The aim of this study was to analyze the quality of lipid-lowering therapy in a cohort of patients with cardiovascular disease enrolled in a Moscow-based registry, and to analyze the factors affecting the regularity of statin administration in this patient category.
MethodsThe present study included all patients who successively sought medical advice in the Preventive Pharmacotherapy Department of the Ministry of Healthcare of the Russian Federation between May 1 and December 31, 2011 (n=274). Each patient was given a specially designed questionnaire in order to assess compliance with the prescribed treatment that included the following questions: (1) if they knew, according to the results of previous exams, that they had elevated cholesterol levels (yes, no, don’t know); (2) what method of hypercholesterolemia correction they used (diet, medication, physical exercise, or other); (3) if they were taking any statins (regularly, no, irregularly); and (4) if yes, what statin preparation and what dose they were taking. Patients’ compliance with statin therapy was assessed on the basis of the responses received and the regularity of statin intake.
ResultsThe influence of various factors on regularity of statin intake in patients with cardiovascular disease was assessed by calculating odds ratios (OR) and 95% confidence intervals (CI) for advanced age (>70 years) (OR 0.49); higher statin dose than standard (OR 0.49); hypertension (OR 1.659); history of acute cerebrovascular event (OR 2.019); diabetes (OR 1.023); coronary heart disease (CHD) (OR 4.357); history of myocardial infarction (MI) (OR 4.838); history of coronary angiography/percutaneous coronary intervention (PCI) (OR 5.167).
ConclusionsAnalysis of factors with impact on regular compliance with statin therapy showed that the following were most significant: CHD, history of MI, and history of PCI. Previous cerebrovascular events and presence of diabetes did not motivate these patients to take statins on a regular basis.
O objetivo deste estudo foi analisar a qualidade do tratamento hipolipemiante realizado numa coorte de pacientes portadores de doenças cardiovasculares, obtido sob a forma de registo, em Moscovo, e analisar os fatores que afetam a regularidade da administração de estatinas nesta categoria de pacientes.
MétodosO presente estudo incluiu todos os pacientes que consecutivamente procuraram aconselhamento médico no Departamento de Farmacoterapia Preventiva durante o período de 1 de maio a 31 de dezembro 2011 (n=274). Cada paciente recebeu um questionário especialmente concebido para avaliar a adesão dos pacientes ao tratamento realizado, que incluiu as seguintes questões: 1) se tem conhecimento de níveis elevados de colesterol, de acordo com os exames realizados previamente (sim, não, desconhece); 2) que método utiliza para correção da hipercolesterolemia (dieta, medicação, exercício físico, outro); 3) se toma estatinas (toma regularmente, não toma, toma irregularmente); 4) se sim, qual a estatina e a dose. Com base nas resposta recebidas e regularidade da toma de estatinas, foi efetuada a avaliação do conceito de adesão à terapêutica com estes fármacos.
ResultadosPara determinar o significado de uma série de fatores de acordo com a sua influência sobre a regularidade da ingestão de estatinas em pacientes com doenças cardiovasculares, foram calculados odds ratio (OR): idade avançada (>70anos) - OR de 0,49; aumento da dose de estatina – OR de 0,49; hipertensão arterial (HA) - OR de 1,65; história prévia de doença cerebrovascular aguda (ACVD)- OR de 2,01; diabetes mellitus (DM)- OR de 1,02; doença arterial coronária (DAC)- OR de 4,35; história prévia de enfarte do miocárdio (IM) – OR de 4,83; antecedenetes de angiografia coronária (CAG)/intervenção coronária percutânea (ICP) OR de 5,16.
ConclusõesA análise dos fatores com maior impacto sobre a adesão à toma regular de estatinas mostrou serem mais significativos os seguintes: CHD, história prévia de MI e de PCI. Concomitantemente, salienta-se que a história prévia de ACVD e a presença de DM não motivaram estas classes de doentes a tomar estatinas de forma regular.
The value of statins to achieve target levels of total cholesterol, low-density lipoprotein (LDL) cholesterol, high-density lipoprotein (HDL) cholesterol, and triglycerides is emphasized in current international guidelines.1 The relationship between LDL level and frequency of cardiovascular events has been confirmed in large studies.2–7 However, clinicians do not always follow the recommendations.8 The situation with regard to the use of lipid-lowering drugs in Russia is particularly difficult. A study of statin use in Moscow obtained the following results: only 30% of patients with coronary heart disease (CHD) took statins; 80% of prescriptions were for simvastatin or lovastatin at initial doses; and mean duration of treatment was five months.9 However, this study investigated selective samples of patients. Data that are more relevant to clinical practice are obtained from studies conducted using the principles of consistent inclusion of patients, i.e. under registry rules.10 Analysis of the drugs taken as outpatients by high-risk patients before a reference myocardial infarction in the LIS study enrolled in the hospital's registry showed that the frequency of statin use was only 2%.11 With modern cardiovascular disease registries it is possible not only to determine the frequency of drug prescriptions but also to assess the factors that influence compliance with medication.
