Acute total occlusion of the unprotected left main coronary artery (LMCA) is a dramatic event. There are limited data regarding this population. We aimed to describe the clinical presentation and outcomes of patients and to determine predictors of in-hospital mortality.
MethodsThis retrospective study included patients presenting with acute (<12 h) myocardial infarction due to total occlusion of the LMCA (TIMI flow 0) between January 2008 and December 2020 in three tertiary hospitals.
ResultsDuring this period, 11036 emergent coronary angiographies were performed, 59 (0.5%) of which revealed acute total occlusion of the LMCA. Patients’ mean age was 61.2 (SD±12.2) years and 73% were male. No patients had left dominance. At presentation, 73% were in cardiogenic shock, aborted cardiac arrest occurred in 27% and 97% underwent myocardial revascularization. Primary percutaneous coronary intervention was performed in 90% of cases and angiographic success was achieved in 56% of procedures, while 7% of patients underwent surgical revascularization. In-hospital mortality was 58%. Among survivors, 92% and 67% were alive after one and five years, respectively. After multivariate analysis, only cardiogenic shock and angiographic success were independent predictors of in-hospital mortality. Use of mechanical circulatory support and presence of well-developed collateral circulation were not predictive of short-term prognosis.
ConclusionAcute total occlusion of the LMCA is associated with a dismal prognosis. Cardiogenic shock and angiographic success play a major role in predicting the prognosis of these patients. The effect of mechanical circulatory support on patient prognosis remains to be determined.
A oclusão aguda total de um tronco comum desprotegido é um evento dramático. Há poucos dados na literatura relativos a esta população. Este trabalho pretende descrever a sua apresentação e outcomes, bem como determinar preditores de mortalidade intra-hospitalar.
MétodosEste estudo retrospetivo incluiu doentes com enfarte agudo do miocárdio (<12 h de evolução) por oclusão total do tronco comum (thrombolysis in myocardial infarction=0) entre janeiro de 2008 e dezembro de 2020 em três hospitais terciários.
ResultadosDurante este período foram realizadas 11 036 coronariografias emergentes. Dessas, 59 (0,5%) revelaram oclusão aguda do tronco comum. Os doentes tinham em média 61,2 (±12,2) anos e 73% eram homens. À apresentação, 73% encontravam-se em choque cardiogénico e 27% sofreram paragem cardíaca abortada. Nenhum apresentava dominância esquerda e 97% foram submetidos a revascularização. Em 90% foi feita intervenção coronária percutânea, atingindo-se critérios de sucesso angiográfico em 56% dos procedimentos, e 7% foram submetidos a revascularização cirúrgica. A mortalidade intra-hospitalar foi de 58%. Dos sobreviventes, 92% e 67% encontravam-se vivos após um e cinco anos de follow-up, respetivamente. Após análise multivariada, apenas a presença de choque cardiogénico e sucesso angiográfico foram preditores independentes de mortalidade intra-hospitalar. A utilização de suporte circulatório mecânico e a presença de circulação colateral desenvolvida não foram preditores de morte intra-hospitalar.
ConclusãoA oclusão aguda do tronco comum associa-se a um prognóstico catastrófico. A presença de choque cardiogénico e o sucesso angiográfico são fundamentais como preditores de prognóstico a curto prazo. O efeito do suporte circulatório mecânico no seu prognóstico permanece por esclarecer.
Acute total occlusion of the unprotected left main coronary artery (LMCA) is usually a catastrophic event with a dismal presentation. Owing to the amount of affected myocardium, it often leads to abrupt severe circulatory failure, malignant arrhythmias and sudden cardiac death. As such, these patients represent a group with very high risk of mortality.
There are limited and inconsistent data regarding this population, mostly confined to small observational studies, most of which also include patients with subtotal occlusion of the LMCA.1–7 Thus, clinical management of these patients represents a particular challenge.
The objectives of our study are to describe the clinical presentation and outcomes of patients with acute total occlusion of the LMCA and to determine predictors of in-hospital mortality in these patients.
MethodsWe performed a retrospective multicenter study that identified patients with ST-elevation myocardial infarction (STEMI) or high-risk non-ST-elevation myocardial infarction who underwent emergent coronary angiography between January 2008 and December 2020 in three tertiary hospitals. Among this cohort, patients with acute total occlusion of the LMCA (thrombolysis in myocardial infarction [TIMI] flow 0) were included in the study.
