Despite the well-known health benefits of regular physical activity, sedentary behavior and physical inactivity remain a real global pandemic. Exercise is associated with increased life expectancy, improved quality of life and prevention of multiple diseases. Although less implemented in practice compared to aerobic exercise, recent evidence shows that resistance exercise (RE) is also responsible for various benefits, including improvements in body composition, control of several cardiovascular (CV) risk factors, and reduction of CV outcomes. RE increases strength and muscle mass, is effective in controlling type 2 diabetes, and improves the management of obesity, lipids, and blood pressure profiles. In this setting, clinical guidelines recommend the inclusion of RE for primary and secondary CV risk prevention, particularly in combination with aerobic exercise, in which the benefits are most pronounced. Prescription of RE should follow a methodology that includes key variables such as frequency, intensity, type, time, and progression. Despite challenges, professionals in the CV field should be familiar with RE prescription in order to maximize its referral in clinical practice. This review aims to analyze the CV effects of RE and current recommendations regarding the prescription of this type of exercise.
Apesar dos benefícios conhecidos da atividade física para a saúde, o sedentarismo e a inatividade física continuam a ser uma verdadeira pandemia em termos globais. O exercício está associado ao aumento da sobrevida, à melhoria da qualidade de vida e à prevenção de múltiplas doenças. Embora esteja menos implementado na prática quando comparativamente ao exercício aeróbio, a evidência mostra que o exercício de força (EF) também é responsável por múltiplos benefícios, incluindo melhoria na composição corporal, controlo de vários fatores de risco cardiovascular (CV) e redução de eventos CV. O EF aumenta a força e a massa muscular, é eficaz no controlo da diabetes mellitus tipo 2 e melhora o controlo da obesidade e dos perfis lipídico e da pressão arterial. Neste cenário, as recomendações clínicas advogam a inclusão do EF como medida essencial na prevenção CV primária e secundária, nomeadamente em combinação com exercício aeróbio, pelos benefícios mais pronunciados. A prescrição de EF deve seguir uma metodologia que inclua variáveis-chave como frequência, intensidade, tipo, tempo e progressão. Apesar dos desafios, os profissionais da área CV devem estar familiarizados com a prescrição de EF para maximizar a sua aplicação na prática clínica. Esta revisão tem como objetivo analisar os efeitos CV do EF e as recomendações atuais quanto à prescrição deste tipo de exercício.
A sedentary lifestyle is a well-known risk factor for poor clinical outcomes, including adverse cardiovascular (CV) events and many other conditions such as diabetes, hypertension, obesity, hypercholesterolemia, cancer, and metabolic and neurodegenerative diseases. Physical inactivity is a leading independent predictor for CV disease (CVD) and constitutes a global pandemic that has been identified as one of the four leading contributors to premature mortality, affecting a wide spectrum of the population, from young to older individuals, especially in developed countries.1
Regular physical exercise is associated with various health benefits, including longer life expectancy, improvement in quality of life and lower rates of multiple diseases. As CVD remains a leading cause of death worldwide, especially due to ischemic and cerebrovascular disease, the beneficial effect of exercise is more marked in these clinical conditions. Additionally, the most prevalent CV risk factors can be modified by the adoption of a healthy lifestyle, of which exercise is one of the core components. These benefits can be a valuable part of both primary and secondary CV prevention. The effects of exercise are not limited to CVD, but extend to other conditions, including musculoskeletal, endocrine, respiratory, oncological, psychiatric and neurological diseases.2
Many of the mechanisms responsible for these benefits are traditionally attributable to the positive effects of regular aerobic exercise training; there is in clinical practice a certain reluctance regarding the prescription of resistance exercise (RE). However, an emerging body of evidence shows that RE appears to be effective and safe in preventing and reducing the risk of CVD and other chronic diseases and mortality, and in improving quality of life. These clinical benefits are dramatically increased when combined with aerobic exercise.
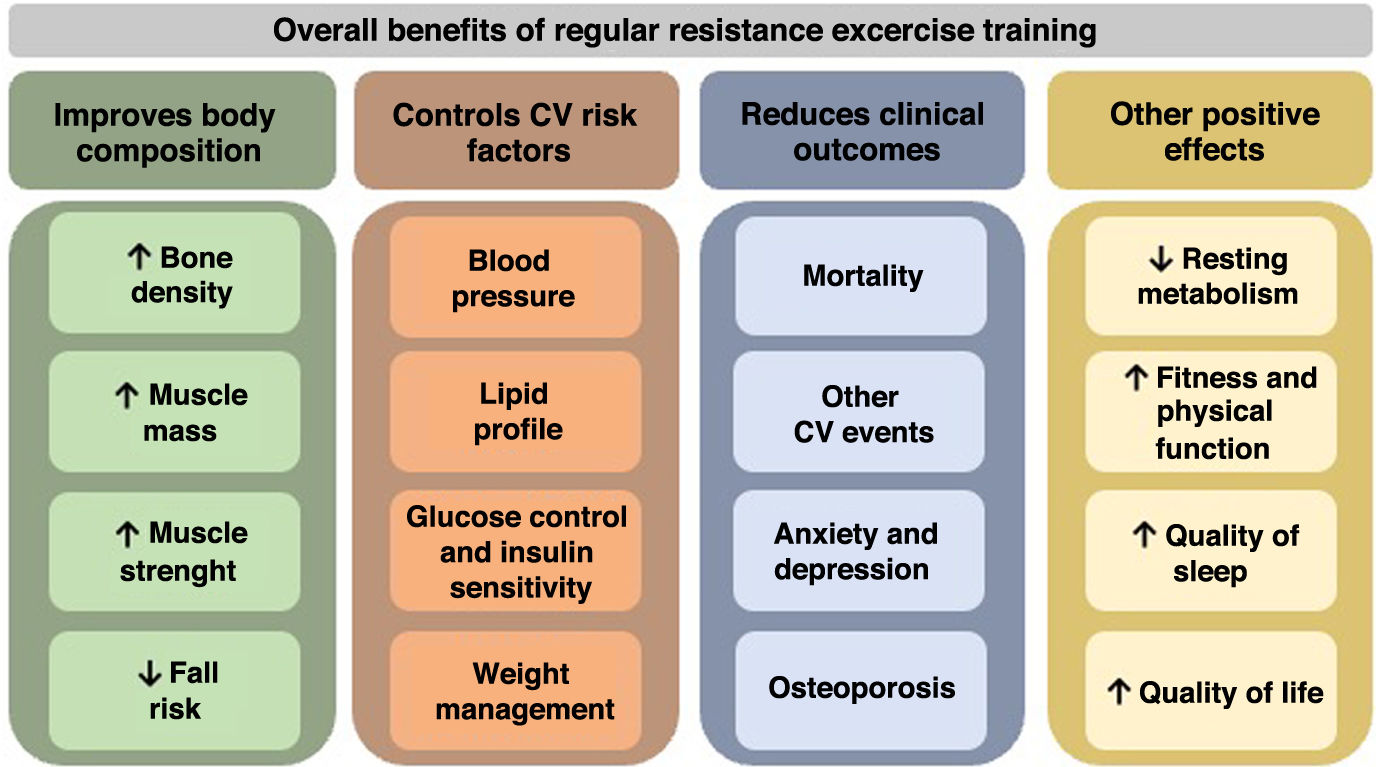
Skeletal muscle represents up to 40% of total body weight and positively influences several metabolic risk factors.3 As muscle mass declines by between 3% and 8% for each decade after age 30, leading to approximately 0.2 kg of lean weight loss per year, and given the impact of sarcopenia in increasingly sedentary and aging populations, the muscle gains promoted by RE take on a more important role.4–7 The positive changes in body composition and the control of CV risk factors induced by RE are reflected in a lower frequency of major clinical outcomes (Figure 1).