ObjectiveThe aim of this study was to analyze the quality of lipid-lowering therapy in a cohort of patients with cardiovascular disease enrolled in a Moscow-based registry, and to analyze the factors affecting the regularity of statin administration in this patient category.
MethodsThe PROFILE registry is a outpatient registry compiled by the Preventive Pharmacotherapy Department of the National Research Center for Preventive Medicine (NRCPM) of the Ministry of Healthcare of the Russian Federation. NRCPM is a federal medical center to which patients from other medical institutions (including municipal) are referred to seek medical advice. The PROFILE registry includes all patients presenting to the department for consultations on cardiovascular disease.
This study included all patients who sought medical advice in the Preventive Pharmacotherapy Department between May 1 and December 31, 2011. Each patient was given a specially designed questionnaire in order to assess compliance with the prescribed treatment. Patients were required to answer the following questions: (1) if they knew, according to the results of previous exams, that they had elevated cholesterol levels (yes, no, don’t know); (2) what method of hypercholesterolemia correction they used (diet, medication, physical exercise, or other); (3) if they were taking any statins (regularly, no, irregularly); and (4) if yes, what statin preparation and what dose they were taking. Compliance with statin therapy was assessed on the basis of the responses received and the regularity of statin intake. A registration card was completed for each patient observed during this period. The questionnaire and the registration card were developed by the researchers. The questionnaire was filled in directly by the patient, while the registration card (including anthropometric, clinical, laboratory and test data, and previous history) was filled in by a physician.
Patients were divided into three age groups: <50 years old, 50–70 years old, and >70 years old. In addition, the following factors were taken into account: (a) alcohol consumption (according to the questionnaire data) – none, occasional (once or twice a week or less), regularly (three or more times a week); (b) smoking status: current smoker, non-smoker, former smoker; (c) education: higher education or not; (d) statin dose: low (rosuvastatin <10 mg, atorvastatin <20 mg, simvastatin <20 mg), medium/standard (rosuvastatin 10–20 mg, atorvastatin 20–40 mg, simvastatin 20–40 mg), high (rosuvastatin >20 mg; atorvastatin >40 mg; simvastatin >40 mg). On the basis of these data patients’ compliance with treatment and its effectiveness as shown by the results of further analysis were assessed.
All patients gave their written informed consent for participation in the study and the questionnaire was approved by the Independent Ethics Committee of NRCPM. Blood tests for cholesterol and its fractions were performed in the laboratory of NRCPM on the day of each patient's enrollment.
Statistical analysisThe statistical data processing was performed using the Statistica 6.0 software package (StatSoft). Data on the three groups are presented as median and interquartile range or as number and percentage of the total. The chi-square test was used to compare groups for qualitative variables. Rank analysis of variance using the Kruskal-Wallis test was used for multiple comparisons of quantitative variables between groups (three or more). Calculation of odds ratios (OR) and 95% confidence intervals (CI) was carried out to determine the influence of various factors on regularity of statin intake in patients with cardiovascular disease. OR were calculated on the basis of 2×2 contingency tables, in cells which accounted for the number of patients regularly and irregularly taking statins depending on the basic attributes analyzed. Differences were considered statistically significant when p<0.05.
ResultsThe present study included consecutive patients seen in the Preventive Pharmacotherapy Department between May 1 and December 31, 2011. During this period 274 patients were recorded in the registry. Their main demographic and clinical characteristics are presented in Table 1.
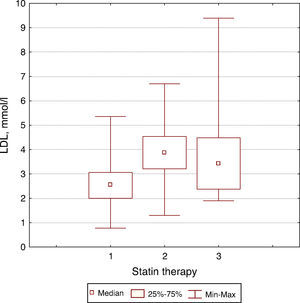
Main demographic and clinical characteristics of the study population.
| Age, years (range) | 64.0 (57.0–72.0) |
| Male gender | 135 (49.3%) |
| Higher education | 231 (84.3%) |
| Currently employed | 141 (51.4%) |
| BMI | 28.7 (25.4–31.3) |
| Smoking | 40 (14.6%) |
| Baseline HC >5.0 mmol/l | 266 (97.0%) |
| Current HC >5.0 mmol/l | 113 (41.2%) |
| Current HC >4.5 mmol/l | 153 (55.8%) |
| Diabetes | 43 (15.7%) |
| Hypertension | 230 (83.9%) |
| CHD | 85 (31.0%) |
| Angina CCS grade I-IV | 66 (24.1%) |
| History of MI | 47 (17.1%) |
| Interventional procedures | |
| CAG | 50 (18.2%) |
| PCI | 22 (8.0%) |
| CABG | 9 (3.3%) |
| History of stroke | 19 (6.9%) |
| Heart failure | 50 (18.2%) |
BMI: body mass index; CABG: coronary artery bypass grafting; CAG: coronary angiography; CHD: coronary heart disease; HC: hypercholesterolemia; MI: myocardial infarction; PCI: percutaneous coronary intervention.