We excluded patients with subacute (>12 h) presentation, subtotal LMCA occlusion, previous LMCA angioplasty, previous coronary artery bypass grafting, or iatrogenic LMCA occlusion. Patients with acute aortic or coronary dissection or infective endocarditis were also excluded.
Data on demography, clinical features and outcome were collected from all in-hospital and clinical records.
In each center an interventional cardiologist was responsible for reviewing the coronary angiograms performed in their respective center. These investigators were blinded to all other patient data.
Variables assessed included the presence of cardiogenic shock at admission, defined as the presence of sustained hypotension (systolic blood pressure <90 mmHg lasting ≥30 min) or the need for support to maintain systolic blood pressure >90 mmHg, associated with signs of end-organ hypoperfusion including cool extremities, oliguria (<30 ml/h) and altered level of consciousness.8
Coronary collateral circulation was graded according to Rentrop's classification: grade 0, no filling of the occluded vessel; grade 1, filling of the side branches; grade 2, partial filling of the epicardial vessel; or grade 3, complete filling of the epicardial vessel.9
Angiographic success was defined as residual stenosis <30% with TIMI flow 3.
The study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki as reflected in prior approval by the institution's human research committee.
Statistical analysisContinuous variables were expressed as means±standard deviation (SD) and/or medians with interquartile range (IQR) as appropriate. Discrete variables were expressed as numbers or percentages. Statistical comparisons were performed using the Student's t test or the Mann–Whitney test for continuous variables, and the chi-square test or Fisher's exact test for categorical variables, as appropriate. A p-value <0.05 was considered statistically significant.
Univariate logistic regression analysis was performed with in-hospital death as the dependent variable. Multivariate stepwise logistic regression analysis was performed in which independent variables were removed from the model if their p-value was >0.10.
All statistical analyses were performed using IBM SPSS software (version 25.0, IBM SPSS Inc., Chicago, IL).
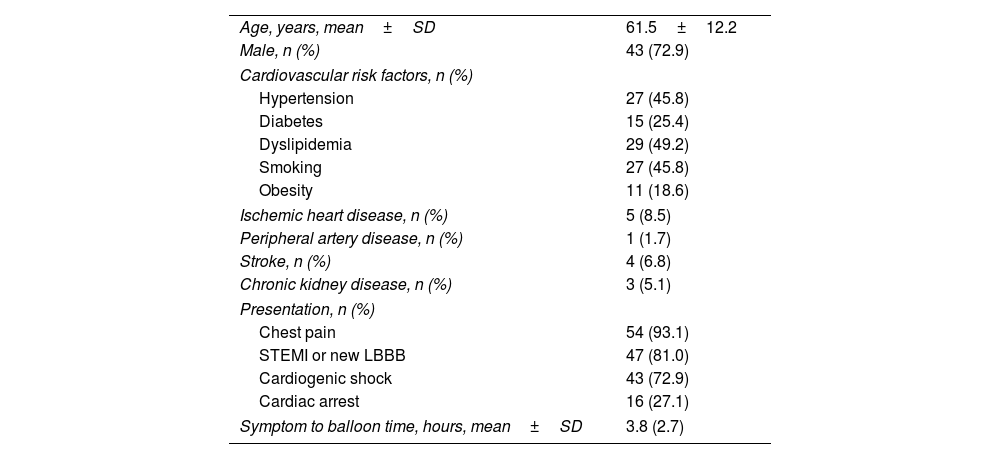
ResultsIncidence and baseline clinical dataBetween January 2008 and December 2020, 11036 patients underwent emergent coronary angiography in the three participating centers. Acute total occlusion of the LMCA was identified in 59 (0.5%) of these cases. Baseline demographic and clinical characteristics of the study population are presented in Table 1. Patients’ mean age at the time of the event was 61.2 (SD±12.2) years and 43 (73%) were male. There was a relatively low prevalence of cardiovascular risk factors, and only five (9%) had a history of ischemic heart disease. Chest pain was reported in 54 (93%) clinical presentations. At hospital admission, 47 (81%) patients had ST-segment elevation on the ECG and 43 (73%) were in cardiogenic shock. Aborted cardiac arrest occurred in 16 (27%) patients prior to catheterization (of these, 37% were out-of-hospital and 63% were in-hospital cardiac arrests).
