We wondered if a modification of the conventional transseptal puncture technique performed with an angioplasty wire could be useful in patients with contrast hypersensitivity or allergy-like reactions.
MethodsThis study comprised our initial experience in 22 patients with atrial fibrillation who were scheduled for an electrophysiology study (EPS) and pulmonary vein ablation and who had a contraindication for iodinated contrast administration.
ResultsOf the 22 patients, 16 were men and ages ranged from 27 to 74 years (mean 56 years). Overall successful transseptal access was achieved in all 22. A control echocardiogram was performed in all patients. There were no complications in any case and no significant differences were found from the conventional transseptal puncture technique regarding procedure or fluoroscopy time.
ConclusionsA modification of the conventional transseptal puncture technique performed with fluoroscopy and EPS catheters for anatomical reference and an angioplasty wire is an option in cases with severe contrast hypersensitivity.
Questionámo-nos se uma modificação da técnica de punção transseptal tradicional realizada com fio guia de angioplastia poderia ser útil em doentes com hipersensibilidade ou outros tipos de reações alérgicas ao contraste.
MétodosEste estudo reflete a nossa experiência inicial com 22 doentes com fibrilhação auricular, programados para estudo eletrofisiológico e ablação da veia pulmonar, que tiveram contraindicação para injeção de contraste com iodo.
ResultadosO acesso transseptal global bem-sucedido foi alcançado na totalidade dos 22 doentes (16 homens) entre os 27-74 anos (idade média 56). Foi realizado um ecocardiograma de controlo em todos os doentes. Não se registaram complicações nem diferenças significativas em relação à técnica de punção tradicional relativamente à duração do procedimento ou ao tempo de fluoroscopia.
ConclusõesA modificação da técnica de punção transseptal tradicional com fluoroscopia, cateteres de EEF para referências anatómicas e fio guia de angioplastia pode constituir uma opção válida nos casos de hipersensibilidade grave ao contraste.
Transseptal puncture was first performed in 1959 by Ross, Braunwald and Morrow,1 and later Brockenbrough et al.2 published their initial experience with 450 patients. Transseptal puncture appears to be safe in experienced hands, but although rare, fatal complications do occur and it may be associated with life-threatening situations, with an incidence of 0.74-0.79% described in other publications.3 In centers where puncture cannot be guided by echocardiography, fluoroscopy with administration of contrast dye is frequently performed.4 However, due to the significant increase in the number of procedures requiring transseptal puncture, such as atrial fibrillation (AF) ablation, contrast hypersensitivity and allergy-like reactions are nowadays frequently encountered.5 The aim of this study was to demonstrate the added value of routine use of an angioplasty wire as described by Daoud and Ahsan et al.,6,7 thus potentially preventing complications during fluoroscopy, in cases with severe contrast hypersensitivity.
