A 61-year-old man was admitted to our hospital due to acute inferior myocardial infarction, complicated by complete heart block and cardiogenic shock. The patient had received dual antiplatelet therapy (aspirin and ticagrelor) and an emergency coronary angiogram was performed. It should be noted that he had previously been with hypertension, hypercholesterolemia, a 48×41-mm abdominal aortic aneurysm and gastric ulcer.
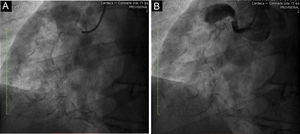
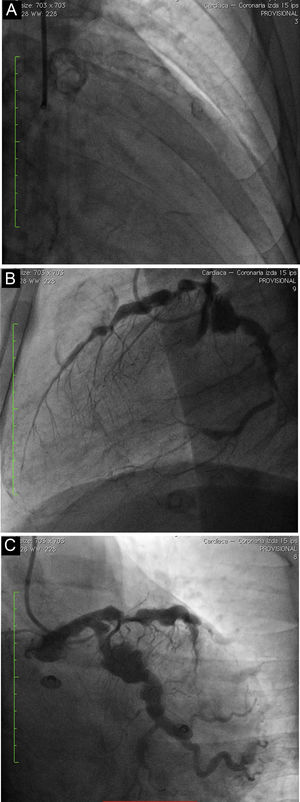
Single-plane fluoroscopy (Figure 1A) and coronary angiography showed a giant calcified aneurysm (73 mm×72 mm) of the mid-right coronary artery (RCA), and smaller aneurysms that were proximal and distal to the first. The proximal RCA was occluded by a thrombus (Figure 1B) so percutaneous revascularization could not be performed. The left coronary artery had multiple calcified aneurysms, and severe stenosis of the proximal anterior descending coronary artery (Figures 2A–C) was found. We performed ascending aortography, which was normal. These findings could be related to Kawasaki disease (KD). Despite good evolution following cardiogenic shock, the patient had upper gastrointestinal bleeding, a major and acute complication, which was fatal.
KD is a self-limiting acute systemic vasculitis of unknown etiology, which affects infants and children. It usually involves small and medium-sized arteries, and commonly the coronary arteries. The morbidity and mortality in KD are associated with the development of coronary aneurysms that can lead to myocardial infarction. In adults, most cases are reported in patients under the age of 40 years. This case is of great interest due to the late onset and the severe form of the disease.
Conflicts of interestThe authors have no conflicts of interest to declare.