In this context, the most recent guidelines for CV prevention and exercise prescription from various international health and exercise organizations are consistent in recommending the prescription of RE combined with aerobic exercise.8 The combination of regular RE and aerobic exercise training may be an optimal strategy to improve adherence and clinical outcomes.
Individualized assessment and prescription of RE is essential but somewhat challenging. In the same way as for aerobic exercise, RE prescription should follow a methodology that considers multiple characteristics and key components, such as frequency, intensity, time, type, and progression. In practice, RE involves lifting weights, using machines or free weights, the intensity being prescribed according to specific methods, such as the one-repetition maximum (1RM), defined as the heaviest weight a person can lift with maximum effort in a single repetition.9 The involvement of health and exercise professionals with experience in the field is essential, especially in cases in which the exercise prescription is more specific, as is the case for elite athletes and patients with CVD.
This review aims to analyze the CV effects of RE and current recommendations regarding the prescription of this type of exercise.
Physiological cardiovascular adaptations to resistance exerciseMuscle contraction has mechanical and metabolic properties that are involved in the various CV adaptations caused by RE. At the mechanical level, RE is traditionally subdivided into dynamic and static exercise. Dynamic RE involves concentric (shortening of muscle fibers) or eccentric (lengthening of muscle fibers) contractions, with changes in muscle length and tension, while static or isometric RE is characterized by sustained muscle contraction against a fixed load or resistance, without changes in muscle length.10 RE can be classified as anaerobic exercise at the metabolic level due to the short duration of the bouts and the regional stimulus. This means that it does not depend on the availability of oxygen (O2). Most physical activities combine these types of exercise, and are classified according to the dominant process (mechanical or metabolic).
Due to the different physiological responses to dynamic-aerobic (endurance) compared to dynamic resistance-anaerobic (strength) exercise, recommendations for exercise prescription should consider these two types of activities separately.11 In addition, different methodologies adopted in RE training sessions can activate different mechanisms and responses. Heavier loads induce more neural adaptations, moderate loads more tissue adaptations and lighter ones more metabolic adaptations.12
The type and magnitude of CV hemodynamic responses to exercise vary according to the characteristics of the exercise, being more marked in endurance exercise. Activities in which dynamic-aerobic exercise dominates are associated with a significant increase in oxygen uptake (VO2), cardiac output (CO), stroke volume (SV) and heart rate (HR), in parallel with the intensity of the activity, until a plateau at maximum effort (more evident for VO2 and SV). Systolic blood pressure (SBP) progressively increases, while diastolic blood pressure (DBP) remains steady or decreases slightly. There is also a significant decrease in peripheral vascular resistance and increased O2 extraction, widening the systemic arteriovenous O2 difference. To ensure maximal performance and to provide maximum energy for the exercising muscles, the blood is redistributed, with a shunt from metabolically less active regions, such as the renal and gastrointestinal systems, to active skeletal muscle, preserving cerebral and cardiac supply.2
By contrast, compared to aerobic exercise, CV hemodynamic responses to RE are less pronounced. During RE, changes in hemodynamic variables are directly proportional to the maximum force that can be performed, usually represented as a percentage of maximum voluntary contraction (MVC).13 Acute CV responses result in only a slight increase in peak VO2 and CO but a substantial increase in blood pressure (BP), peripheral vascular resistance, and HR. The overall effect is increased afterload, resulting in left ventricular (LV) pressure overload.14 Due to reflex vasoconstriction when intramuscular pressure exceeds intravascular pressure, even at a lower percentage of MVC, there is no significant increase in muscle blood flow with RE. SV is usually unchanged, but at high levels of tension may even decrease. For example, lifting a heavy weight can increase intrathoracic pressure leading to decreased venous return and reduced SV and CO, a typical response during the Valsalva maneuver.