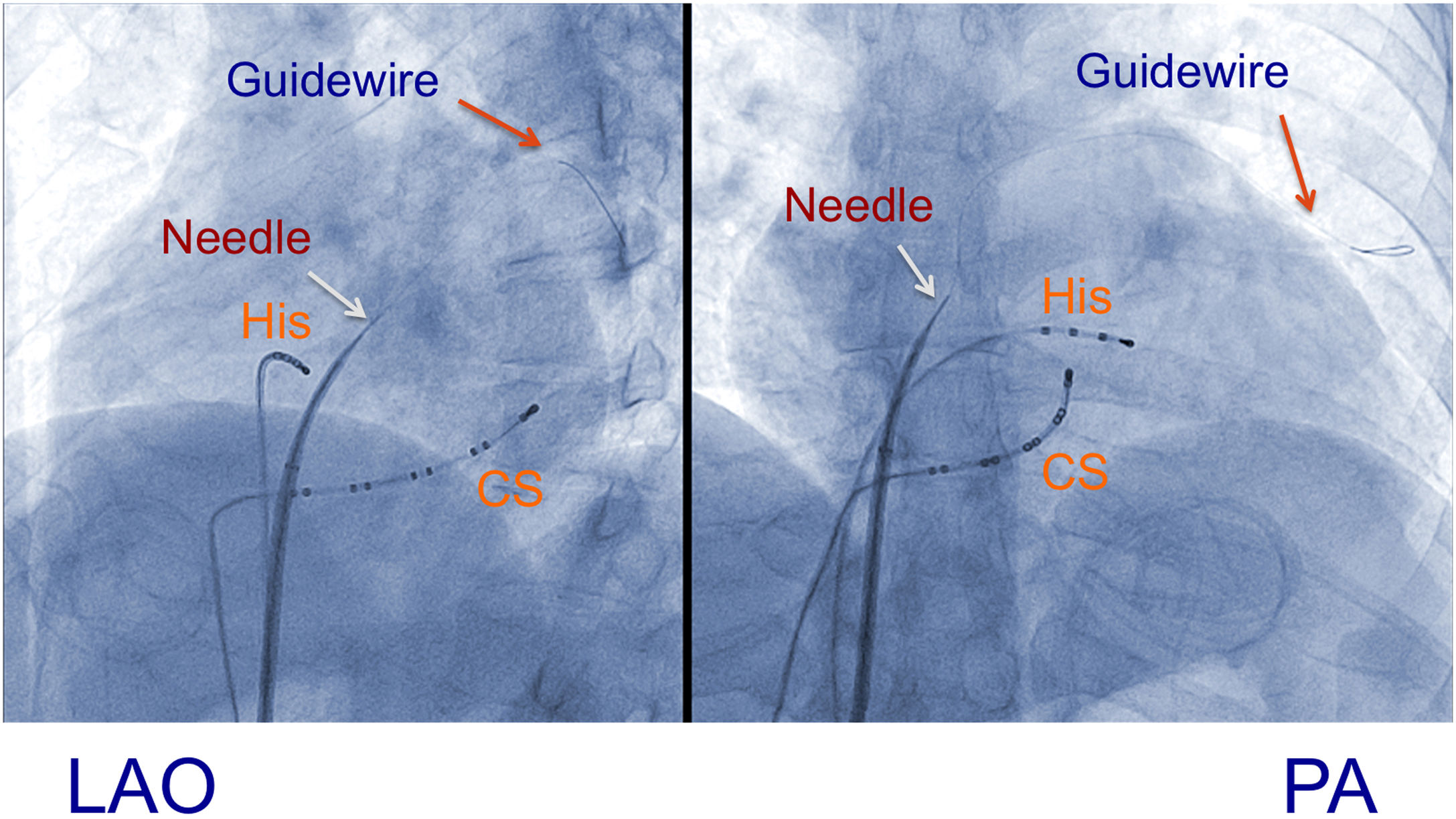
MethodsThis study comprised our initial experience in 22 patients with AF and referred for electrophysiology study (EPS) and pulmonary vein ablation and who had a contraindication for iodinated contrast administration, including eight cases with contrast hypersensitivity. All procedures were performed under conscious sedation and local anesthesia. In all patients, four introducers were displayed in the femoral veins (two on each side: 6F and 7F left, 7F and 8F right). An 8F SL0 transseptal sheath and dilator (St. Jude Medical, Minnetonka, MN, USA) replaced the right 7F introducer and was advanced over a 0.035-inch wire into the superior vena cava. Following standard transseptal procedures, no pressure recording was used. The wire was removed and a standard Brockenbrough needle (BRK XS, St. Jude Medical) was introduced through the sheath. Under fluoroscopic guidance, the transseptal sheath and needle, in a 4-6 o’clock position, were gradually withdrawn to engage and puncture the fossa ovalis. A 0.36 mm×180 cm Runthrough NS floppy PTCA guidewire (Terumo) was then introduced through the Brockenbrough needle instead of contrast administration, and advanced to one pulmonary vein to confirm appropriate location (Figure 1A and B, Video 1 and 2). Finally, the needle, dilator, and sheath were advanced over the guidewire only if the distal part of the guidewire was clearly in a pulmonary vein, outside the cardiac silhouette. Once this was confirmed, both needle and guidewire were removed together to prevent accidental wire embolization. Following our standard procedure, only a single transseptal puncture was performed in all patients. Subsequently, the ablation catheter was advanced into the left atrium. EPS was performed in the standard way and a control echocardiogram was performed in all patients. Data were analyzed using SPSS for Windows (version 15.0, SPSS Inc., Chicago, IL, USA). Continuous variables are expressed as mean ± SD.
Left anterior oblique (LAO) and posteroanterior (PA) views in which catheters are displayed as anatomical references, with a decapolar catheter in the coronary sinus (CS) and a quadripolar catheter in the bundle of His (His); an 8F SL0 transseptal sheath and dilator (St. Jude Medical) and standard Brockenbrough needle (BRK XS, St. Jude Medical) with deployment of a Runthrough floppy guidewire through the Brockenbrough needle.
