Type 2 diabetes poses a significant health challenge in Portugal, increasing the susceptibility to complications/comorbidities such as hypertension, obesity, and cardiovascular (CV) disease. This study aimed to evaluate the prevalence of type 2 diabetes-related vascular complications/comorbidities and their pharmacological management in Portugal.
MethodscMORE was a non-interventional, cross-sectional, multicenter study conducted in 32 Portuguese primary healthcare units between October 2020 and 2022. Secondary data, including sociodemographic, anthropometric, clinical information, cardiometabolic comorbidities, HbA1c levels, lipid parameters and medication, were collected from electronic medical records.
ResultsSeven hundred and eighty adult patients with type 2 diabetes were included, predominantly male (55.5%), with an average age of 67.7 years and a mean disease duration of 10.5 years. Family history of type 2 diabetes (43.1%) and CV disease (32.1%) was prevalent. Mean HbA1c was 7.0%, progressively increasing with disease duration (p<0.001). Microvascular and macrovascular complications occurred in 38.1% and 19.6% of patients, respectively. The most prevalent comorbidities included overweight/obesity (85.5%), dyslipidemia (85.4%), and hypertension (82.6%). Multimorbidity burden was significant (99.3%) and positively correlated with older age, larger waist circumference, and overweight/obesity. Longer type 2 diabetes duration was associated with higher odds of diabetic retinopathy and CV disease/procedures, while dyslipidemia and hypertension were linked with older age, regardless of disease duration. Most patients received oral antidiabetic medications (94.6%), primarily biguanides (92.4%), followed by DPP-4 (39.1%) and SGLT2 inhibitors (34.2%).
ConclusionsThe cMORE study reveals a substantial burden of vascular complications/comorbidities among Portuguese patients with type 2 diabetes. Despite the high multimorbidity rates, effective type 2 diabetes management is observed, emphasizing the country's commitment to personalized care.
A diabetes mellitus tipo 2 (DMT2) representa um importante desafio para a saúde em Portugal, aumentando a suscetibilidade a complicações/comorbilidades como a hipertensão arterial, obesidade e doença cardiovascular (CV). Este estudo teve como objetivo avaliar a prevalência de complicações vasculares/comorbilidades relacionadas com a DMT2 e o seu tratamento farmacológico em Portugal.
MétodosO cMORE foi um estudo não intervencional, transversal e multicêntrico realizado em 32 unidades de cuidados de saúde primários portuguesas entre outubro de 2020 e 2022. Foram colhidos dados secundários a partir de registos médicos eletrónicos, nomeadamente informação sociodemográfica, antropométrica, clínica, comorbilidades cardiometabólicas, níveis de HbA1c, parâmetros lipídicos e medicação.
ResultadosForam incluídos 780 doentes com DMT2, predominantemente homens (55,5%), com uma idade de 67,7 anos e duração da doença de 10,5 anos, em média. A história familiar de DMT2 (43,1%) e de doença CV (32,1%) foi prevalente. A HbA1c média foi de 7,0%, aumentando progressivamente com a duração da doença (p<0,001). As complicações microvasculares e macrovasculares ocorreram em 38,1% e 19,6% dos doentes, respetivamente. As comorbilidades mais prevalentes foram o excesso de peso/obesidade (85,5%), dislipidemia (85,4%) e hipertensão arterial (82,6%). A multimorbilidade foi significativa (99,3%) e correlacionou-se positivamente com idade mais avançada, maior perímetro abdominal e excesso de peso/obesidade. A duração mais longa da DMT2 foi associada a uma maior probabilidade de retinopatia diabética e de doença/procedimentos CV, enquanto a dislipidemia e a hipertensão foram associadas à idade mais avançada, independentemente da duração da doença. A maioria dos doentes recebeu medicamentos antidiabéticos orais (94,6%), principalmente biguanidas (92,4%), seguidas de inibidores DPP-4 (39,1%) e SGLT2 (34,2%).
ConclusõesO estudo cMORE revela uma carga substancial de complicações vasculares/comorbilidades em doentes portugueses com DMT2. Apesar da elevada multimorbilidade, existe uma gestão eficaz da DMT2, com esforços para um cuidado personalizado.
Type 2 diabetes is a chronic metabolic disorder characterized by elevated blood glucose levels in patients with impaired insulin secretion and insulin resistance.1,2 With an increasing prevalence worldwide, type 2 diabetes is a significant global health concern. It is projected that it will affect 11.3% of the adult population by 2030.3–5 In Portugal, the impact of type 2 diabetes is particularly noteworthy, with an estimated prevalence of 14.1% among individuals aged 20–79 years. Furthermore, the incidence of type 2 diabetes in Portugal is known to increase with age and body mass index (BMI).6
The development of type 2 diabetes is driven by a combination of lifestyle, environmental, and genetic factors; overweight/obesity and physical inactivity are the primary risk factors.3,7 Hence, effective management of type 2 diabetes patients aims to control blood glucose levels and improve patient quality of life through a multifaceted approach involving a healthy diet, regular physical activity, and pharmacological treatment.3,8,9 When uncontrolled or poorly managed, these patients are at an increased risk of developing diabetes-related micro- and macrovascular complications and morbidity, which may ultimately lead to patient death.10–12 Common complications and comorbidities associated with type 2 diabetes include hypertension, overweight/obesity, hyperlipidemia, chronic kidney disease (CKD), and cardiovascular (CV) disease.13 In fact, CV disease and type 2 diabetes are closely associated: individuals with type 2 diabetes are at higher risk of developing CV disease,14 which is the leading cause of mortality among type 2 diabetes patients.15,16 In addition, obesity, hypertension, and dyslipidemia are not only diabetes-associated comorbidities but also major risk factors for CV disease. Thus, the coexistence and interaction of both conditions coactively amplifies the risk of CV disease in type 2 diabetes patients.17
The American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD) highlight that the pharmacological management of individuals with type 2 diabetes should be individualized, considering patient-specific characteristics and preferences, the influence of social determinants of health, disease duration, degree of hyperglycemia, presence or risk of diabetes-related comorbidities and complications, and the susceptibility to potential treatment side effects.18,19 However, the selection of appropriate antidiabetic agents is challenging, mainly because of their distinct efficacy, safety, and tolerability profiles.18,19 Moreover, type 2 diabetes patients often have a high prevalence of comorbidities, which rarely occur individually: up to 80% of type 2 diabetes patients may suffer from multimorbidity.20,21
ObjectivesIn light of the challenges associated with type 2 diabetes management and the need for a comprehensive understanding of the Portuguese real-world scenario, the cMORE study was designed to evaluate the prevalence and co-prevalence of type 2 diabetes-related vascular complications and other comorbidities in patients attending primary healthcare services in Portugal. In addition, it aimed to assess the frequency of each type 2 diabetes-related condition based on the patients’ current antidiabetic treatment. The results of this study will raise awareness among healthcare professionals regarding the most common diabetes-associated complications/comorbidities affecting Portuguese type 2 diabetes patients and contribute to optimizing patient management and the efficient allocation of healthcare resources.