Baseline demographic and clinical characteristics of the study population (n=59).
| Age, years, mean±SD | 61.5±12.2 |
| Male, n (%) | 43 (72.9) |
| Cardiovascular risk factors, n (%) | |
| Hypertension | 27 (45.8) |
| Diabetes | 15 (25.4) |
| Dyslipidemia | 29 (49.2) |
| Smoking | 27 (45.8) |
| Obesity | 11 (18.6) |
| Ischemic heart disease, n (%) | 5 (8.5) |
| Peripheral artery disease, n (%) | 1 (1.7) |
| Stroke, n (%) | 4 (6.8) |
| Chronic kidney disease, n (%) | 3 (5.1) |
| Presentation, n (%) | |
| Chest pain | 54 (93.1) |
| STEMI or new LBBB | 47 (81.0) |
| Cardiogenic shock | 43 (72.9) |
| Cardiac arrest | 16 (27.1) |
| Symptom to balloon time, hours, mean±SD | 3.8 (2.7) |
LBBB: left bundle branch block; SD: standard deviation; STEMI: ST-elevation myocardial infarction.
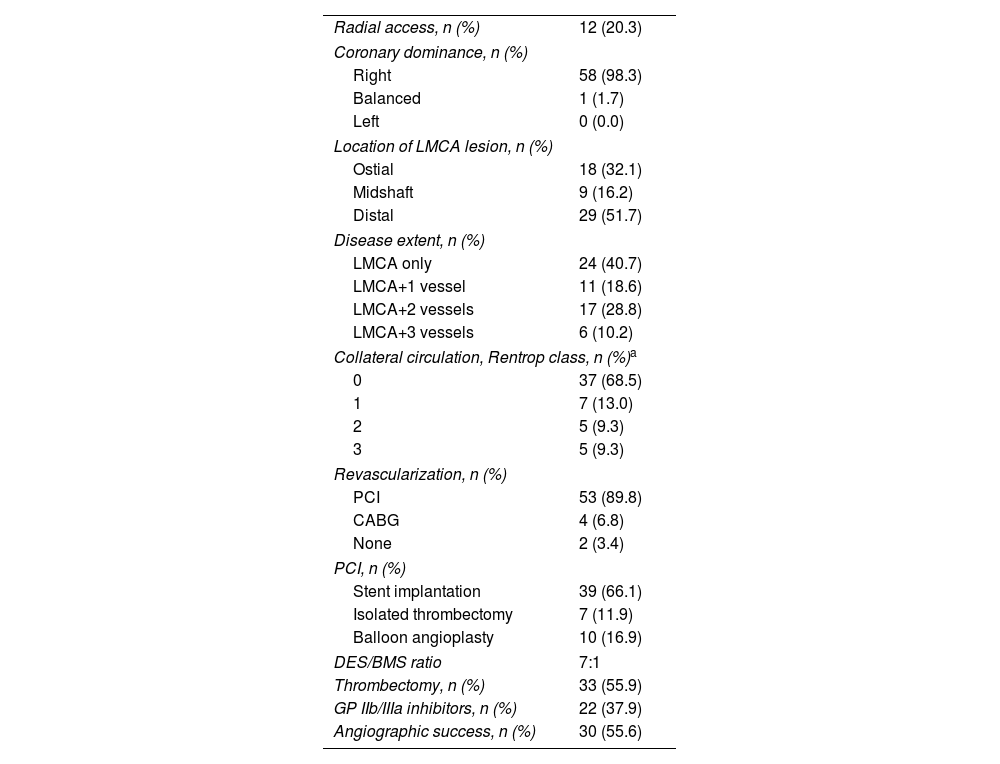
Angiographic and procedural data are presented in Table 2. A femoral approach was used in the majority of procedures. Right dominance was present in all patients except one, who had co-dominancy. Thirty-four cases (58%) had significant coronary artery disease beyond the LMCA. In 29 (52%) cases, the occlusion was located in the distal segment of the LMCA at the level of the bifurcation. Data regarding collateral circulation were available in 54 patients. Of these, 44 (82%) had a Rentrop score <2. These patients had a significantly higher prevalence of cardiogenic shock compared to patients with Rentrop score ≥2 (79.5% vs. 40.0%, p=0.02).
