The coronavirus SARS-CoV-2 (COVID-19) pandemic has been an unmatched challenge to global healthcare. Although the majority of patients admitted with acute coronary syndrome (ACS) may not be infected with COVID-19, the quarantine and public health emergency measures may have affected this particular high risk group. The objective of this study is to assess the impact of the early period of the COVID-19 pandemic on ACS admissions and clinical course in a tertiary care hospital in Portugal's most affected region.
MethodsThis retrospective, case-control study included patients admitted with a diagnosis of ACS during March and April 2020 (pandemic group) and in the same period in 2019 (control group). Clinical course and complications were also assessed.
ResultsDuring the pandemic, there were fewer ACS admissions but presentation was more severe, with a larger proportion of acute ST-elevation myocardial infarctions (54.9% vs. 38.8%, p=0.047), higher maximum troponin levels and greater prevalence of left ventricular systolic dysfunction at discharge (58.0% vs. 35.0%, p=0.01). In this population, although not statistically significant, it was observed a delay between the onset of symptoms and percutaneous coronary intervention, which may traduce a deferred search for urgent medical care during the pandemic.
ConclusionThe lockdown phase of COVID-19 pandemic was associated with fewer and more severe ACS in a Tertiary Care Hospital in Portugal's most affected region by the pandemic.
A pandemia pela COVID-19 colocou os sistemas de saúde em todo o mundo sob uma exigência sem precedentes. Apesar de a maioria dos doentes admitidos por síndrome coronária aguda não estar infetada com COVID-19, as medidas de saúde pública instituídas poderão afetar este grupo de risco particularmente elevado. O objetivo deste estudo passa por avaliar o impacto que a fase inicial da pandemia COVID-19 teve na apresentação e evolução clínica de doentes admitidos por síndrome coronária aguda num hospital terciário numa das regiões de Portugal mais afetadas pela pandemia.
MétodosEste estudo retrospetivo de caso-controlo incluiu doentes admitidos com o diagnóstico de síndrome coronária aguda entre março e abril de 2020 (grupo pandémico) e no mesmo período em 2019 (grupo controlo). Foram recolhidos dados em relação à evolução clínica em regime de internamento e após a alta.
ResultadosDurante o período de pandemia, verificou-se uma diminuição do número de admissões por síndrome coronária aguda bem como apresentações mais graves, registando-se uma maior proporção de enfartes agudos do miocárdio com supradesnivelamento do segmento ST (54,9% versus 38,8%, p=0,047), níveis máximos de troponina I mais elevados, e maior prevalência de disfunção sistólica do ventrículo esquerdo à data de alta (58,0% versus 35,0%, p=0,01). Apesar de não se ter atingido valores estatisticamente significativos, observou-se um aumento do intervalo de tempo entre o início de sintomas e a realização de intervenção coronária percutânea, o que poderá traduzir um atraso na procura de cuidados de saúde.
ConclusãoA fase inicial da pandemia COVID-19 associou-se a um menor número e uma maior gravidade de admissões por síndrome coronária aguda num hospital terciário numa das regiões de Portugal mais afetadas pela pandemia.
COVID-19, caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is a highly contagious condition that may lead to serious respiratory illness and premature death; with up to 20% of hospitalized patients requiring mechanical ventilation and intensive care.1,2 The first cases were reported in December 2019 in Wuhan, Hubei, China but rapidly spread worldwide, being declared as a pandemic by the WHO on 11 March 2020.3 Currently, there are about 34 million cases, with more than 1 million deaths globally.4
In order to contain the COVID-19 pandemic, there was a widespread lockdown worldwide, with restrictive home confinement and social distancing measures.5,6 Overwhelmed healthcare systems were also promptly restructured, expanding intensive care units and altering or cancelling non-essential procedures.7,8
In the meantime, many countries reported a significant reduction in hospital admissions for several acute conditions that require life-saving evidence-based emergent treatment, such as acute coronary syndrome (ACS) and stroke.9–20 Moreover, patients with cardiovascular disease are at increased risk of severe COVID-19 illness, endorsing the direct and indirect consequences of delayed care of this particular group of patients.21–23 In Portugal, the first case was reported on 2 March 2020 in Porto. The mandatory national lockdown was imposed from 18 March to 2 May, amounting to 25 190 cases and 1023 deaths due to COVID-19 at the end of this period. The northern region of Portugal, mainly Porto's metropolitan area, had the highest incidence of COVID-19 cases, reaching around 14 951 cases and 585 deaths.24–27
The aim of this study was to assess the impact of the COVID-19 pandemic on ACS admissions to the Cardiology Department of the Centro Hospitalar Universitário de São João, a tertiary care hospital in Porto's metropolitan area.