MethodsStudy design and settingcMORE was a non-interventional, cross-sectional, multicenter study conducted at 32 sites across mainland Portugal, including the Norte, Lisboa e Vale do Tejo (LVT), Centro, and Alentejo regions. The study was conducted over a 2-years period, between October 2020 and 2022. Each participating site recruited participants through routine clinical practice over an average four-month period. The study relied principally on secondary data retrieval from electronic hospital databases for data collection.
Study participantsFor sample size calculation, a prevalence of 50% for each complication/comorbidity of interest in type 2 diabetes subjects was assumed. Considering a 3.5% margin of error and a 0.05 significance level, a sample of 784 subjects was estimated, distributed per Nomenclature of Territorial Units for Statistics (NUTS) according to the respective resident population. Subjects meeting all eligibility criteria were consecutively enrolled during routine diabetes appointments. To minimize selection bias, patients were recruited during morning and afternoon appointments, on alternating days. Each investigator invited the first two eligible subjects on a given day, the last two on the following day, and so forth.
Eligible patients had to meet all of the following inclusion criteria: be aged ±18 years with a diagnosis of type 2 diabetes and information on the year of diagnosis, have at least one glycated hemoglobin (HbA1c) value from the previous six months, have attended at least one diabetes appointment at the study site in the previous 12 months, and have given informed consent.
Patients with a different type of diabetes or those who were pregnant were not eligible for study participation.
Study objectivesThe cMORE study was designed primarily to assess the prevalence and co-prevalence of several diabetes-related vascular complications and comorbidities among type 2 diabetes individuals in the Portuguese primary healthcare setting. In addition, it aimed to characterize the sociodemographic, anthropometric, and clinical characteristics of type 2 diabetes patients and to analyze the frequency of complications/comorbidities based on current antidiabetic use.
Data collectionTo meet the aforementioned objectives, sociodemographic (sex, age, region [according to the NUTS classification], educational level, and smoking and alcohol habits), anthropometric (BMI and waist circumference), and clinical (presence of type 2 diabetes-related complications/comorbidities, disease duration since diagnosis, family history of type 2 diabetes and CV disease, HbA1c levels, lipid profile, estimated glomerular filtration rate [eGFR] for patients with CKD, and use of oral antidiabetics, non-insulin injectables, insulin, antiplatelets, anticoagulants, antihypertensives, statins, fibrates, and cholesterol absorption inhibitors) data were collected from electronic medical records over a mean period of four months per study center. Vascular complications and other comorbidities of interest were considered if documented in the patient's medical record and were as follows: CKD, micro- (30–299 μg/mg creatinine) and macroalbuminuria (≥300 μg/mg creatinine), diabetic retinopathy, diabetic neuropathy, CV disease or CV-related procedures (congestive heart failure, myocardial infarction, revascularization, ischemic heart disease, peripheral arterial disease, or cerebrovascular disease), dyslipidemia, pancreatitis, liver disease, hypertension, overweight/obesity, diabetic foot infection, and depression.
Statistical analysisQuantitative variables were summarized using mean and standard deviation (SD), and qualitative variables by absolute (n) and relative (%) frequencies. Data normality was assessed using the Shapiro–Wilk's test. No imputation of missing data was performed. Percentages were calculated based on non-missing values.
The total number of complications/comorbidities per patient was determined in those who had available information for all diabetes-related conditions evaluated.
Fisher's exact test was used to compare two independent groups for qualitative variables. p-Values were adjusted for multiple comparisons using the Benjamini–Hoshberg correction method. The correlation between HbA1c levels and the type 2 diabetes duration since diagnosis was estimated using the Spearman's correlation test.
To address whether the probability of each complication/comorbidity was associated with clinically relevant patient's characteristics, multivariable logistic regression models were adjusted considering each type 2 diabetes-related condition as a dependent variable and the following characteristics as independent variables: gender, age, geographic region, educational level, type 2 diabetes disease duration since diagnosis, BMI, waist circumference, HbA1c level, and use of oral antidiabetic agents, insulin, or non-insulin injectables.
A two-sided p-value of <0.05 was considered statistically significant in all analyses. Computations were implemented in Python 3.6 but using statistical methods from R® software version 4.1.2 (Vienna, Austria).
Ethics declarationThis study was conducted in accordance with the Good Pharmacoepidemiology Practices and with the ethical principles of the Declaration of Helsinki. The study protocol was approved by the local ethics committee and managing board of each participating site. Informed consent was obtained from all study participants.