Angiographic and procedural data (n=59).
| Radial access, n (%) | 12 (20.3) |
| Coronary dominance, n (%) | |
| Right | 58 (98.3) |
| Balanced | 1 (1.7) |
| Left | 0 (0.0) |
| Location of LMCA lesion, n (%) | |
| Ostial | 18 (32.1) |
| Midshaft | 9 (16.2) |
| Distal | 29 (51.7) |
| Disease extent, n (%) | |
| LMCA only | 24 (40.7) |
| LMCA+1 vessel | 11 (18.6) |
| LMCA+2 vessels | 17 (28.8) |
| LMCA+3 vessels | 6 (10.2) |
| Collateral circulation, Rentrop class, n (%)a | |
| 0 | 37 (68.5) |
| 1 | 7 (13.0) |
| 2 | 5 (9.3) |
| 3 | 5 (9.3) |
| Revascularization, n (%) | |
| PCI | 53 (89.8) |
| CABG | 4 (6.8) |
| None | 2 (3.4) |
| PCI, n (%) | |
| Stent implantation | 39 (66.1) |
| Isolated thrombectomy | 7 (11.9) |
| Balloon angioplasty | 10 (16.9) |
| DES/BMS ratio | 7:1 |
| Thrombectomy, n (%) | 33 (55.9) |
| GP IIb/IIIa inhibitors, n (%) | 22 (37.9) |
| Angiographic success, n (%) | 30 (55.6) |
BMS: bare-metal stent; CABG: coronary artery bypass graft; DES: drug-eluting stent; GP: glycoprotein; LMCA: left main coronary artery; PCI: percutaneous coronary intervention; SD: standard deviation.
Fifty-seven (97%) patients underwent myocardial revascularization. Primary percutaneous coronary intervention (PCI) was performed in 53 (90%) patients. Stents were implanted in 39 (66%) of the procedures. In 34 (87%) of these, a drug-eluting stent was used. Angiographic success was achieved in 30 (56%) of the procedures. Stenting of the LMCA was not associated with a significantly higher rate of angiographic success (58.3 vs. 52.9%, p=0.71). Four (7%) patients underwent coronary artery bypass grafting (CABG).
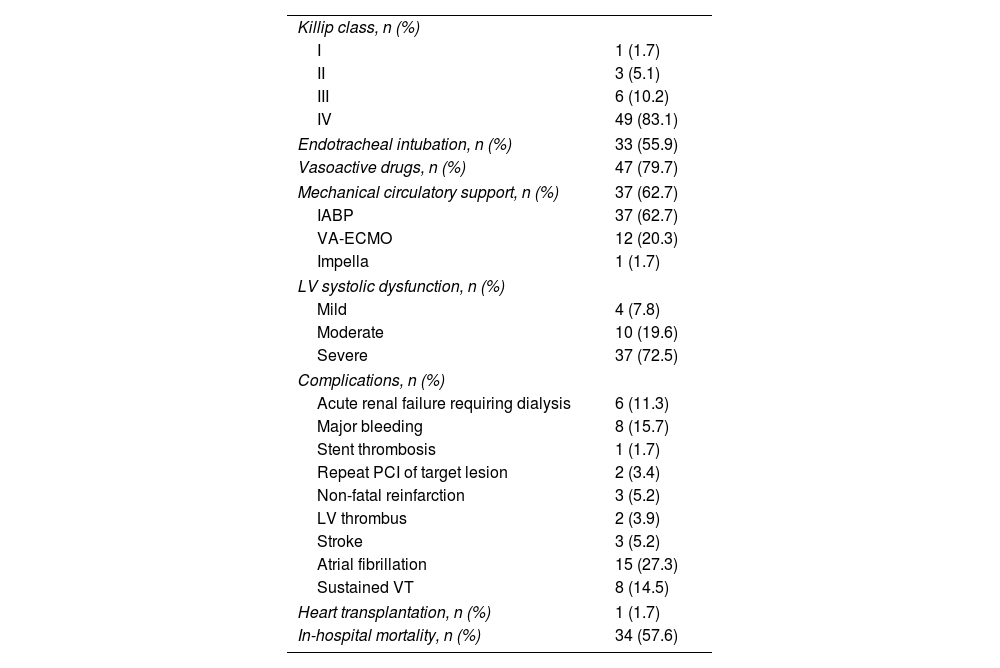
In-hospital outcomesIn-hospital outcomes are presented in Table 3. Most patients (83%) were in Killip class IV. Vasoactive support was used in 47 (80%). Mechanical circulatory support (MCS) was used in 37 (63%) of patients, in most cases an intra-aortic balloon pump. Venoarterial extracorporeal membrane oxygenation was used in 12 (20%) patients. An Impella device was implanted in one (2%) case. In 24 (41%) patients, MCS was instituted before angioplasty.