Patients were divided into three groups according to how regularly they were taking statins: regularly, irregularly, or none. These groups were compared in terms of lipid profile (Table 2).
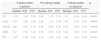
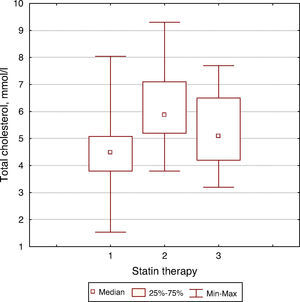
Comparisons between groups according to lipid profile.
| Taking statins regularly | Not taking statins | Taking statins irregularly | p | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Median | P25 | P75 | Median | P25 | P75 | Median | P25 | P75 | ||
| TC | 4.50 | 3.80 | 5.08 | 5.88 | 5.20 | 7.10 | 5.10 | 4.20 | 6.50 | 0.0001 |
| LDL | 2.57 | 2.00 | 3.06 | 3.89 | 3.21 | 4.54 | 3.43 | 2.38 | 4.48 | 0.0001 |
| VLDL | 0.62 | 0.53 | 0.76 | 0.62 | 0.53 | 0.76 | 0.55 | 0.44 | 0.79 | 0.6456 |
| HDL | 1.17 | 0.95 | 1.43 | 1.19 | 0.95 | 1.43 | 1.22 | 1.08 | 1.41 | 0.8905 |
| TG | 1.28 | 1.08 | 1.65 | 1.33 | 1.08 | 1.65 | 1.20 | 0.97 | 2.58 | 0.5421 |
HDL: high-density lipoprotein cholesterol; LDL: low-density lipoprotein cholesterol; P25: 25th percentile; P75: 75th percentile; TC: total cholesterol; TG: triglycerides; VLDL: very low density lipoprotein cholesterol.
There were significant differences in total cholesterol and LDL cholesterol levels between patients regularly taking statins and patients not taking or irregularly taking statins (Figures 1 and 2).
Odds ratios (OR) and their 95% confidence intervals (CI) were calculated to determine the influence of various factors on regularity of statin intake (Table 3).
Influence of major factors on regularity of statin intake.
| OR | 95% CI | p | |
|---|---|---|---|
| Sociodemographic variables | |||
| Elderly age (>70 years) | 0.429 | 0.224–0.822 | 0.015 |
| Higher statin dose than standard | 0.49 | 0.169–1.423 | 0.306 |
| Smoking | 0.607 | 0.812–1.404 | 0.342 |
| Education | 0.855 | 0.384–1.906 | 0.86 |
| Avoidance of alcohol | 1.145 | 0.640–2.049 | 0.757 |
| Male gender | 1.775 | 0.993–3.173 | 0.072 |
| Currently employed | 1.966 | 0.694–4.322 | 0.129 |
| Clinical variables | |||
| Diabetes | 1.023 | 0.489–2.138 | 0.898 |
| Hypertension | 1.659 | 0.692–3.979 | 0.365 |
| History of stroke | 2.019 | 0.631–6.463 | 0.347 |
| CHD | 4.357 | 2.188–8.677 | 0.0001 |
| History of MI | 4.838 | 1.765–13.259 | 0.002 |
| History of CAG/PCI | 5.167 | 2.055–12.99 | 0.0001 |
CAG: coronary angiography; CHD: coronary heart disease; CI: confidence interval; PCI: percutaneous coronary intervention.
The question of patients’ compliance with prescribed therapy is extremely important, especially concerning statins, given their possible side effects that require dynamic control by biochemical blood tests.
This study addresses these issues. Certain limitations should be noted, particularly the selectivity of the study population; this was not an epidemiological study, but an analysis of clinical practice that assessed ordinary patients.
The criteria for statin use in this study were based on current guidelines: patients with TC >5 mmol/l and LDL >3 mmol/l and high-risk patients with documented CHD, previous MI or stroke or associated clinical conditions, as well as with additional risk factors including TC >4.5 mmol/l and LDL >2.5 mmol/l.
The study is relevant to the issue, which has also been analyzed in other studies carried out in recent years.12–16 It is striking that our study, which was small but governed strictly by guidelines for registries, revealed such interesting data. In our analysis of the factors affecting regularity of statin intake in patients with cardiovascular disease enrolled in the PROFILE registry, those that were most likely to increase the chances that the patient would take statins regularly were the presence of CHD and a history of MI and PCI (Table 3). At the same time it should be noted that a history of stroke and the presence of diabetes did not motivate these patients to take statins on a regular basis.
This can probably be explained by the fact that cardiologists are more likely to adhere to current international guidelines for the management of their patients and to prescribe statins, in contrast to neurologists and endocrinologists, who also often see patients with a history of stroke and diabetes, respectively.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.