MethodsThis retrospective, case-controlled study included all patients admitted to the Cardiology Department of Centro Hospitalar Universitário de São João with a diagnosis of ACS, during the months of March and April of 2020 (pandemic group) and in the same period of 2019 (control group). Patients who tested positive for SARS-CoV-2, and therefore admitted to COVID-19 exclusive units, were also included.
The database used in this study was completed retrospectively using the available clinical records. Patients were selected based on the final diagnosis at the time of discharge (ST-segment elevation myocardial Infarction (STEMI), non-ST-segment elevation myocardial infarction (NSTEMI) or unstable angina (UA)). ACS was defined according to the Fourth Universal Definition of Myocardial Infarction.28
Demographic characteristics (gender, age, presence of cardiovascular risk factors, chronic kidney disease, previous vascular events and LV dysfunction), in-hospital clinical course (length of stay, Killip class, maximum troponin value, complications, prevalence of left ventricular (LV) systolic dysfunction at discharge), and short term mortality were compared between groups. Continuous variables were summarized as mean ± standard deviation or median (25, 75 percentiles) and categorical variables as proportions. Groups were compared using Student's t tests, Wilcoxon Rank Sum tests, and χ2 tests, as appropriate. Values of p<0.05 were considered significant. All statistical analyses were performed using IBM SPSS statistics 25 (New York, United States).
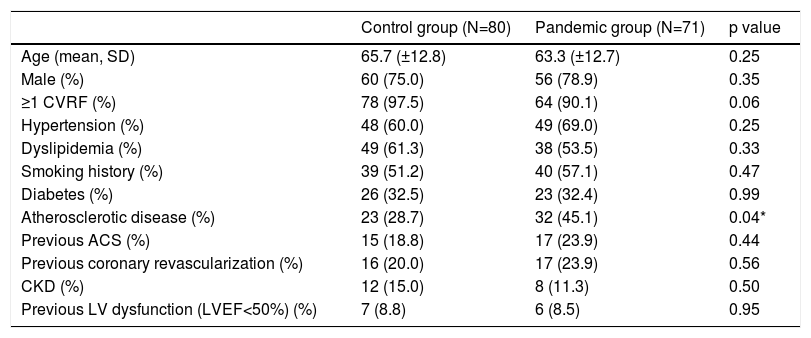
ResultsBaseline patient characteristicsOur study included 151 patients hospitalized with ACS in the two aforementioned periods. There were 71 ACS admissions between March and April, 2020 (n=71), representing a reduction of 11.3% relative to the same period in 2019 (n=80).
Overall, there were no significant differences in age, gender, and cardiovascular risk factors in both groups (Table 1). The pandemic group had a higher prevalence of atherosclerotic disease (defined as history of peripheral, coronary or cerebral arterial disease) (45.1% vs. 28.7%, p=0.04), although there was no difference considering previous ACS or revascularization procedures.
Baseline characteristics of the participants.