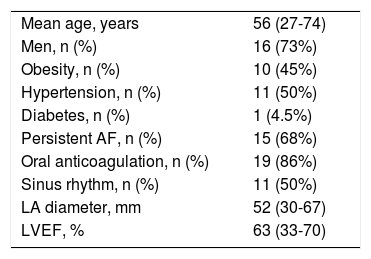
Of the 22 patients, 16 were men and ages ranged from 27 to 74 years (mean 56 years). Overall successful transseptal access was achieved in all 22 patients. The clinical and echocardiographic characteristics of the study population are described in Table 1. Seven patients had paroxysmal AF and fifteen persistent AF, and most were under oral anticoagulation before the procedure (19 patients, 86%). Mean fluoroscopy time was 153±69 s (range 56-600 s). There were no complications in any case. Hence, although based on a limited number of cases, in our experience it appears that the modification of conventional transseptal puncture technique performed with an angioplasty wire is feasible, and could be of particular interest in cases with severe contrast hypersensitivity or a contraindication to iodinated contrast administration.
Clinical and echocardiographic characteristics of the study population (n=22).
| Mean age, years | 56 (27-74) |
| Men, n (%) | 16 (73%) |
| Obesity, n (%) | 10 (45%) |
| Hypertension, n (%) | 11 (50%) |
| Diabetes, n (%) | 1 (4.5%) |
| Persistent AF, n (%) | 15 (68%) |
| Oral anticoagulation, n (%) | 19 (86%) |
| Sinus rhythm, n (%) | 11 (50%) |
| LA diameter, mm | 52 (30-67) |
| LVEF, % | 63 (33-70) |
AF: atrial fibrillation, LA: left atrial, LVEF: left ventricular ejection fraction.
Studies show that echocardiographic imaging may be better than fluoroscopy for guiding transseptal puncture,8 especially in less experienced hands, increasing safety through early detection of complications. Nevertheless, transesophageal echocardiography requires a high level of sedation and is sometimes poorly tolerated, while intracardiac echocardiography requires additional expertise, significantly increases the cost of the procedure,9 and is not available in most centers. As is well known, iodinated contrast administration should be avoided, whenever possible, in any patient who has had a previous moderate or severe anaphylactoid reaction to iodinated contrast material, although steroid premedication is occasionally recommended. So from our point of view, this subtle variant of the conventional transseptal puncture technique using a guidewire helps ensure successful atrial septal crossing by advancing the transseptal assembly over the guidewire.10,11 It could be especially useful in patients for whom cardiac imaging is not available and those with severe intolerance to iodinated contrast, difficult septal anatomy or renal insufficiency. Importantly, a substantial number of patients require a second left atrial procedure after AF ablation; repeat transseptal catheterization after a first AF ablation may be more challenging and potentially associated with more complications than the first procedure.12
Furthermore, transseptal puncture is nowadays not used exclusively in AF ablation, but also in ablation of left-sided accessory pathways and left ventricular tachycardia, and in other interventional cardiology procedures. Even though our study is not a randomized comparison of conventional fluoroscopy-guided and wire-guided transseptal puncture, it demonstrates the added value of the latter approach in patients with contrast allergies, which to our knowledge has never been studied before. This variation of the technique could be reasonable in centers that rely heavily on contrast and fluoroscopy.
ConclusionsA slight modification of the conventional transseptal puncture technique performed with fluoroscopy and EPS catheters for anatomical reference and an angioplasty wire instead of iodinated contrast administration is an option in cases with severe contrast hypersensitivity.
Conflicts of interestThe authors have no conflicts of interest to declare.
The following are the supplementary material to this article:
Left anterior oblique view in which catheters are displayed as anatomical references, with a decapolar catheter in the coronary sinus and a quadripolar catheter in the bundle of His; an 8F SL0 transseptal sheath and dilator (St. Jude Medical) and standard Brockenbrough needle (BRK XS, St. Jude Medical) with deployment of a Runthrough floppy guidewire through the Brockenbrough needle.
Posteroanterior view in which catheters are displayed as anatomical references, with a decapolar catheter in the coronary sinus (CS) and a quadripolar catheter in the bundle of His (His); an 8F SL0 transseptal sheath and dilator (St. Jude Medical) and standard Brockenbrough needle (BRK XS, St. Jude Medical) with deployment of a Runthrough floppy guidewire through the Brockenbrough needle.