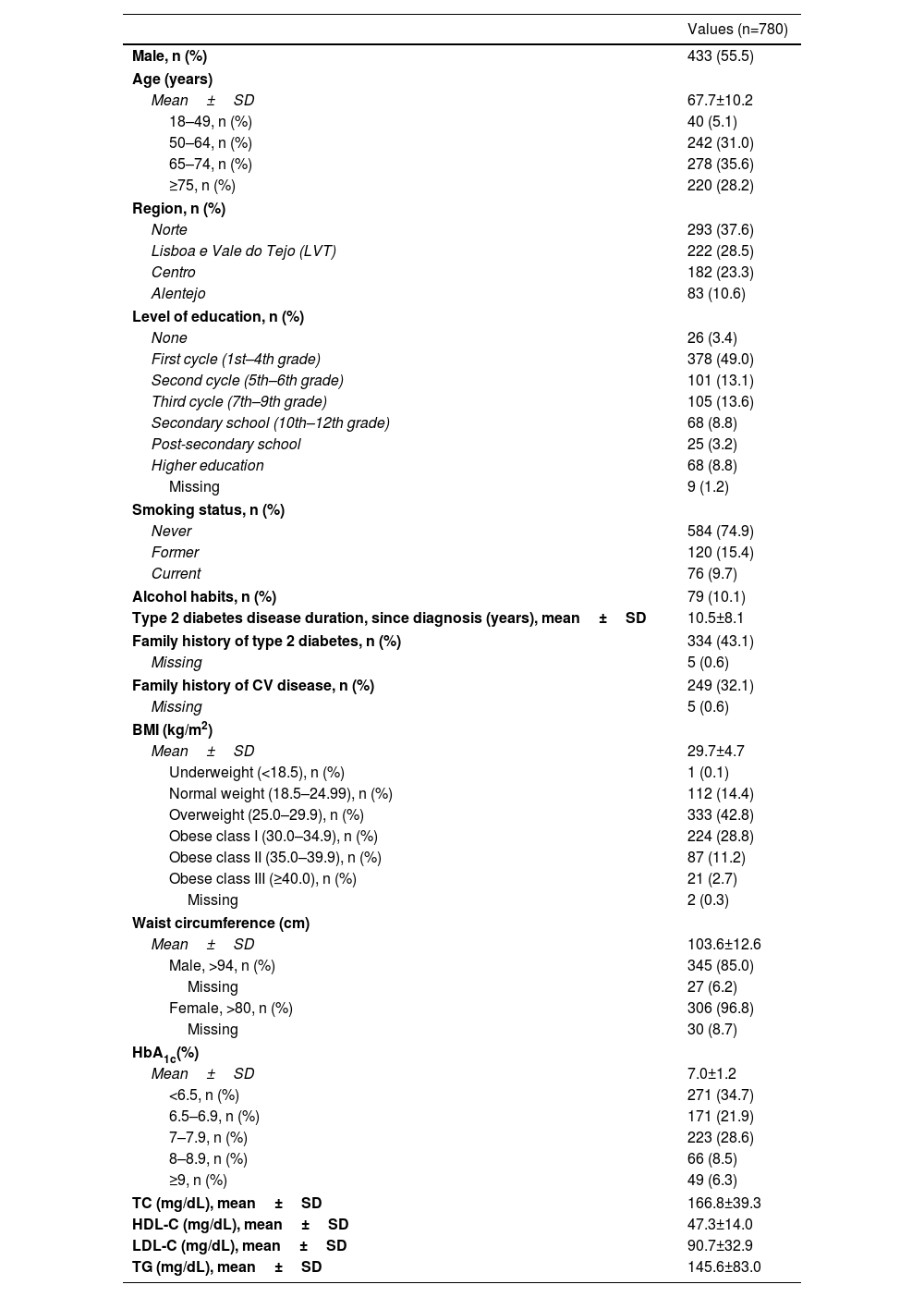
ResultsSociodemographic, anthropometric, and clinical characteristics of the study sampleOf the 795 type 2 diabetes patients who were assessed for eligibility, 15 failed screening and the other 780 met the eligibility criteria and were included in the study. The sociodemographic, anthropometric, and clinical characteristics of the 780 type 2 diabetes patients at the time of study enrollment are presented in Table 1.
Patient sociodemographic, anthropometric, and clinical characteristics at enrollment.
| Values (n=780) | |
|---|---|
| Male, n (%) | 433 (55.5) |
| Age (years) | |
| Mean±SD | 67.7±10.2 |
| 18–49, n (%) | 40 (5.1) |
| 50–64, n (%) | 242 (31.0) |
| 65–74, n (%) | 278 (35.6) |
| ≥75, n (%) | 220 (28.2) |
| Region, n (%) | |
| Norte | 293 (37.6) |
| Lisboa e Vale do Tejo (LVT) | 222 (28.5) |
| Centro | 182 (23.3) |
| Alentejo | 83 (10.6) |
| Level of education, n (%) | |
| None | 26 (3.4) |
| First cycle (1st–4th grade) | 378 (49.0) |
| Second cycle (5th–6th grade) | 101 (13.1) |
| Third cycle (7th–9th grade) | 105 (13.6) |
| Secondary school (10th–12th grade) | 68 (8.8) |
| Post-secondary school | 25 (3.2) |
| Higher education | 68 (8.8) |
| Missing | 9 (1.2) |
| Smoking status, n (%) | |
| Never | 584 (74.9) |
| Former | 120 (15.4) |
| Current | 76 (9.7) |
| Alcohol habits, n (%) | 79 (10.1) |
| Type 2 diabetes disease duration, since diagnosis (years), mean±SD | 10.5±8.1 |
| Family history of type 2 diabetes, n (%) | 334 (43.1) |
| Missing | 5 (0.6) |
| Family history of CV disease, n (%) | 249 (32.1) |
| Missing | 5 (0.6) |
| BMI (kg/m2) | |
| Mean±SD | 29.7±4.7 |
| Underweight (<18.5), n (%) | 1 (0.1) |
| Normal weight (18.5–24.99), n (%) | 112 (14.4) |
| Overweight (25.0–29.9), n (%) | 333 (42.8) |
| Obese class I (30.0–34.9), n (%) | 224 (28.8) |
| Obese class II (35.0–39.9), n (%) | 87 (11.2) |
| Obese class III (≥40.0), n (%) | 21 (2.7) |
| Missing | 2 (0.3) |
| Waist circumference (cm) | |
| Mean±SD | 103.6±12.6 |
| Male, >94, n (%) | 345 (85.0) |
| Missing | 27 (6.2) |
| Female, >80, n (%) | 306 (96.8) |
| Missing | 30 (8.7) |
| HbA1c(%) | |
| Mean±SD | 7.0±1.2 |
| <6.5, n (%) | 271 (34.7) |
| 6.5–6.9, n (%) | 171 (21.9) |
| 7–7.9, n (%) | 223 (28.6) |
| 8–8.9, n (%) | 66 (8.5) |
| ≥9, n (%) | 49 (6.3) |
| TC (mg/dL), mean±SD | 166.8±39.3 |
| HDL-C (mg/dL), mean±SD | 47.3±14.0 |
| LDL-C (mg/dL), mean±SD | 90.7±32.9 |
| TG (mg/dL), mean±SD | 145.6±83.0 |
BMI: body mass index; CV: cardiovascular; HbA1c: glycated hemoglobin; HDL-C: high density lipoprotein cholesterol; LDL-C: low density lipoprotein cholesterol; NUTS: Nomenclature of Territorial Units for Statistics; SD: standard deviation; TC: total cholesterol; TG: triglycerides.