| Control group (N=80) | Pandemic group (N=71) | p value | |
|---|---|---|---|
| Age (mean, SD) | 65.7 (±12.8) | 63.3 (±12.7) | 0.25 |
| Male (%) | 60 (75.0) | 56 (78.9) | 0.35 |
| ≥1 CVRF (%) | 78 (97.5) | 64 (90.1) | 0.06 |
| Hypertension (%) | 48 (60.0) | 49 (69.0) | 0.25 |
| Dyslipidemia (%) | 49 (61.3) | 38 (53.5) | 0.33 |
| Smoking history (%) | 39 (51.2) | 40 (57.1) | 0.47 |
| Diabetes (%) | 26 (32.5) | 23 (32.4) | 0.99 |
| Atherosclerotic disease (%) | 23 (28.7) | 32 (45.1) | 0.04* |
| Previous ACS (%) | 15 (18.8) | 17 (23.9) | 0.44 |
| Previous coronary revascularization (%) | 16 (20.0) | 17 (23.9) | 0.56 |
| CKD (%) | 12 (15.0) | 8 (11.3) | 0.50 |
| Previous LV dysfunction (LVEF<50%) (%) | 7 (8.8) | 6 (8.5) | 0.95 |
ACS: acute coronary syndrome; CVRF: cardiovascular risk factors; CKD: chronic kidney disease; LV: left ventricular; LVEF: left ventricular ejection fraction; SD: standard deviation. *p<0.05.
Three patients from the pandemic group tested positive for SARS-COV-2.
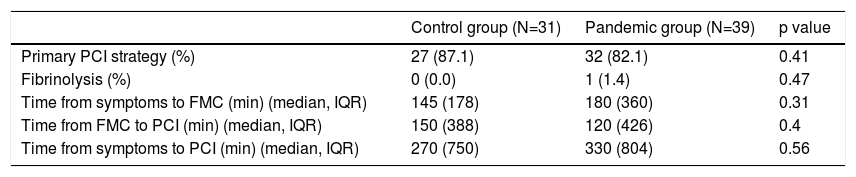
Initial presentation and managementThe proportion of ACS presenting as STEMI was significantly higher in the pandemic group (54.9% vs. 38.8%, p=0.047). This was driven not only by a decrease in the number of NSTEMI and UA patients (49 vs. 32) but also by an increase in the absolute number of STEMIs (31 vs. 39).
Among STEMI admissions, although not statistically significant, there was a longer period between time of first symptom onset to first medical contact (FMC), during the pandemic (control vs. pandemic; median 145±178 min vs. 180±360 min, p=0.31) (Table 2). This was more pronounced considering NSTEMI and UA presentations (control vs. pandemic; median 180±330 min vs. 300±1170 min, p=0.38).
Initial presentation and management of ST-elevation myocardial infarction patients.
| Control group (N=31) | Pandemic group (N=39) | p value | |
|---|---|---|---|
| Primary PCI strategy (%) | 27 (87.1) | 32 (82.1) | 0.41 |
| Fibrinolysis (%) | 0 (0.0) | 1 (1.4) | 0.47 |
| Time from symptoms to FMC (min) (median, IQR) | 145 (178) | 180 (360) | 0.31 |
| Time from FMC to PCI (min) (median, IQR) | 150 (388) | 120 (426) | 0.4 |
| Time from symptoms to PCI (min) (median, IQR) | 270 (750) | 330 (804) | 0.56 |
FMC: first medical contact; IQR: interquartile range; PCI: percutaneous coronary intervention.
The proportion of STEMI patients who underwent emergent angiography was similar in both years (87.1% vs. 82.1%, p=0.41). Time from FMC to emergent percutaneous coronary intervention (PCI) was also similar (150+/-270 min vs. 120+/-492 min, p=0.56). Among patients admitted to hospitals without the ability to perform primary PCI, there was no significant difference in TMC to PCI times in both groups (190+/-632 vs. 210+/-600, p=0.57).