The most important hemodynamic change in RE is increased BP. The less pronounced increase in CO, when associated with vasoconstriction, induces an elevation in BP that persists during the exercise. This increase is more evident for SBP, but there is also a substantial rise in DBP, a significant difference from aerobic exercise. It is important to highlight that the level of pressure overload and the subsequent changes in BP induced by RE are dependent on the magnitude of the resistance required (percentage of MVC) and the duration of muscle contraction in relation to the resting period.2
After the release of tension in strength exercise, venous return increases, increasing CO (through a constricted arterial vascular system), which results in an additional sharp rise in BP and myocardial O2 demand. During heavy RE and especially with the Valsalva maneuver, lightheadedness or dizziness may occur if CO is reduced. After relaxation, headaches may be induced while BP remains elevated.15 The Valsalva maneuver should thus be avoided in individuals with higher BP, by teaching patients appropriate breathing technique, exhaling during muscle contraction and inhaling when returning to the starting position.
Beyond the hemodynamic CV adaptations, there are also physiological adaptations related to RE at the cardiac structural level. Intensive RE characteristically increases LV wall thickness and mass, with little or no change in LV dimensions. This exercise-induced hypertrophy is typically symmetric, occurring in response to pressure overload, in contrast to the volume load found in aerobic exercise. This hypertrophy reduces the systolic burden per myofiber, thereby preserving normal LV wall stress. As most sporting disciplines combine endurance and strength exercise, physiological adaptations are the result of interconnected structural, metabolic, and hormonal mechanisms, leading to mixed phenotypes.16 Regarding cardiac function, both systolic and diastolic LV function remain normal in RE.
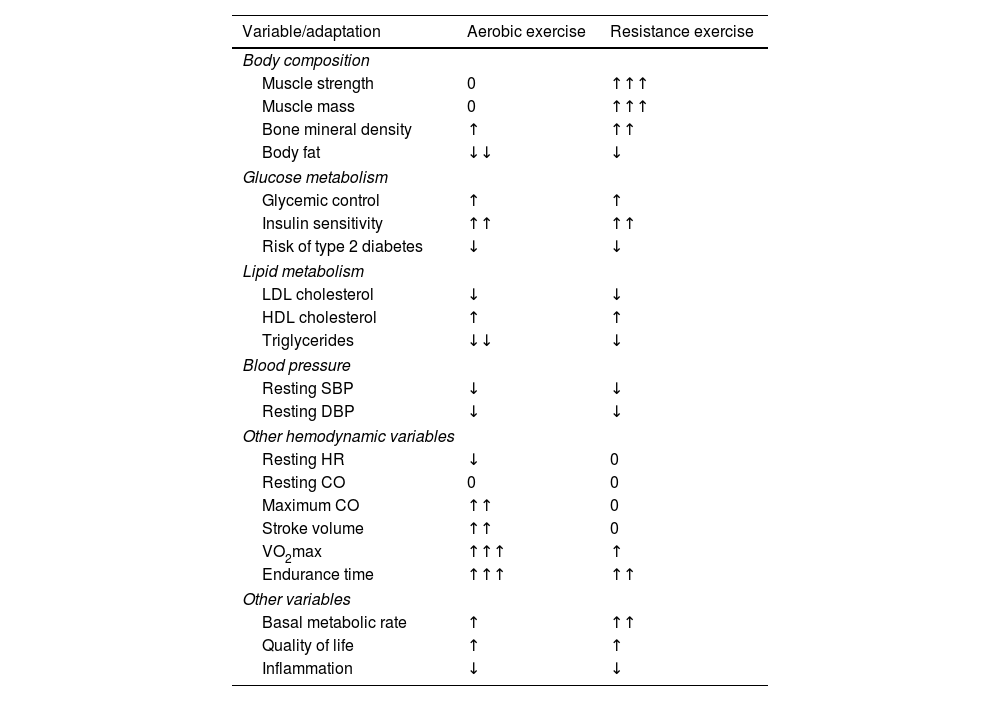
Mechanisms responsible for the cardiovascular benefits of resistance exerciseRE is associated with several benefits for CV health, especially by activating mechanisms linked to positive changes in body composition and control of various CV risk factors (Figure 1). Given the extensive evidence for the benefits of aerobic exercise training in reducing CV risk factors, RE should be seen as a complement to and not a substitute for aerobic exercise. The magnitude of the effects of RE on several variables compared to aerobic exercise is presented in Table 1.