In-hospital outcomes.
| Killip class, n (%) | |
| I | 1 (1.7) |
| II | 3 (5.1) |
| III | 6 (10.2) |
| IV | 49 (83.1) |
| Endotracheal intubation, n (%) | 33 (55.9) |
| Vasoactive drugs, n (%) | 47 (79.7) |
| Mechanical circulatory support, n (%) | 37 (62.7) |
| IABP | 37 (62.7) |
| VA-ECMO | 12 (20.3) |
| Impella | 1 (1.7) |
| LV systolic dysfunction, n (%) | |
| Mild | 4 (7.8) |
| Moderate | 10 (19.6) |
| Severe | 37 (72.5) |
| Complications, n (%) | |
| Acute renal failure requiring dialysis | 6 (11.3) |
| Major bleeding | 8 (15.7) |
| Stent thrombosis | 1 (1.7) |
| Repeat PCI of target lesion | 2 (3.4) |
| Non-fatal reinfarction | 3 (5.2) |
| LV thrombus | 2 (3.9) |
| Stroke | 3 (5.2) |
| Atrial fibrillation | 15 (27.3) |
| Sustained VT | 8 (14.5) |
| Heart transplantation, n (%) | 1 (1.7) |
| In-hospital mortality, n (%) | 34 (57.6) |
IABP: intra-aortic balloon pump; LV: left ventricular; PCI: percutaneous coronary intervention; SD: standard deviation; VA-ECMO: venoarterial extracorporeal membrane oxygenation; VT: ventricular tachycardia.
Major complications during hospitalization were reported in 34 (58%) patients (Table 3). These included supraventricular and ventricular arrhythmias, major thromboembolic and bleeding events, and acute renal failure requiring dialysis. Of note, one patient developed acute stent thrombosis and required repeat angioplasty. One patient was successfully transplanted during hospitalization, but did not survive due to infectious complications.
In-hospital mortality was 58%. The majority of deaths (68%) occurred during the first day of hospitalization, and 80% within the first week. Mortality was significantly higher in patients without angiographic criteria for PCI success (87.5 vs. 36.7%, p<0.001), as well as among patients who presented with cardiogenic shock (76.7 vs. 6.3%, p<0.001) or experienced cardiac arrest in the acute phase (81.3 vs. 48.8%, p=0.03). Although not reaching statistical significance, in-hospital mortality was considerably higher among patients with STEMI (61.7 vs. 36.4%, p=0.18) or Rentrop class <2 (61.4 vs. 30.0%, p=0.09). Patients receiving MCS before PCI tended to have higher mortality (66.7 vs. 51.4%, p=0.25), but also a higher incidence of cardiogenic shock at admission (83.3 vs. 65.7%, p=0.14). Stenting of the LMCA was associated with higher in-hospital mortality (62.2 vs. 52.9%), although this was not significant (p=0.52). None of the patients undergoing CABG died during hospitalization. Patients who survived hospitalization had a median length of stay of 18 (IQR 8–50) days.