The study sample consisted predominantly of male participants (n=433, 55.5%) with a mean age of 67.7±10.2 years. Geographically, the Norte region had the highest representation with 37.6% (n=293) of the participants, followed by LVT with 28.5% (n=222), Centro with 23.3% (n=182), and Alentejo with 10.6% (n=83). Never smokers (n=584, 74.9%) and individuals without alcohol consumption habits (n=701, 89.9%) were abundant among this sample. Family history of type 2 diabetes was present in 43.1% of the patients (n=334), while 32.1% (n=249) had a family history of CV disease. The average duration of type 2 diabetes diagnosis was 10.5±8.1 years, with a mean BMI of 29.7±4.7 kg/m2 and waist circumference of 103.6±12.6 cm.
Mean HbA1c level from the previous 6 months was 7.0±1.2%, which increased significantly with longer type 2 diabetes disease duration (ρ=0.231, p<0.001; Figure S1). Nevertheless, 56.7% of the patients (n=442) achieved target glycemic control of HbA1c <7%. Lipid parameters collected during the 12 months prior to study entry were also evaluated and are detailed in Table 1.
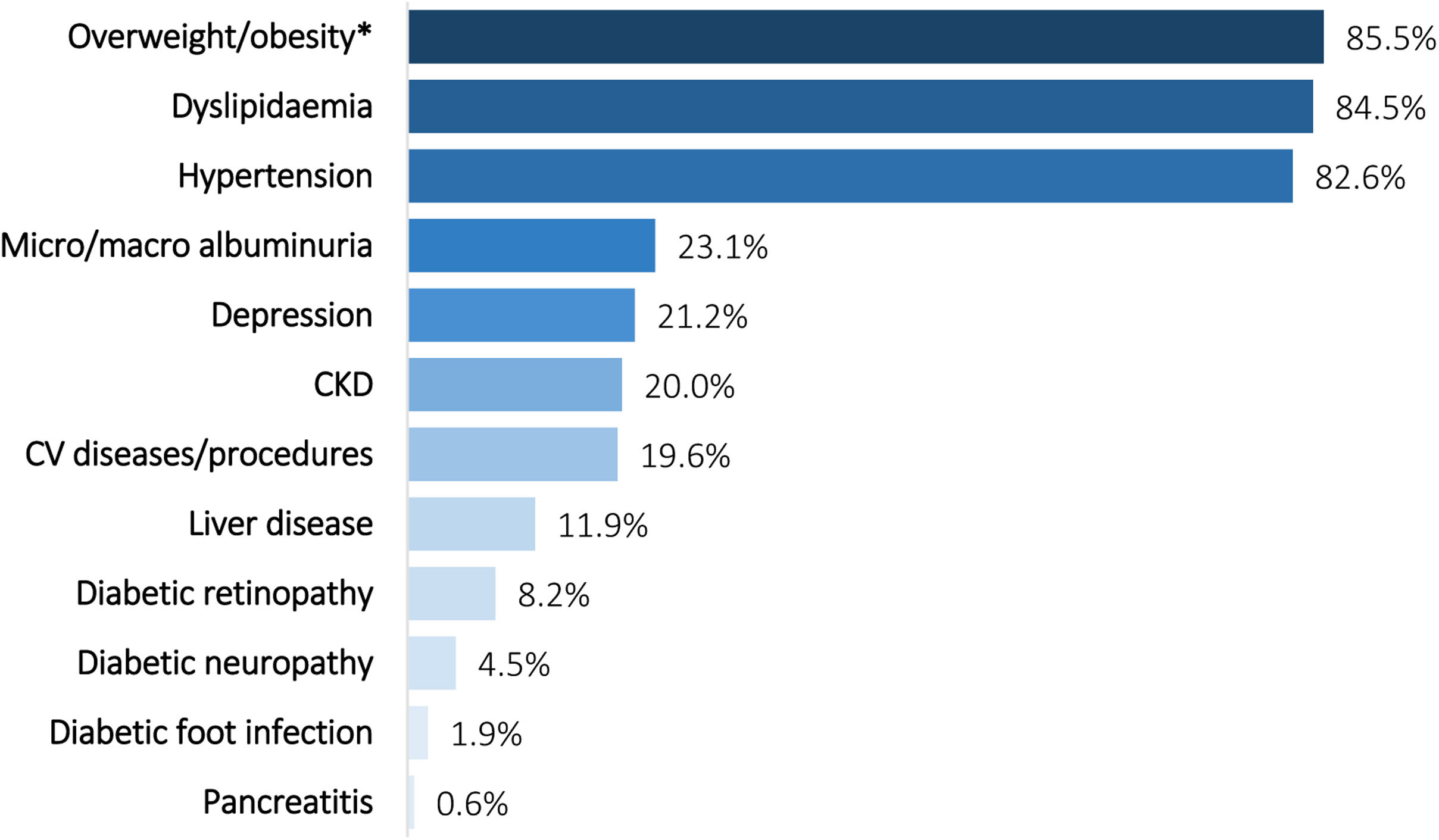
Vascular complications and other comorbidities of type 2 diabetes patientsOverall, this sample had a high prevalence of complications and comorbidities: 5.0% (n=32) of patients had one complication or comorbidity and 94.3% (n=598) had two or more (based on the 634 patients with available information on all complications/comorbidities). Microvascular complications, including CKD, micro- and macroalbuminuria, diabetic neuropathy, diabetic retinopathy, and diabetic foot infections, were observed in 38.1% (n=297) of patients, while macrovascular complications, including CV diseases and procedures, were present in 19.6% (n=153). Additionally, 99.1% (n=773) of participants had comorbidities, including being overweight/obesity, dyslipidemia, hypertension, pancreatitis, liver disease, and depression.
The most prevalent type 2 diabetes-related conditions were overweight/obesity (n=665, 85.5%), dyslipidemia (n=666, 85.4%), and hypertension (n=644, 82.6%), followed by micro/macroalbuminuria (n=146, 23.1%), depression (n=165, 21.2%), CKD (n=156, 20.0%), and CV disease/procedures (n=153, 19.6%) (Figure 1 and Table S1). Patients with CKD had a mean eGFR value of 57.4±22.6 mL/min/1.73 m2.