Changes in risk factors and adaptive responses to aerobic exercise and resistance exercise training.
| Variable/adaptation | Aerobic exercise | Resistance exercise |
|---|---|---|
| Body composition | ||
| Muscle strength | 0 | ↑↑↑ |
| Muscle mass | 0 | ↑↑↑ |
| Bone mineral density | ↑ | ↑↑ |
| Body fat | ↓↓ | ↓ |
| Glucose metabolism | ||
| Glycemic control | ↑ | ↑ |
| Insulin sensitivity | ↑↑ | ↑↑ |
| Risk of type 2 diabetes | ↓ | ↓ |
| Lipid metabolism | ||
| LDL cholesterol | ↓ | ↓ |
| HDL cholesterol | ↑ | ↑ |
| Triglycerides | ↓↓ | ↓ |
| Blood pressure | ||
| Resting SBP | ↓ | ↓ |
| Resting DBP | ↓ | ↓ |
| Other hemodynamic variables | ||
| Resting HR | ↓ | 0 |
| Resting CO | 0 | 0 |
| Maximum CO | ↑↑ | 0 |
| Stroke volume | ↑↑ | 0 |
| VO2max | ↑↑↑ | ↑ |
| Endurance time | ↑↑↑ | ↑↑ |
| Other variables | ||
| Basal metabolic rate | ↑ | ↑↑ |
| Quality of life | ↑ | ↑ |
| Inflammation | ↓ | ↓ |
↑: increasing effect of the variable; ↓: a decreasing effect of the variable; 0: the variable remains unchanged; one arrow denotes small effect, two arrows moderate effect, and three arrows large effect. CO: cardiac output; DBP: diastolic blood pressure; HDL: high-density lipoprotein; HR: heart rate; LDL: low-density lipoprotein; SBP: systolic blood pressure; VO2max: peak oxygen uptake.
Changes in body composition are central to multiple benefits attributable to RE. Typically, muscle mass decreases with aging by about 8% per year in individuals between 50 and 70 years old.17 This loss of muscle mass with aging can be slowed by performing RE. Several studies have demonstrated that even relatively short sessions of regular RE can increase muscle mass, strength, power, and bone development, with a 1–3% rise in bone mineral density. These effects are the result of neuromuscular and connective tissue adaptations, induced when substantial force is placed on the bone by muscle contraction or gravity.
Although calorie expenditure during RE is less than with endurance exercise, the increase in muscle mass increases basal metabolic rate, contributing to weight control, leading to improved insulin sensitivity and enhanced sympathetic activity, mechanisms involved in the reduction of visceral and intra-abdominal fat.18
Enhancing muscle and bone strength may also contribute to preventing, slowing, or even reversing the loss of bone mass in individuals with osteoporosis, reduce pain and disability in osteoarthritis and be effective in the treatment of chronic back pain.19 Especially in physically frail elderly individuals, RE improves several components of physical function and dynamic balance, helping to reduce the incidence of falls, which are critically associated with high morbidity in this population.
These benefits in body composition also help to improve physical performance, movement control, walking speed and distance, functional independence, cognitive abilities, and self-esteem.20,21
Cardiovascular risk factorsRE has a positive role in the prevention and control of several CV risk factors, including obesity, diabetes, hypertension, and hypercholesterolemia, thereby influencing prognosis and survival free from CV events.22–24 As these factors frequently coexist and are associated with an exponentially increased risk, and share some pathophysiological mechanisms, regular exercise training has additional importance.
The beneficial effects on CV risk factors may be directly and indirectly due to various mechanisms that are attributable to RE. As discussed above, changes in body composition, particularly decreases in abdominal and visceral fat and increases in lean mass, are crucial to the control of traditional CV risk factors.25,26 A gain of 1 kg in muscle mass should increase resting energy expenditure by approximately 21 kcal/day. The effect of RE on weight management helps reduce visceral adipose tissue and increase fat-free mass, which is effective in preventing and treating a constellation of conditions leading to metabolic syndrome.
Even relatively short periods of RE can improve and activate processes involved in insulin sensitivity, endothelial function, sympathetic and neurohumoral activity, and glucose and lipid metabolism.27 Some studies suggest that low-to-moderate intensity RE may attenuate oxidative stress markers and have anti-inflammatory effects, which is important because inflammation has a central role in the pathophysiology of CVD, metabolic syndrome, and diabetes.4,28
One of the most important positive effects of RE is in the prevention of type 2 diabetes. Various mechanisms are associated with this benefit, including decreased visceral fat, reduced glycated hemoglobin (HbA1c), increased glucose transporter type 4 (GLUT4) density, increased glycogen synthase content and activity, and improved insulin sensitivity.2,4 Again, as insulin resistance is associated with abdominal fat, weight control is essential for diabetes prevention. Muscle contractions increase the expression of GLUT4, a translocator of glucose in skeletal muscle, increasing glucose uptake and glycogen synthesis, and improving insulin sensitivity in skeletal muscle, which contributes to better glycemic control.4 A meta-analysis by Strasser et al.29 showed that RE reduces visceral adipose tissue and decreases HbA1c in individuals with abnormal glucose metabolism, justifying recommendation of this type of exercise in the management of type 2 diabetes and other metabolic disorders. The benefits associated with RE were also evident in patients with type 1 diabetes, who have a higher susceptibility to complications in several physiological systems.30
Regarding BP, RE is effective in reducing resting SBP and DBP, especially in individuals with mild or moderate hypertension.23,31 Although BP reductions seem modest with this type of exercise, an SBP decrease of 3 mmHg has been associated with reductions in cardiac morbidity of 5–9%, stroke of 8–14%, and all-cause mortality of 4%.32 Compared to individuals with normal BP, those with hypertension have larger reductions following RE.33 Further benefits of RE were documented in a meta-analysis by Carlson et al.,34 which revealed that mild-to-moderate intensity isometric exercise was more effective in reducing BP in both normotensive and hypertensive individuals than aerobic training or dynamic resistance training.