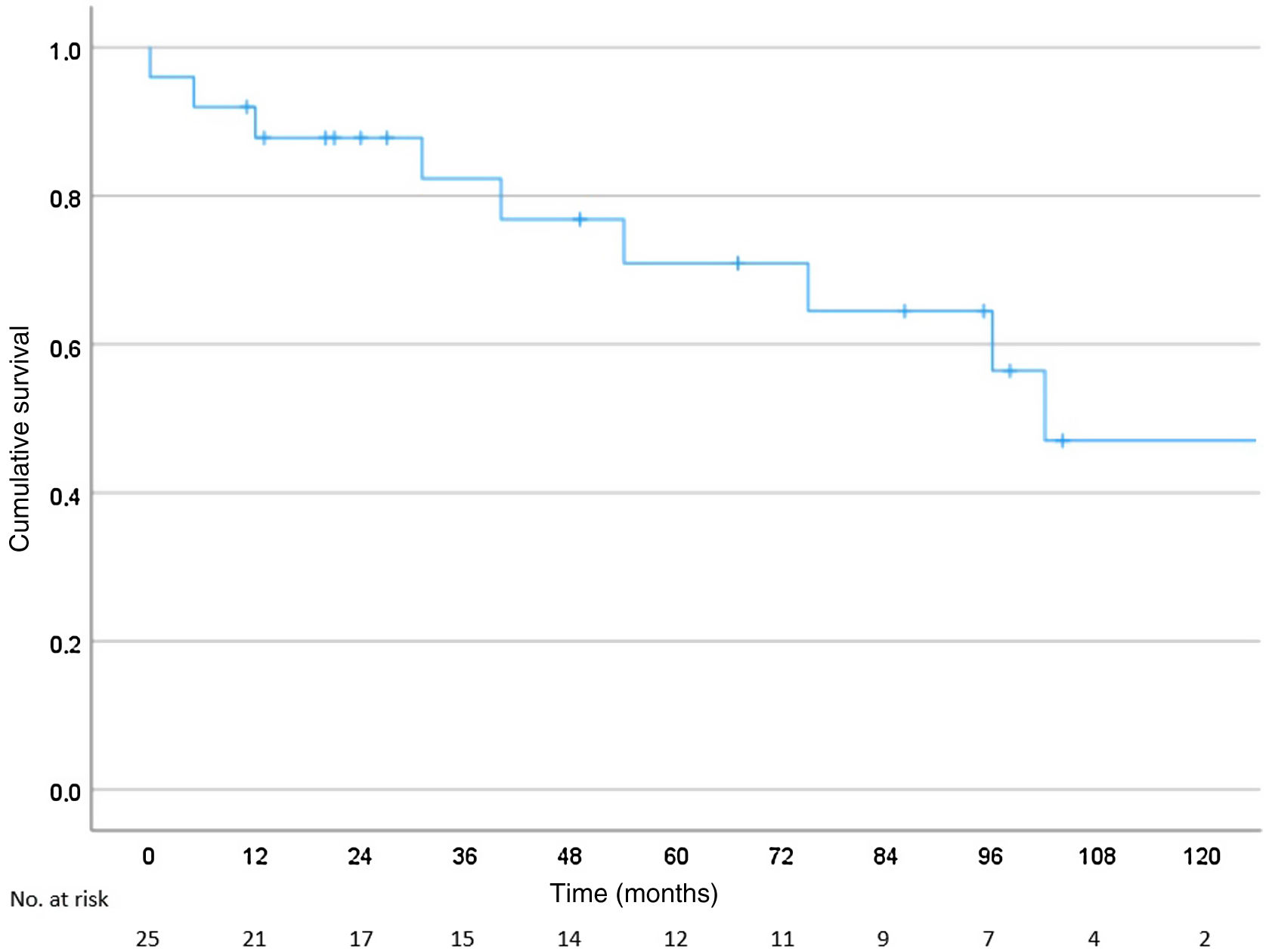
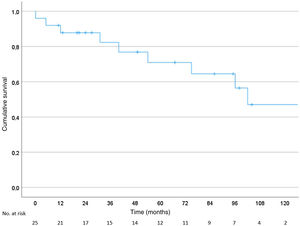
Long-term outcomesPatients surviving the index hospitalization had a median follow-up of 95 months (IQR 74–116 months). Survival rates at one and five years of follow-up were 92% and 67%, respectively (Figure 1). One patient underwent a second intervention of the LMCA three years after discharge; three patients required hospitalization because of decompensated heart failure (at one week, nine months and 2.5 years after discharge); and one patient developed advanced heart failure and underwent cardiac transplantation one year after the index event.