The probability of having each complication/comorbidity was evaluated based on clinically relevant patient characteristics, and those that significantly contributed to this probability are detailed in Table S2. The analysis focused specifically on whether the duration of type 2 diabetes affected this probability when controlling for a possible confounding effect of the patient's age. The analysis revealed that the longer the duration of type 2 diabetes, the higher the chance of the patients having diabetic retinopathy (odds ratio [OR]=2.531; p=0.006) and CV disease/procedures (OR=1.571; p=0.021), independent of the patient's age. Concerning CV disease/procedures, female gender (OR=0.530; p=0.001) and insulin use (OR=2.504; p<0.001) were also independently correlated with the probability of patients having this vascular complication. On the other hand, older patients were more likely to have dyslipidemia (50–64 years: OR=5.424, p<0.001; 65–74 years: OR=7.603, p<0.001; ±75 years: OR=7.430, p<0.001) and hypertension (65–74 years: OR=3.376, p=0.003; ≥75 years: OR=8.193, p<0.001) than those aged 18–49 years, regardless of the duration of the type 2 diabetes. None of the other type 2 diabetes-related conditions showed a significant association with either disease duration or patient age.
Regarding multimorbidity, the most common combination of conditions was the presence of overweight/obesity, dyslipidemia, and hypertension (n=126, 19.9%); followed by overweight/obesity, dyslipidemia, hypertension, and depression (n=41, 6.5%); overweight/obesity and dyslipidemia (n=35, 5.5%); and overweight/obesity, dyslipidemia, hypertension, and micro- or macroalbuminuria (n=28, 4.4%) (Table S3). The burden of multimorbidity was greater in older patients (≥2 complications/comorbidities: 18–49 years=85.3% vs. 50–64 years=90.9% vs. 65–74 years=96.0% vs. ≥75 years=97.8%; p=0.023), among female or male subjects with waist circumferences >80 and 94 cm, respectively (female ≤80=71.4% vs. female >80=96.0% vs. male ≤94=75.5% vs. male >94=96.4%; p<0.001), and in those overweight/obese (underweight/normal weight=77.9% vs. overweight=96.7% vs. obese class I=97.7% vs. obese class II=98.6% vs. obese class III=100.0%; p<0.001).
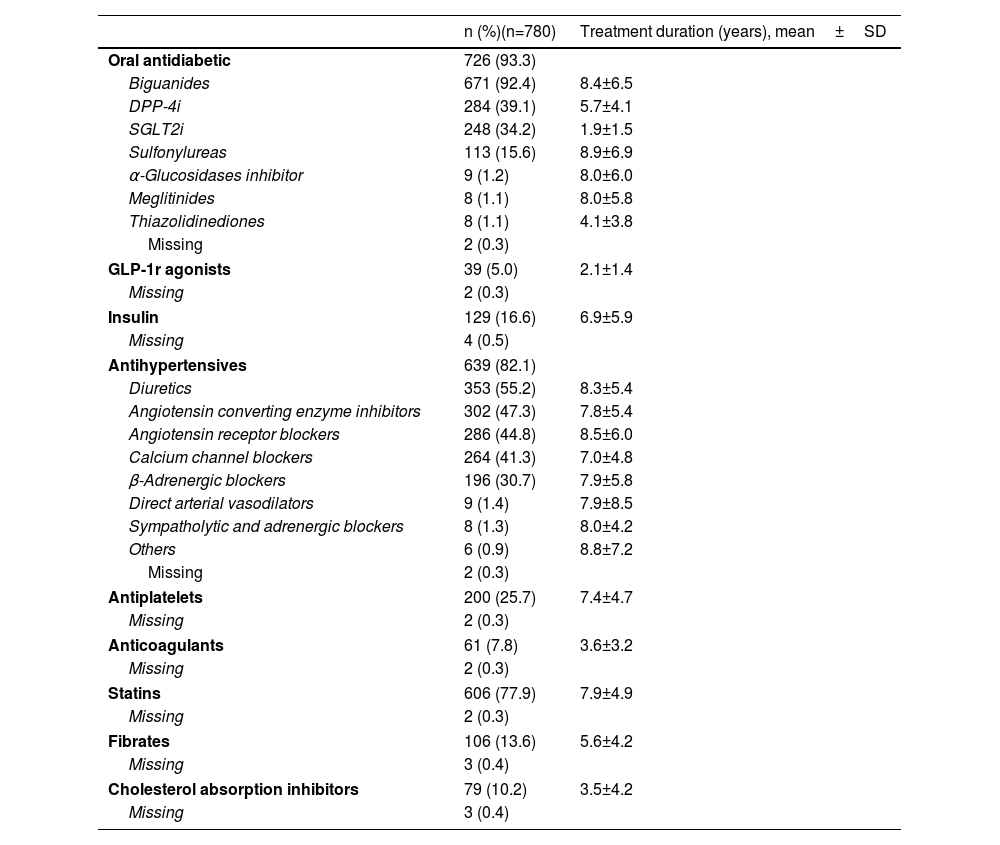
Pharmacological management of type 2 diabetes patientsPharmacologic management of participants involved the use of different therapeutic classes. The most frequently prescribed medications were oral antidiabetics (n=726, 93.3%), antihypertensives (n=639, 82.1%), and statins (n=607, 77.9%), as outlined in Table 2. A smaller group of patients also received insulin (n=129, 16.6%) and glucagon-like peptide 1 receptor (GLP-1r) agonists (n=39, 5.0%) for glycemic control, as well as fibrates (n=106, 13.6%) and cholesterol absorption inhibitors (n=79, 10.2%) as cholesterol-lowering agents. Table 2 also shows the duration of treatment with each therapeutic class since initiation.