The benefits of RE are also evident in lipid profile. According to the American College of Sports Medicine's position stand on exercise and physical activity for older adults, RE can increase high-density lipoprotein (HDL) cholesterol by 8–21%, decrease low-density lipoprotein cholesterol by 13–23%, and reduce triglycerides by 11–18%.35 In a study of more than 8000 men, there was a reduced risk of hypercholesterolemia among individuals participating in RE programs, especially in those training more than four hours per week.36 RE combined with aerobic exercise may be more efficacious for dyslipidemia control and reduction of the prevalence of metabolic syndrome.37
Influence of resistance exercise on cardiovascular clinical outcomesThe health benefits of enhancing muscle fitness are well documented and higher levels of muscle strength are associated with significantly better cardiometabolic risk profiles, lower risk of all-cause mortality and fewer CV events.39 RE is associated with significant clinical benefits, increasing life expectancy, and reducing major CV outcomes. Conversely, muscle weakness is a strong predictor of premature death in patients with CVD.40
In a recent meta-analysis by Saeidifard et al.41 analyzing 370256 individuals during a mean follow-up of eight years, RE alone was associated with a 21% reduction in all-cause mortality and a 40% reduction when combined with regular aerobic exercise training. In the same study, RE had a borderline association with lower CV mortality and showed no significant association with cancer mortality.
A study by Liu et al.42 analyzed 12591 individuals with a mean age of 47 years who were assessed at least twice between 1987 and 2006, with a self-report of RE training in a questionnaire. During the follow-up period, weekly RE training of 1–3 sessions or a total of 1–59 min led to a 40–70% decrease in the risk of total CV events. These benefits were independent of aerobic exercise. However, there was no significant risk reduction for RE training of more than four sessions or at least 60 min per week. Regarding CV morbidity and all-cause mortality, the results were similar.43 This study suggests that even a low frequency and amount of RE is associated with reduced risk of major CV events, independently of aerobic exercise, but apparently with a U-shaped relationship.
A recent meta-analysis of patients with coronary artery disease (CAD) showed improvement in cardiorespiratory fitness and strength with RE, to a similar degree to aerobic exercise. Lower myocardial demand, attenuation of ischemic responses, and greater subendocardial perfusion have all been observed in studies of RE compared to dynamic exercise. However, the combination of both types of exercise further increased fitness and strength.44-46 As muscle strength and cardiorespiratory fitness are independent risk factors for mortality, these results support the prescription of RE for individuals with CAD.47
In the context of post-acute coronary syndrome, exercise training should be integrated into a cardiac rehabilitation program, a multidisciplinary intervention targeting underlying risk factors, functional capacity, recovery, and psychological well-being. Cardiac rehabilitation is cost-effective, and improves quality of life and overall prognosis, leading to fewer major CV outcomes. The latest evidence emphasizes the safety and efficacy of RE in CAD patients under cardiac rehabilitation, which brings physiological adaptations additional to those from aerobic exercise alone.46 During prolonged cardiac rehabilitation (phase III programs), RE should be also implemented, with more focus on functional RE, targeting muscle groups needed to facilitate activities of daily living.47
In patients with heart failure (HF), prescription of RE has traditionally been discouraged, due to concerns about the potential negative effects of LV remodeling related to increased afterload. However, with the dose of RE that HF patients usually perform, hemodynamic responses do not exceed levels achieved during standard exercise testing, and adverse remodeling has not been shown. In this setting, the incorporation of RE in cardiac rehabilitation programs for patients with HF is safe and should be prescribed.47
Additionally, RE has other beneficial effects that indirectly influence CV health, such as improvement in mental health, reducing anxiety and depression, and in quality of sleep.48
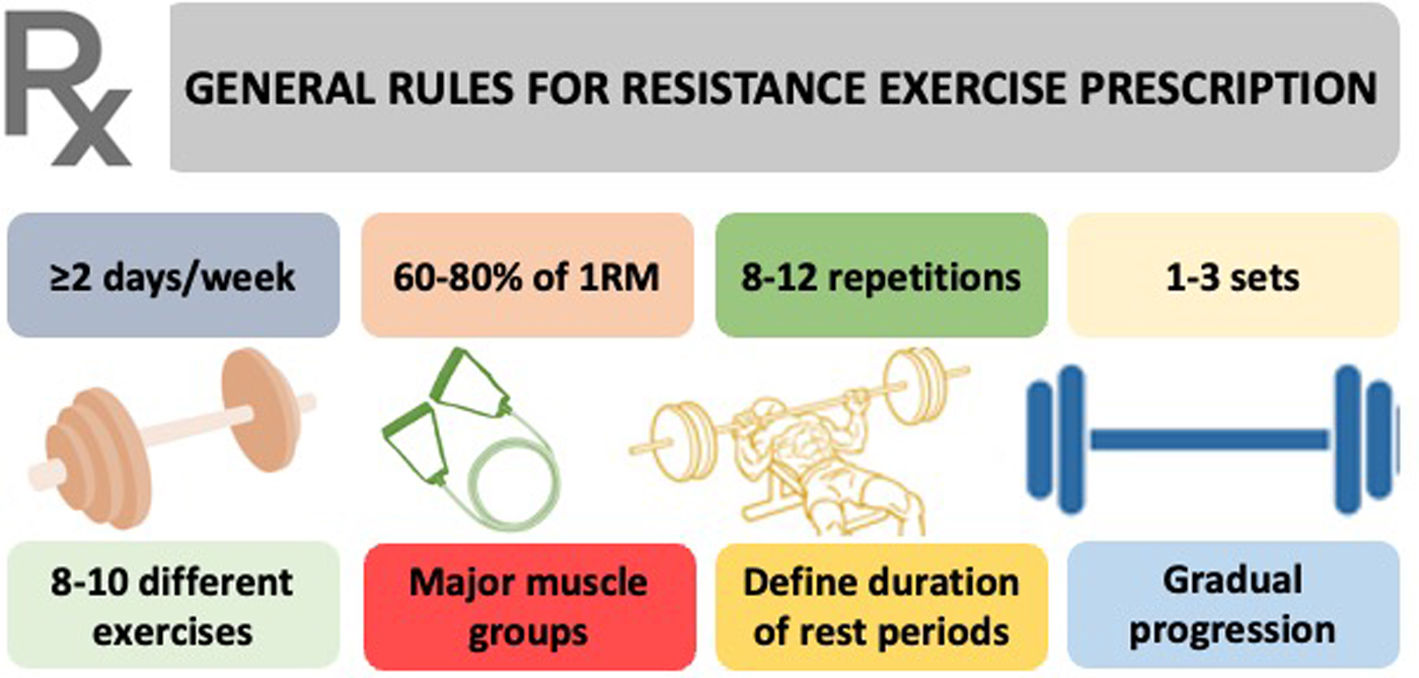
Prescription of resistance exercisePrescription of RE should be individualized, taking several variables into consideration, including the FITT principle (frequency, intensity, time spent and type), and progression of exercise. The general rules for RE prescription are summarized in Figure 2.
