was treated with thrombectomy and abciximab without stenting the artery.
A síndrome antifosfolipídica (SAF) é uma doença autoimune da coagulação que se manifesta clinicamente por tromboses venosas e arteriais, podendo afetar qualquer tecido ou órgão. Contudo, o envolvimento das artérias coronárias é extremamente raro. Os casos relatados na literatura de síndrome coronária aguda e de SAF tratados com intervenção coronária percutânea (ICP) apresentam resultados controversos.
Relata-se o caso de um doente do sexo masculino com SAF que se apresentou com um enfarte agudo do miocárdio (EAM). Dado o alto risco de trombose nestes doentes, optou-se por ICP com trombectomia e abciximab. Faz-se uma revisão dos poucos casos relatados na literatura de ICP em doentes com SAF. De acordo com a nossa pesquisa, este trata-se do primeiro caso publicado em que um doente com SAF e EAM devido a oclusão coronária trombótica foi tratado com trombectomia e abciximab, sem implantação de stent.
Antiphospholipid syndrome (APS) is an autoimmune coagulation disorder that manifests as recurrent venous or arterial thrombosis. High levels of antiphospholipid antibodies (anticardiolipin and/or lupus anticoagulant) are characteristic serologic markers. APS may affect any tissue or organ but coronary artery involvement is rare.1 We describe a patient with APS who presented with acute myocardial infarction, which was treated percutaneously with thrombectomy and abciximab. We discuss the option of not implanting a stent in this complication.
Case reportA 47-year-old male without standard coronary risk factors was admitted for chest pain of one hour's duration. Nine years earlier, he had had an inferior acute myocardial infarction and had received thrombolytic treatment with tenecteplase at another center. Coronary angiography at the time showed normal arteries. Four years later, he was readmitted for right pulmonary thromboembolism from a venous femoral popliteal thrombosis. Since this was a second thrombotic event, a thrombophilia study was undertaken. Lupus anticoagulant and cardiolipin antibody tests were positive but tests for other antibodies (including anti-ANA and anti-DNA) were negative. APS was diagnosed and treatment with pravastatin and acenocoumarol was started.
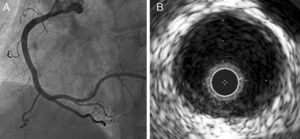
At admission to our center, five years later, an ECG showed inferior ST elevation of 2 mm and he was diagnosed with inferior acute myocardial infarction. Coronary angiography showed a normal left coronary artery and occlusion of the right coronary artery (Figure 1A). The INR was 1.3. Sodium heparin was given at doses of 1 mg/kg weight and a bolus of abciximab was administered at doses of 0.25 mg/kg, followed by an infusion of 0.125 μg/kg/min. After the occlusion was crossed with an angioplasty guidewire, the vessel was partially repermeabilized (Figure 1B), suggesting a thrombotic occlusion. Several thrombectomies were performed using an aspiration catheter (Export XT, Medtronic, Inc., Minneapolis, USA), and a large quantity of thrombotic material was extracted. After intracoronary sodium nitroprusside was given, minimal coronary luminal irregularities and TIMI III flow were observed (Figure 1C).
Since blood flow was restored and the patient had been diagnosed with APS, we decided not to implant a stent. Coronary angiography performed five days later showed that the luminal irregularities had improved. Intravascular ultrasound showed a mild concentric plaque with a minimal luminal diameter of 3.7 mm. No images of plaque rupture, ulcer or parietal thrombus were seen (Figure 2). Peak creatinine phosphokinase was 609 U/l. The erythrocyte sedimentation rate was 18 mm/h and C-reactive protein level was 6.1 mg/l. During hospitalization, the patient received enoxaparin at doses of 1 mg/kg every 12 hours via a subcutaneous route and double oral antiplatelet therapy (aspirin 100 mg/d and clopidogrel 75 mg/d). Acenocoumarol (target INR 2–3) was prescribed and the patient was discharged. Double antiplatelet therapy was continued for three months, and acenocoumarol, aspirin (100 mg) and atorvastatin (80 mg) were then given indefinitely. Stress testing was negative at 3, 12 and 24 months. After discharge the patient frequently had INR outside the therapeutic range, which was resolved with an anticoagulation self-monitoring device and telephone counseling by the Hemostasis and Thrombosis team.
DiscussionIn patients with APS, myocardial ischemia is usually caused by a thrombus and is related to antiphospholipid antibodies. Some patients may also have coronary stenosis due to associated atheromatous plaque. In the literature, results after treatment of ST-elevation acute coronary syndrome in patients with antiphospholipid syndrome are variable. Isolated thrombolysis,2 balloon angioplasty associated with thrombolytic therapy3 and stent implantation4–5 reportedly yield good results in some patients. However, recurrent thrombotic vessel occlusion after thrombolysis, isolated balloon angioplasty or stent implantation, leading to need for coronary artery bypass or even death, has been reported.6–10
Primary coronary angioplasty with stent implantation has become the treatment of choice for opening the infarct-related artery in patients with acute coronary syndrome. The association of angioplasty with thrombus aspiration improves myocardial reperfusion and clinical outcome. Since the risk of stent thrombosis in APS patients is unknown, in our patient we decided to perform thrombectomy only and to administer abciximab. To our knowledge, this is the first case in which repermeabilization of the artery was accomplished only with thrombectomy and glycoprotein IIb/IIIa platelet inhibitors without stent implantation.
The restenosis rate in APS patients is unknown. High lipoprotein levels and positive anticardiolipin antibodies increase the risk of restenosis in patients after balloon PCI.11 In our patient, the likelihood of restenosis was low, since no dilatation of the artery was performed. Due to the recurrence of ACS, it was decided to add aspirin to the acenocoumarol treatment, with a target INR of 2–3.12
In conclusion, APS should be considered in young patients with acute coronary syndrome, especially if there are no coronary risk factors. When the cause of the coronary occlusion is a thrombus without an associated significant stenotic lesion, thrombectomy and glycoprotein IIb/IIIa platelet inhibitors without stent implantation may be considered an effective alternative treatment.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.