One of the patients from the pandemic group had known SARS-COV-2 infection at the time of presentation. He was admitted with inferior wall STEMI (less than one hour after symptom onset) and underwent fibrinolysis, followed by routine PCI. The decision to perform fibrinolysis was made based on a STEMI reperfusion algorithm published at the time.30
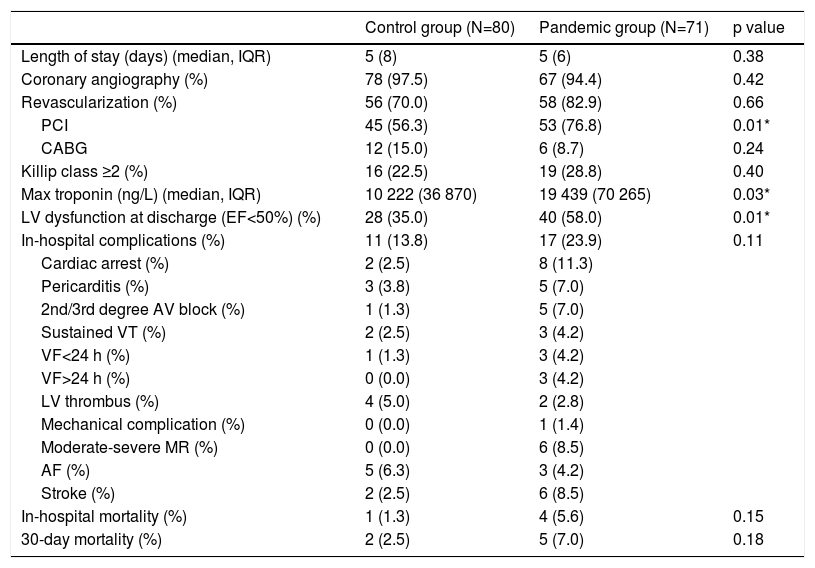
Clinical courseBoth groups had a similar length of hospitalization (control vs. pandemic: 5±8 vs. 5±6 days, p=0.377) (Table 3). There was no difference regarding Killip class classification. Maximum measured high-sensitivity Troponin I was significantly higher in the pandemic group (19 439±70 265 ng/L vs. 10 222±36 870 ng/L, p=0.03). There were also significantly more patients with LV systolic dysfunction at discharge (58.0% vs. 35.0%, p=0.01).
Clinical course and outcomes.
| Control group (N=80) | Pandemic group (N=71) | p value | |
|---|---|---|---|
| Length of stay (days) (median, IQR) | 5 (8) | 5 (6) | 0.38 |
| Coronary angiography (%) | 78 (97.5) | 67 (94.4) | 0.42 |
| Revascularization (%) | 56 (70.0) | 58 (82.9) | 0.66 |
| PCI | 45 (56.3) | 53 (76.8) | 0.01* |
| CABG | 12 (15.0) | 6 (8.7) | 0.24 |
| Killip class ≥2 (%) | 16 (22.5) | 19 (28.8) | 0.40 |
| Max troponin (ng/L) (median, IQR) | 10 222 (36 870) | 19 439 (70 265) | 0.03* |
| LV dysfunction at discharge (EF<50%) (%) | 28 (35.0) | 40 (58.0) | 0.01* |
| In-hospital complications (%) | 11 (13.8) | 17 (23.9) | 0.11 |
| Cardiac arrest (%) | 2 (2.5) | 8 (11.3) | |
| Pericarditis (%) | 3 (3.8) | 5 (7.0) | |
| 2nd/3rd degree AV block (%) | 1 (1.3) | 5 (7.0) | |
| Sustained VT (%) | 2 (2.5) | 3 (4.2) | |
| VF<24 h (%) | 1 (1.3) | 3 (4.2) | |
| VF>24 h (%) | 0 (0.0) | 3 (4.2) | |
| LV thrombus (%) | 4 (5.0) | 2 (2.8) | |
| Mechanical complication (%) | 0 (0.0) | 1 (1.4) | |
| Moderate-severe MR (%) | 0 (0.0) | 6 (8.5) | |
| AF (%) | 5 (6.3) | 3 (4.2) | |
| Stroke (%) | 2 (2.5) | 6 (8.5) | |
| In-hospital mortality (%) | 1 (1.3) | 4 (5.6) | 0.15 |
| 30-day mortality (%) | 2 (2.5) | 5 (7.0) | 0.18 |
AF: atrial fibrillation; AV: atrioventricular; CABG: coronary artery bypass graft; EF: ejection fraction; IQR: interquartile range; LV: left ventricular; MR: mitral regurgitation; PCI: percutaneous coronary intervention; VF: ventricular fibrillation; VT: ventricular tachycardia. *p<0.05.