It is essential to determine the magnitude of the external or absolute load before prescribing RE. Regarding frequency, for previously untrained individuals, marked improvements in muscle fitness can be gained by training each muscle group as little as once per week. These rapid improvements are attributed to neural adaptations. For individuals who have progressed beyond the initial stage, the principal driver for improvements in muscle fitness is the total training volume per muscle group per week, with training frequency considered secondary in importance. For CV prevention, all the guidelines are consistent in recommending RE at least two days per week, the frequency associated with optimal strength gains.
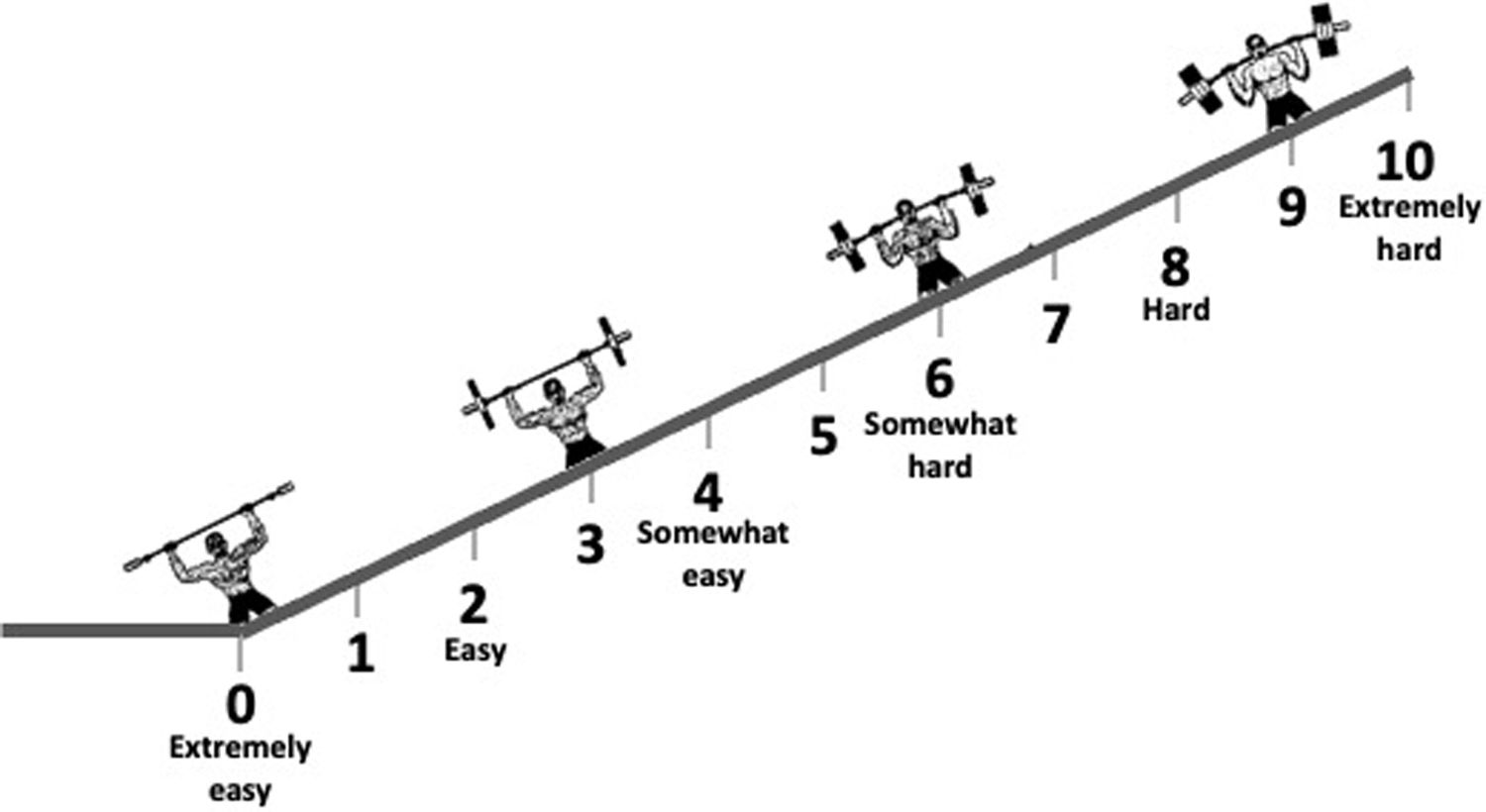
Intensity in RE corresponds to the magnitude of loading, as the amount of weight lifted. It is possible to prescribe RE using ratings of perceived exertion, as in the OMNI-Resistance Exercise Scale (Figure 3), or repetitions in reserve (RIR).12,49 With RIR, patients are advised not to train to muscle failure within each set. Instead, based on their individual characteristics, a specific repetition value or range is selected, and they are instructed to stop a certain number of repetitions short of muscle failure.