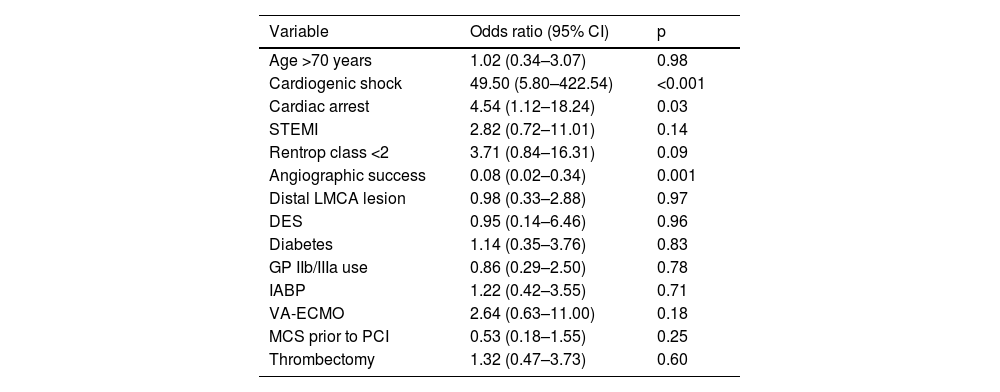
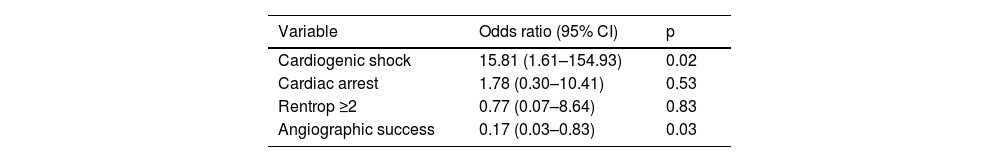
Prognostic determinantsUnivariate predictors of in-hospital mortality are presented in Table 4. Multivariate stepwise logistic regression analysis shown cardiogenic shock and angiographic success as independent predictors of in-hospital mortality (Table 5). Use of MCS and the presence of a well-developed collateral circulation were not predictors of in-hospital mortality.
Univariate predictors of in-hospital mortality.
| Variable | Odds ratio (95% CI) | p |
|---|---|---|
| Age >70 years | 1.02 (0.34–3.07) | 0.98 |
| Cardiogenic shock | 49.50 (5.80–422.54) | <0.001 |
| Cardiac arrest | 4.54 (1.12–18.24) | 0.03 |
| STEMI | 2.82 (0.72–11.01) | 0.14 |
| Rentrop class <2 | 3.71 (0.84–16.31) | 0.09 |
| Angiographic success | 0.08 (0.02–0.34) | 0.001 |
| Distal LMCA lesion | 0.98 (0.33–2.88) | 0.97 |
| DES | 0.95 (0.14–6.46) | 0.96 |
| Diabetes | 1.14 (0.35–3.76) | 0.83 |
| GP IIb/IIIa use | 0.86 (0.29–2.50) | 0.78 |
| IABP | 1.22 (0.42–3.55) | 0.71 |
| VA-ECMO | 2.64 (0.63–11.00) | 0.18 |
| MCS prior to PCI | 0.53 (0.18–1.55) | 0.25 |
| Thrombectomy | 1.32 (0.47–3.73) | 0.60 |
CI: confidence interval; DES: drug-eluting stent; GP: glycoprotein; IABP: intra-aortic balloon pump; LMCA: left main coronary artery; MCS: mechanical circulatory support; PCI: percutaneous coronary intervention; STEMI: ST-elevation myocardial infarction; VA-ECMO: venoarterial extracorporeal membrane oxygenation.
There is a paucity of data regarding patients with true acute total occlusion of the LMCA. Most of the existing literature includes patients with subocclusion or severe stenosis of the LMCA. To our knowledge, there are only two retrospective studies that exclusively included patients with true occlusion of the LMCA (TIMI flow 0).2,3
In our study, acute total occlusion of the LMCA was an uncommon event, accounting for less than 1% of acute coronary syndromes undergoing emergent coronary angiography. This is lower than reported in most studies, as patients with LMCA subocclusion or severe stenosis were often included.1,5,10–12 Although rare, this figure is likely to be underestimated, as only patients undergoing angiography were included in our study.
We observed that acute total occlusion of the LMCA occurred in a relatively young population of patients. Importantly, only a few had known ischemic heart disease, and the prevalence of known cardiovascular risk factors was relatively low. This may indicate difficulty in identifying patients at risk of suffering such dramatic events and the need to develop tools to improve individual cardiovascular risk stratification among the general population. The ominous nature of true acute LMCA occlusion makes this particularly relevant: our study showed that most patients present with cardiogenic shock and frequently suffer cardiac arrest during the acute phase of the event. A high degree of suspicion for acute total occlusion of the LMCA is needed in this clinical scenario, as prompt management may be critical for patient outcomes.