Finally, there was a greater proportion of patients in the pandemic group with in-hospital complications (23.9% vs. 13.8%, p=0.11) and in-hospital (5.6% vs. 1.3%, p=0.15) and 30-day (7.0% vs. 2.5%, p=0.18) mortality, although these did not reach statistical significance (Table 3). At the time of discharge, there was no difference in the number of patients receiving angiotensin-converting-enzyme inhibitors and/or beta-blockers (control vs. pandemic; 96.8% vs. 94.6%, p=0.55). Almost all patients had undergone angiography (97.5% vs. 94.4%, p=0.42). Globally, there was a trend towards higher revascularization rates in the pandemic group (70.0% vs. 82.9%, p=0.66), with a significantly higher number of patients undergoing PCI (56.3% vs. 76.8%, p=0.01) and fewer patients undergoing coronary artery bypass grafting (15.0% vs. 8.7%, p=0.24).
DiscussionIn the early COVID-19 pandemic, the number of patients requiring hospitalization and intensive care overwhelmed the healthcare facilities in numerous countries. Meanwhile, a major decline in hospital admissions with ACS in several medical centers was observed, possibly due to the quarantine and other large-scale public health measures.9–17 Some centers in highly affected regions, like Northern Italy and China, implemented early fibrinolysis protocols in STEMI treatment, with a direct decrease in the number of primary PCIs.32,33 Afterwards, position statements reinforced that during the COVID-19 pandemic, the standard of care for STEMI patients at PCI-capable hospitals remained primary PCI when it could be provided in a timely manner.29–34 During the first phase of the COVID-19 pandemic in Portugal, the population of Porto and the surrounding urban area was the most affected by SARS-COV-2 disease. Contrary to what was seen in other countries, we did not see a clear reduction in hospitalization but presentations were more severe, with a larger proportion of STEMIs, higher maximum troponin values and greater prevalence of LV systolic dysfunction at discharge. The fear of becoming infected by SARS-Cov-2 may have discouraged patients that experienced milder symptoms to seek urgent medical care. In fact, previous studies in other countries noted a deferred search for urgent medical care during the pandemic.17,29 Although not statistically significant, our data suggests that there was a delay between the onset of symptoms and search for medical care during the pandemic. The non-significance of this finding may be related to the small sample size. This delay may explain the larger number of STEMIs admitted and consequently the higher prevalence of LV systolic dysfunction at the time of discharge. It is of relevance that during the pandemic there was a significantly higher prevalence of atherosclerosis among patients and this may have had some impact on the differences seen in the outcomes of the two groups.
In-hospital and 30-day mortality were numerically higher in patients admitted during the pandemic, similar to those observed in other studies.15 Our study was innovative since it also assessed complications related to ACS; the rate was overall low but a higher proportion of complications occurred during the pandemic. This may translate into higher mortality and higher morbidity in the near future. Our concern also extends to patients that did not reach out for medical care during the pandemic, which may negatively affect long-term cardiovascular health. This may partially explain the higher revascularization rates, since milder cases may not have come to medical attention. More studies should be designed to explore these events.
Importantly, there was no evidence of significant delay in the healthcare response to STEMI patients, including in cases initially admitted to hospitals without the ability to perform primary PCI. Revascularization rates were not precluded and fibrinolysis use was residual. These data may be explained since Portugal did not reach a situation in which the health care system was overwhelmed or began to collapse.34
This analysis has some limitations. Only patients admitted to one center were included. Additionally, acute morbidity and mortality may be underestimated, since patients who died in the pre-hospital phase/emergency room or were admitted at other intensive care units were not included.
ConclusionDuring the lockdown phase of the COVID-19 pandemic, there were fewer admissions for ACS but more serious presentations in a tertiary hospital center in the region most affected by COVID-19 in Portugal, possibly due to a deferred search for healthcare by the population. As ACS requires prompt in-hospital assessment and treatment in order to prevent significant morbidity and mortality, the general population should be made aware of this problem. Also, a public healthcare safety message addressing non-COVID emergencies must be transmitted. The global healthcare policy focused on addressing the current pandemic must not disregard other serious medical emergencies. More studies are needed to assess the long term repercussion of the COVID-19 pandemic in acute cardiovascular patients.
Conflicts of interestThe authors have no conflicts of interest to declare.