OMNI-Resistance Exercise Scale of perceived exertion.
Adapted from Robertson et al.49.
RE intensity should be selected in a shared decision-making process with the patient. The range of intensity and repetitions varies depending on the component of muscle fitness the individual wishes to develop (e.g. endurance, hypertrophy, strength, power). For example, muscle endurance is achieved by training using light loads (<50% 1RM) and higher repetition range (>15 repetitions) and slow tempo. Hypertrophy can be achieved with a range of 6–12 repetitions at moderate speed, and for muscle strength loads higher than 85% 1RM at maximum speed are recommended. Power can be improved with 1–3 sets per exercise, using light-to-moderate loading, for 3–6 repetitions (50% of 1RM), all performed aiming to move the resistance with maximum velocity. Planning the duration of rest periods between sets is also important. In general, to increase strength and power the best rest period is 2–5 min, 30–180 s for hypertrophy and 30 s or less for muscle endurance. This duration is related to the type of energy systems activated during the training sessions.12
It is possible to define training zones according to RE intensity. Moderate training intensity of 30–50% 1RM with 15–30 repetitions is considered muscle endurance training and intensities higher than 50–70% 1RM with 8–15 repetitions are optimal for strength gains.
For the general population, 1–3 sets of 8–12 repetitions are recommended at an intensity of 60–80% of the individual's 1RM. This type of exercise should include a variety of 8–10 different exercises involving each major muscle group. For older adults or deconditioned individuals, it is suggested to start with one set of 10–15 repetitions at 40–50% 1RM. In addition, older adults should perform multicomponent exercise, combining aerobic, strength and balance exercises.8 Once safety is assured, evidence is emerging that dynamic high-intensity RE should be preferred over dynamic low-intensity RE to maximize muscle mass and strength gains.47
Regarding the type of RE, a variety of equipment can be used, encompassing free weights, machines, body weight, bands or any other object requiring exertion of force against resistance. Various regimens can be also adopted, including multiple joint exercises targeting more than one muscle group, single joint exercises targeting individual muscle groups, or core exercises that engage the muscles of the trunk. RE should address concentric, eccentric, and isometric actions. To avoid muscle imbalances, opposing muscle groups should be included, such as push-ups and dumbbell rows or leg extensions and leg curls.11,50 RE can follow a station approach, in which individuals complete all the sets for a given exercise per muscle group before moving to another exercise and muscle group, or a circuit approach, with one set of each muscle group and rotation to another exercise and muscle group until the full set of exercises in completed per muscle group.
When following the principle of progressive overload, establishing an appropriate progression is very important for musculoskeletal adaptation and to reduce the risk of injury. The initial weight load should be set at a moderate level, particularly for patients with CVD, but increasing it with time will improve muscle strength and endurance. This progression and external load increase can be achieved by adjusting several variables: volume (number of sets or repetitions), intensity (amount of load lifted), and density (by changing rest periods while keeping volume and intensity unchanged).
Before starting an RE program, especially in individuals with known CV risk factors or established CVD, it is important to obtain medical clearance from physicians with experience in exercise prescription. Current scientific statements recommend avoidance of intense RE in selected patients with various CV conditions. For example, the following constitute absolute contraindications to RE: unstable CAD, decompensated HF, uncontrolled arrhythmias, severe pulmonary hypertension, severe and symptomatic aortic stenosis, uncontrolled hypertension (>180/110 mmHg), aortic dissection and Marfan syndrome.2
Resistance exercise prescription in the guidelinesBefore prescribing exercise, it is essential to perform a medical assessment, particularly in previously sedentary individuals, in the presence of already known CV risk factors or CVD, and in those aiming to start high-intensity exercise or competitive sport. The main purpose of this screening is the early identification of individuals with high CV risk or unstable medical conditions, who are at increased risk for adverse events induced by exercise training, or with conditions that may worsen with exercise. The methodology of assessment varies according to the individual's age, since the most frequent causes of sudden cardiac death differ between younger and older individuals. In young athletes, the most common causes are hereditary heart disease, especially cardiomyopathies and primary arrhythmias, while in veterans (aged over 35 years) the great majority of cases are caused by atherosclerotic CAD.
It is important to stress that a diagnosis of CVD does not mean immediate ineligibility for sport or exercise training, even at a competitive level. It means that a personalized exercise prescription, adjusted to the individual's and disease-related characteristics, is needed. For example, patients with recent myocardial infarction, coronary revascularization (percutaneous or surgical), other cardiac surgery or HF, should be included in supervised cardiac rehabilitation programs, with risk stratification, individualized exercise prescription and monitoring during training sessions.