Regarding angiographic and procedural data, we observed that a significant proportion of patients with acute total LMCA occlusion did not achieve angiographic criteria of success. These results are in line with previous reports3 and are significantly worse than those reported in patients with STEMI13 and among patients who undergo elective angioplasty of the LMCA.14,15 This may be partly explained by functional and structural microvascular obstruction, which is demonstrated to occur frequently in STEMI patients despite epicardial recanalization of the culprit vessel, and may be particularly prominent in the setting of acute LMCA occlusion.16 However, evidence-based strategies targeting microvascular dysfunction are lacking.17 A randomized trial comparing the effect of deferred versus conventional immediate stenting on clinical outcomes of patients with acute occlusion of the LMCA is underway.18 This is relevant, as stenting of the LMCA was associated with a non-significant increase in in-hospital mortality in our study. As angiographic success appears to be one of the main determinants of in-hospital mortality in patients with acute total occlusion of the LMCA, every effort should be made to achieve this goal. Consistent with the reported literature, we did not observe any case with left dominance, which supports previous suggestions that this presentation may be incompatible with life.19
Our study revealed high in-hospital mortality, with most deaths occurring very early during hospitalization. This is consistent with recent2,3,12 as well as older reports.1,7,20 As in these studies, this mortality may be underestimated, as patients who died before reaching the catheterization laboratory were not included in our analysis. Despite clinical and technological advances in recent decades that have led to significant prognostic improvement in patients with STEMI,21 acute LMCA occlusion remains associated with poor prognosis. On the other hand, as in previous reports,1–4,6,19,22–24 patients surviving the index hospitalization had a favorable prognosis, with a five-year survival of nearly 70%. Hospitalizations for heart failure or subsequent acute coronary event were low.
After adjusting for confounding variables, the independent predictors of in-hospital mortality were cardiogenic shock at presentation and achievement of angiographic success. These results highlight the poor prognosis associated with cardiogenic shock, reflecting the importance of balancing aggressive hemodynamic support with the need to promptly and adequately restore coronary blood flow.
Temporary MCS devices may be important for improving patient outcomes, but the lack of randomized data creates difficulties regarding patient selection and management. In our study, the use of MCS was not a predictor of in-hospital mortality, while implantation of MCS prior to PCI was associated with a non-significant increase in in-hospital mortality. The retrospective nature of our analysis and small sample size limit conclusions regarding this issue. Overall, acute management of patients with acute occlusion of the LMCA is still a challenge that needs to be overcome.
There remains some controversy regarding the impact of early recruitment of collateral circulation on outcomes in STEMI patients.25,26 Among patients with acute total occlusion of the LMCA, data are lacking on this subject. It has long been suggested that the presence of a well-developed collateral circulation may be an important predictor of survival in this clinical scenario.7,19,27 Our study found that patients with well-developed collateral circulation (Rentrop score ≥2) had a significantly lower prevalence of cardiogenic shock at presentation, highlighting its role in these patients. However, collateral circulation was not an independent predictor of in-hospital mortality after adjustment for confounding variables. Further studies are needed in order to elucidate the role of collateral circulation in patients with acute total occlusion of the LMCA.
There was no in-hospital mortality recorded among patients who underwent CABG. These results may reflect a subgroup of patients who were more stable and able to undergo this procedure, which is generally not an option in highly unstable patients.
LimitationsThis was a small retrospective observational study susceptible to biases inherent in its non-randomized design, and lacking statistical power due to the small numbers of patients included. The long study period may have also introduced bias, as patient characteristics and outcomes may have changed over its course as a result of technological advances and improved clinical management.
ConclusionsAcute total occlusion of the LMCA is an uncommon event associated with a catastrophic presentation. Most patients present in cardiogenic shock and many suffer cardiac arrest. In-hospital mortality is high and often occurs during the first day of admission. Cardiogenic shock and achievement of angiographic success criteria play a major role in predicting the outcome of these patients. However, the latter is not achieved in almost half of procedures. There is a need to better define the role of MCS in this challenging clinical scenario.
FundingNone to declare.
Conflicts of interestThe authors have no conflicts of interest to declare.