Pharmacologic agents used for the treatment of type 2 diabetes patients at study enrollment.
| n (%)(n=780) | Treatment duration (years), mean±SD | |
|---|---|---|
| Oral antidiabetic | 726 (93.3) | |
| Biguanides | 671 (92.4) | 8.4±6.5 |
| DPP-4i | 284 (39.1) | 5.7±4.1 |
| SGLT2i | 248 (34.2) | 1.9±1.5 |
| Sulfonylureas | 113 (15.6) | 8.9±6.9 |
| α-Glucosidases inhibitor | 9 (1.2) | 8.0±6.0 |
| Meglitinides | 8 (1.1) | 8.0±5.8 |
| Thiazolidinediones | 8 (1.1) | 4.1±3.8 |
| Missing | 2 (0.3) | |
| GLP-1r agonists | 39 (5.0) | 2.1±1.4 |
| Missing | 2 (0.3) | |
| Insulin | 129 (16.6) | 6.9±5.9 |
| Missing | 4 (0.5) | |
| Antihypertensives | 639 (82.1) | |
| Diuretics | 353 (55.2) | 8.3±5.4 |
| Angiotensin converting enzyme inhibitors | 302 (47.3) | 7.8±5.4 |
| Angiotensin receptor blockers | 286 (44.8) | 8.5±6.0 |
| Calcium channel blockers | 264 (41.3) | 7.0±4.8 |
| β-Adrenergic blockers | 196 (30.7) | 7.9±5.8 |
| Direct arterial vasodilators | 9 (1.4) | 7.9±8.5 |
| Sympatholytic and adrenergic blockers | 8 (1.3) | 8.0±4.2 |
| Others | 6 (0.9) | 8.8±7.2 |
| Missing | 2 (0.3) | |
| Antiplatelets | 200 (25.7) | 7.4±4.7 |
| Missing | 2 (0.3) | |
| Anticoagulants | 61 (7.8) | 3.6±3.2 |
| Missing | 2 (0.3) | |
| Statins | 606 (77.9) | 7.9±4.9 |
| Missing | 2 (0.3) | |
| Fibrates | 106 (13.6) | 5.6±4.2 |
| Missing | 3 (0.4) | |
| Cholesterol absorption inhibitors | 79 (10.2) | 3.5±4.2 |
| Missing | 3 (0.4) | |
DPP-4i: dipeptidyl-peptidase-4 inhibitor; GLP-1r: glucagon-like peptide receptor 1; SD: standard deviation; SGLT2i: sodium glucose cotransporter 2 inhibitor.
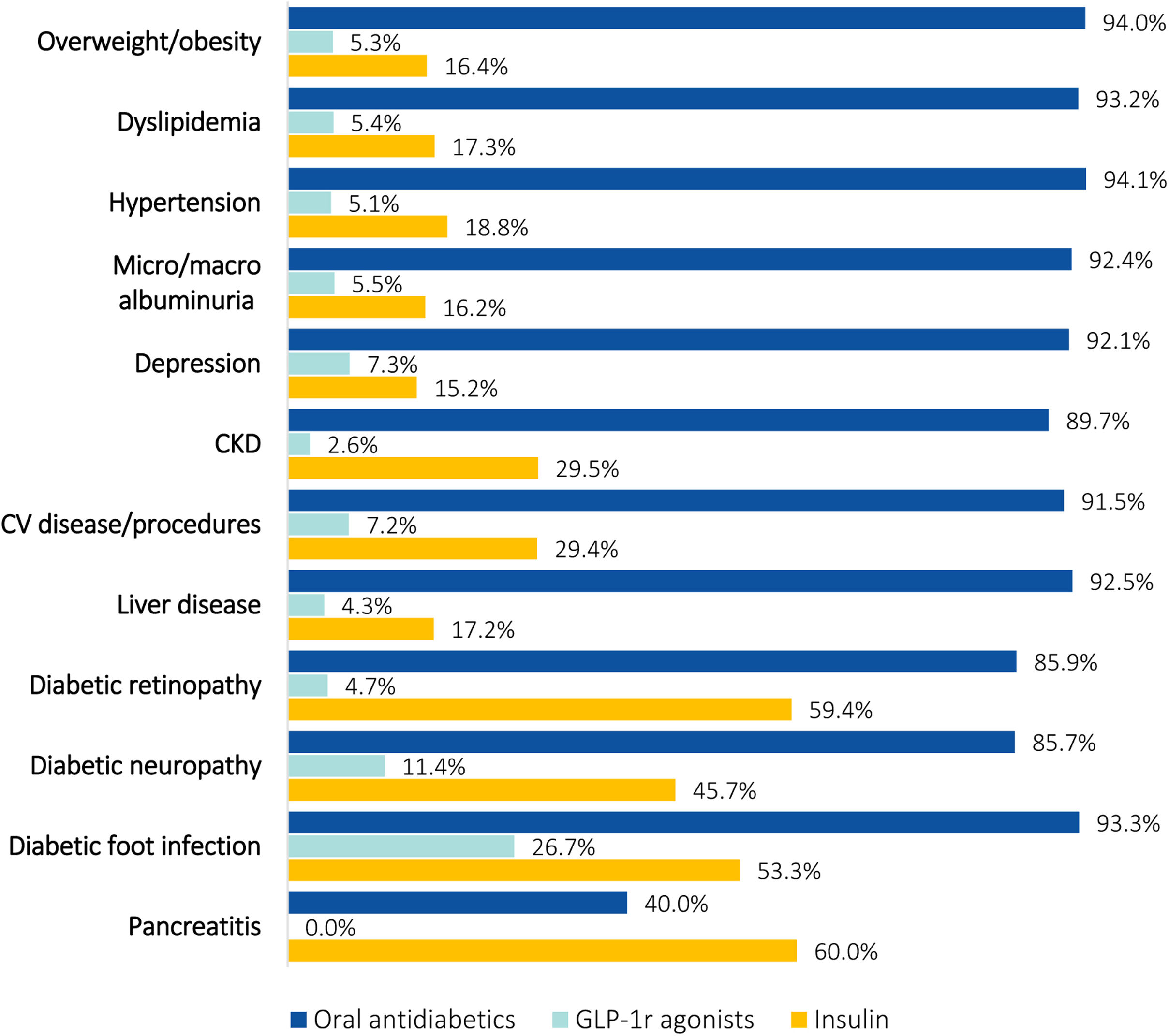
Among the 738 patients (94.9%) who received antidiabetic agents, the most common treatment was biguanide monotherapy (n=245, 31.5%), as shown in Table S4. A total of 585 patients (75.2%) were solely on oral medication, 101 (13.0%) were on a combination of oral medication and insulin, 23 (3.0%) combined oral medication with GLP-1r agonists, 15 (1.9%) were on oral medication combined with GLP-1r agonists and insulin, 13 (1.7%) were using insulin alone, and 1 (0.1%) was using GLP-1r agonists alone. The distribution of these antidiabetic classes – oral medication, GLP-1r agonists, and insulin – according to each complication/comorbidity is presented in Figure 2 and Table S5. Oral antidiabetics were widely prescribed in patients with various complications/comorbidities. Insulin usage was more frequent in patients with diabetic retinopathy (n=38, 59.4%), diabetic neuropathy (n=16, 45.7%), and diabetic foot infection (n=8, 53.3%).