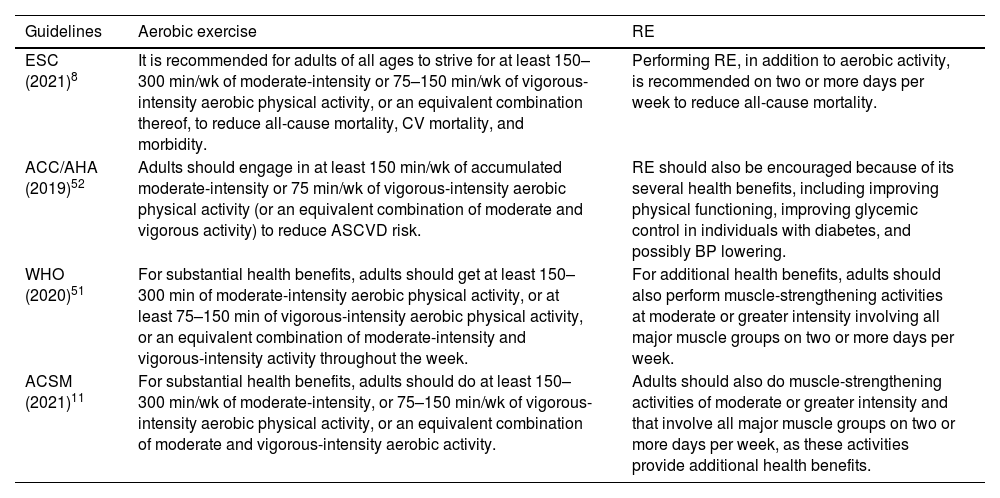
Due to the multiple benefits of the combination of RE and aerobic exercise and its positive impact in reducing total CV events and all-cause mortality, the European Society of Cardiology (ESC) guidelines recommend a combination of these two types of exercise for CV prevention.8 For adults of all ages, at least 150–300 min per week of moderate-intensity or 75–150 min per week of vigorous-intensity aerobic exercise or an equivalent combination are recommended. Adults who cannot perform 150 min of moderate-intensity exercise per week should stay as active as possible, which is essential to reduce sedentary time in daily activities.
The general population are recommended to perform RE at least two days per week, in addition to aerobic exercise.8,11,51,52 RE should be prescribed with moderate or greater intensity and involve all major muscle groups. These recommendations, for both aerobic and resistance exercise, are similar in the guidelines from several health organizations, as shown in Table 2.
Recommendations for physical activity in the general population, according to the ESC, ACSM, WHO and ACC/AHA.
| Guidelines | Aerobic exercise | RE |
|---|---|---|
| ESC (2021)8 | It is recommended for adults of all ages to strive for at least 150–300 min/wk of moderate-intensity or 75–150 min/wk of vigorous-intensity aerobic physical activity, or an equivalent combination thereof, to reduce all-cause mortality, CV mortality, and morbidity. | Performing RE, in addition to aerobic activity, is recommended on two or more days per week to reduce all-cause mortality. |
| ACC/AHA (2019)52 | Adults should engage in at least 150 min/wk of accumulated moderate-intensity or 75 min/wk of vigorous-intensity aerobic physical activity (or an equivalent combination of moderate and vigorous activity) to reduce ASCVD risk. | RE should also be encouraged because of its several health benefits, including improving physical functioning, improving glycemic control in individuals with diabetes, and possibly BP lowering. |
| WHO (2020)51 | For substantial health benefits, adults should get at least 150–300 min of moderate-intensity aerobic physical activity, or at least 75–150 min of vigorous-intensity aerobic physical activity, or an equivalent combination of moderate-intensity and vigorous-intensity activity throughout the week. | For additional health benefits, adults should also perform muscle-strengthening activities at moderate or greater intensity involving all major muscle groups on two or more days per week. |
| ACSM (2021)11 | For substantial health benefits, adults should do at least 150–300 min/wk of moderate-intensity, or 75–150 min/wk of vigorous-intensity aerobic physical activity, or an equivalent combination of moderate and vigorous-intensity aerobic activity. | Adults should also do muscle-strengthening activities of moderate or greater intensity and that involve all major muscle groups on two or more days per week, as these activities provide additional health benefits. |
ACC/AHA: American College of Cardiology/American Heart Association; ACSM: American College of Sports Medicine; ASCVD: atherosclerotic cardiovascular disease; BP: blood pressure; CV: cardiovascular; ESC: European Society of Cardiology; RE: resistance exercise; WHO: World Health Organization.
In patients diagnosed with CVD, risk stratification is essential before starting regular exercise training. Exercise prescription should take into consideration the severity of the disease, its relationship with exercise-triggered complications, and potential worsening with exercise.
The ESC guidelines on sports cardiology and exercise in patients with CVD clarify the recommendations for exercise training in the wide spectrum of CVD.53 This document contains the following points in which RE is highlighted in the context of certain clinical conditions:
- •
Obesity: RE is recommended in addition to aerobic exercise at least three times per week (class I recommendation, level of evidence A).
- •
Diabetes: RE is recommended at least three times per week to improve insulin sensitivity and achieve a better CV risk profile (class I, level A).
- •
Well-controlled hypertension: RE three or more times per week is recommended to reduce BP and CV risk (class I, level A).
- •
Well-controlled hypertension but high risk and/or target organ damage: high-intensity RE is not recommended (class III, level C).
- •
Heart failure with preserved ejection fraction: moderate endurance and dynamic RE are recommended, together with lifestyle intervention and optimal treatment of CV risk factors (class I, evidence C).
- •
Aortopathy: dynamic exercise should be considered more suitable than static exercise (class IIa, level C).
RE is associated with several benefits, notably improvement in body composition, increased strength and muscle mass, control of CV risk factors (especially diabetes, hypercholesterolemia and hypertension), and reduction of CV outcomes. There is clear evidence that these benefits are most pronounced when RE is combined with aerobic exercise. Consequently, clinical guidelines are consistent in recommending RE prescription for CV prevention, on at least two days per week, and in addition to aerobic exercise. However, RE prescription is challenging and should follow a methodological approach that considers key variables including frequency, intensity, type, time, and progression. It is time to change the current paradigm and include RE in clinical practice as an essential component to improve health, especially CV health.
Conflicts of interestThe authors have no conflicts of interest to declare.