An assessment of the prevalence of each complication/comorbidity by the type of antidiabetic regimen revealed that patients treated with a combination of oral antidiabetics and insulin were more likely to have certain complications/comorbidities compared to those taking oral antidiabetics alone. These included hypertension (p=0.004), higher creatinine levels (p=0.005), CKD (p<0.001), diabetic retinopathy (p<0.001), CV diseases/procedures (p<0.001) – namely ischemic heart disease (p=0.008), cerebrovascular disease (p=0.045) and peripheral artery disease (p=0.004), as well as diabetic neuropathy (p=0.002) and diabetic foot infection (p=0.022) (Table S6). The distribution of each complication/comorbidity among patients receiving the five most common antidiabetic regimens and those taking or not taking oral antidiabetics is detailed in Tables S7 and Table S8.
DiscussionThe cMORE study provides valuable insights into the sociodemographic and clinical characteristics, multimorbidity patterns, and pharmacologic management of patients with type 2 diabetes attending primary healthcare services in mainland Portugal. The findings of this study shed light on several important aspects of the disease, allowing for a comprehensive understanding of its complexity and the challenges associated with its management.
The sociodemographic and clinical characteristics of this sample are consistent with those of the primary care TEDDI study22 and of the overall Portuguese type 2 diabetes population, as reported in the Annual Report of the Portuguese Diabetes Society released in 2023.6 Patients were predominantly male and overweight, with a mean age of 67.7 years. The higher prevalence of type 2 diabetes in older individuals is in line with previous research13,23–25 and emphasizes the age-related risk factors associated with the disease, namely the co-prevalence of vascular complications and comorbidities.
This study examined the multimorbidity burden among type 2 diabetes patients and revealed a high prevalence of vascular complications and comorbidities. Overweight/obesity, dyslipidemia, and hypertension emerged as the most common type 2 diabetes-related conditions, and those with the highest co-prevalence, followed by the vascular complications micro- and macroalbuminuria, CKD, and CV diseases/procedures. This finding underscores the strong connection between type 2 diabetes and these conditions. In particular, there was a correlation between the duration of type 2 diabetes and diabetes-associated complications, namely CV disease/procedures. Concurrently, comorbidities such as dyslipidemia and hypertension were linked to the patient's age, thereby adding a layer of complexity to patient monitoring and treatment. Multimorbidity was present in the vast majority of patients and increased with age, BMI, and waist circumference. These findings are consistent with previous studies,13,24,26 although the prevalence of specific conditions may vary given the different sample characteristics, definitions of diabetes-related conditions evaluated, and type of data source.
Concerning vascular complications, the rates of micro- (38.1%) and macrovascular (19.6%) complications differ from other large multinational observational studies. The A1chieve27 (microvascular: 52.6%; macrovascular: 26.7%) and IMPROVE28 (microvascular: 45.0%; macrovascular: 28.0%) studies reported higher rates of vascular complications compared to the present study, whereas the DISCOVER study29 (microvascular: 18.8%; macrovascular: 12.7%) reported lower rates. While patients in these three studies were younger, had shorter disease duration, and higher HbA1c levels than the population in this study, the prevalence of vascular complications also differed between them. Nevertheless, in the A1chieve,27 DISCOVER,29 and cMORE, the likelihood of CV macrovascular complications was positively associated with similar variables, namely male sex and longer disease duration. Considering that intensive glycemic control has a beneficial effect on the incidence and progression of vascular complications,10–12,30 the observed differences between studies may result from different treatment approaches, patient adherence, or even access to treatment.
Most patients achieved the glycemic target of HbA1c <7%, as per the consensus guidelines of the ADA and EASD available at the time of patient enrolment,31–35 and in line with a previous study conducted in Portugal that showed good glycemic control (HbA1c <7%: 64.8%) in primary care patients.22 However, these guidelines also emphasize the importance of individualizing glycemic targets based on patient characteristics (e.g., age, social determinants of health, and disease duration), multimorbidity profile or risk of diabetes-related comorbidities and complications, and risk for adverse events to therapy (such as hypoglycemia), suggesting that less stringent HbA1c levels may be acceptable for certain patients.18,19,36,37 Given this sample's characteristics, where older patients had more multimorbidity and longer disease duration was associated with higher HbA1c levels,22 it is possible that more individuals achieved satisfactory glycemic control and appropriate disease management, justifying the acceptable rates of vascular complications. This assumption is further supported by the low frequency of type 2 diabetes patients with CV disease or requiring CV-associated procedures, despite the high incidence of major CV risk factors such as hypertension, obesity, and hyperlipidaemia.17 Still, the probability of having CV disease/procedures independently increased with longer disease duration, regardless of patient characteristics, accentuating the need for closer monitoring of patients who have lived with the disease for a long time (>10.5 years).
Glycemic control is not the only goal in the management of patients with type 2 diabetes. Clinicians also need to address the complications and comorbidities associated with diabetes, as these affect patients’ quality of life and potentially lead to anxiety and depression.18,38,39 In this context, selecting the most appropriate pharmacological treatment is a challenge, as it may adversely affect other existing conditions.18 Almost all patients of this study were prescribed glucose-lowering agents, with oral antidiabetics being the most frequent option. Among these, biguanides were the most common class and were most likely to be prescribed to patients initiating pharmacological treatment or achieving sustained glycemic targets.18,33 Insulin and GLP-1r agonists were used in a smaller subset of patients. The antidiabetic regimens varied according to the presence of complications and comorbidities, suggesting a personalized approach to treatment. Oral antidiabetics in combination with insulin were prescribed more frequently than oral agents alone for patients with hypertension, micro- or macroalbuminuria, CKD, CV disease/procedures, diabetic retinopathy, diabetic neuropathy, and diabetic foot infection. This implies that patients with more advanced disease may require intensified treatment regimens with insulin to achieve glycemic targets and delay the progression of additional vascular complications.10–12,30
Despite SGLT2i and GLP-1r agonists having a cardiorenal-protective role and being recommended for patients at high risk of or with established CV or renal diseases,18,31 their use in this study did not align with those recommendations. Indeed, the frequency of patients with CV disease or CKD who were receiving SGLT2i and biguanides dual therapy was similar to those receiving biguanides alone or combined with other oral agents. However, it is important to note that the guidelines with those recommendations were established shortly before the initiation of this study and their implementation can be a lengthy process, which may have been further delayed by the COVID-19 pandemic. Further evaluation is necessary to gain a deeper understanding of glucose-lowering prescription practices and whether they comply with current guidelines.
The cMORE study has several strengths, including its multicenter design and large number of enrolled patients, providing a representative sample of the mainland Portuguese scenario in terms of type 2 diabetes patient characteristics and prevalence of associated complications/comorbidities. Additionally, the study provides detailed associations between type 2 diabetes-related complications/comorbidities, highlighting patient characteristics that need to be considered in the Portuguese healthcare system when monitoring an individual with type 2 diabetes, and the use of antidiabetic agents.
However, there are some limitations to consider. Firstly, the COVID-19 pandemic affected the format of patient clinical appointments and data collection (e.g., anthropometric data). It also impacted the introduction and access to new glucose-lowering therapies. Secondly, the electronic case report form used in the study only allowed for six pre-defined options for CV disease/procedures, which may have affected the reporting of these parameters as patients with other CV problems were considered to have no CV disease or CV-related procedures. Finally, the cross-sectional nature of the study prevents the establishment of temporal relationships and inferences. A longitudinal analysis would provide evidence on whether patients are being properly managed at diagnosis of both the disease and associated complications/comorbidities. Also, evaluation of patient education about type 2 diabetes and lifestyle choices would offer valuable guidance on optimal strategies to implement throughout the course of the disease, in order to reduce the therapeutic burden, prevent health deterioration, and improve patients’ quality of life.
ConclusionsThe cMORE study provides valuable insights into the prevalence and co-prevalence of type 2 diabetes-related vascular complications and comorbidities among adult patients with type 2 diabetes in the primary healthcare setting of mainland Portugal. The study demonstrates a tailored approach to treatment, with the incorporation of insulin in patients with vascular complications and highlights important considerations regarding type 2 diabetes pharmacological treatment. Despite the high rates of multimorbidity observed, vascular complications were present at a reasonable level. This, coupled with the satisfactory HbA1c levels achieved by most patients, indicates there is good management of type 2 diabetes in this population. Altogether, these findings underscore the importance of individualized management plans that take into account the unique clinical characteristics and associated comorbidities of patients with type 2 diabetes, starting from the time of diagnosis. Larger-scale studies with extended follow-up periods could provide further understanding of the long-term outcomes of these management strategies and their impact on patient health. By optimizing glycemic control and addressing concurrent conditions, healthcare providers can strive to enhance patient outcomes and mitigate the overall burden of type 2 diabetes.
FundingFunding for this research was provided by MSD Portugal (Protocol NIS008358).
Author contributionsAll authors are responsible for the work described in this paper. S. Alão: Study conception; T. Silva, A.P. Leite, M. Rosário, C. Carvalho, J. Coelho, H. Ferreira, R. Ferreira, J. Abreu, M. Rosa, S. Azevedo, C. Cunha, C. Daniel, B. Juane and R.A. Sousa: Data collection and analysis. All authors participated in the interpretation of data, revised the manuscript for important intellectual content and provided final approval of the version to be published. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Conflicts of interestSA and ACC are employees of MSD Portugal, who may own stock and/or hold stock options in Merck & Co., Inc., Rahway, NJ, USA.
Medical writing and/or editorial assistance was provided by Joana Melo and Carla Gomes (W4Research), statistical support from Adriana Belo (W4Research), and project management by Carolina Moura (MSD Portugal) and Nélia Lima (W4Research), all funded by MSD Portugal.
The authors would also like to express their gratitude to all the investigators involved in this study, namely: Dr. Andreia Chaves Cerejo, Dr. Carlos Franclim, Dr. Diana Oliveira, Dr. Ilda Gonçalves, Dr. Inês Freitas, Dr. Leonor Carrapatoso, Dr. Liliana Costa, Dr. Rachel Barbabela (Unidade Local de Saúde de Matosinhos), Dr. Carina Matos, Dr. Joana Sousa, Dr. Joana Gonçalves, Dr. Ana Coroas, Jorge Azevedo (USF Gil Eanes), Dr. Joana Torres, Dr. Fátima Cruz, Dr. Ana Rafaela Gave (USF Uarcos), Dr. Liliana Marto, Dr. Tiago Baptista, Dr. Sara Araújo (USF Tiago D’Almeida), Dr. Mariana Oliveira, Dr. Joana Lascasas, Dr. Cristina Mendes, Dr. Catarina Campos, Dr. Vera Silva (UCSP Caminha), Dr. Ana Carla Bernardes, Dr. Ana Margarida Gonçalves, Dr. Joana Antunes, Dr. Mariana Coimbra (USF Santiago), Dr. Inês Migueis Ferreira, Dr. Ana Rafaela Esperança (USF Flor de Sal), Dr. Diana Roda, Dr. Joana Gonçalves (UCSP Coimbra Celas), Dr. Daniela Fernandes, Dr. Linda Costa, Dr. Joana Pinto (UCSP Cantanhede), Dr. Liliana Andrade, Dr. Sofia Ribeiro (UCSP Tábua), Dr. Vasco Almeida e Mota, Dr. Dalila Teixeira, Dr. Alyona Koshelnyk (UCSP Torres Vedras), Dr. Mariana Domingues, Dr. Ana Laura, Dr. Camila Ribeiro, Dr. Catarina Alves, Dr. Cláudia Mourato Silva, Dr. Nuno Kakoo, Dr. Patrícia Ferrão (USF Villa Longa), Dr. Francisco Antunes (UCSP Azeitão), Dr. Pedro Alves, Dr. Paula Silva, Dr. Ana Magalhães (USF Conchas), Dr. Edmundo Sá (UCSP Serpa), Dr. Luís Coentro, Dr. Ana Sotero (USF Alfa Beja), Dr. Andreia Oliveira, Dr. Sara Veiga, Dr. Edite Reis, and Dr. Nuno Estradas (UCSP Beja).