Elective percutaneous coronary intervention (PCI) has become an increasingly safe procedure. However, same day discharge (SDD) has yet to become standard practice. Our aim is to characterize the patients who underwent elective PCI and compare outcomes between the overnight stay (ONS) patient group and the group that was discharged on the same day at 24 hours and at 30 days.
MethodsOne-year registry of patients who underwent an elective PCI. The possibility of SDD was established by the operator. Appropriate candidates were discharged at least four hours after the end of the intervention. The primary endpoints were defined as: Major adverse cardiac and cerebrovascular events (MACCE) — death, myocardial infarction (MI) stroke or transient ischemic attack (TIA), non-planned re-intervention — and vascular complications. Secondary endpoints were any unplanned hospital visit, readmission and re-catheterization.
ResultsWe performed 155 elective PCIs. One patient was admitted to the coronary care unit; 111 patients stayed overnight (ONS Group); 43 patients were discharged the same day (SDD Group). Three patients had early (<4 hours) post procedure complications: two TIAs and one vascular access site complication. There were no MACCE between four and 24 hours, nor at 30 days. At 24 hours, two patients from the SDD group had unplanned visits. Between one and 30 days, more patients from the SDD group had unplanned visits (9.3% vs. 0.9%. p=0.02). One patient from the ONS group had a recatherization. There were no readmissions or reinterventions.
ConclusionSame day discharge of selected patients who undergo elective PCIs is feasible and safe.
A intervenção coronária percutânea (ICP) eletiva tornou-se um procedimento cada vez mais seguro. No entanto, a alta no próprio dia (APD) não é uma prática de rotina. O nosso objetivo é caracterizar os doentes submetidos a ICP eletiva e comparar os resultados entre o grupo que pernoitou no hospital (PNH) e o grupo com APD, às 24 horas e aos 30 dias.
MétodosRegisto de um ano dos doentes submetidos a ICP eletiva. A possibilidade de APD foi definida pelo operador. Os candidatos apropriados tiveram alta, pelo menos quatro horas após a intervenção. Os endpoints primários foram definidos como: MACCE – morte, enfarte do miocárdio (EM), acidente vascular cerebral (AVC) ou acidente isquémico transitório (AIT), reintervenção não planeada – e complicações vasculares. Como endpoints secundários definimos: recurso não planeado ao hospital, reinternamento e recateterização.
ResultadosRealizamos 155 ICPs eletivas. Um doente foi admitido na unidade coronária; 111 doentes pernoitaram no hospital (Grupo-PNH); 43 doentes tiveram alta no próprio dia (Grupo-APD). Três doentes tiveram complicações precoces (<4 horas) pós-procedimento: dois AITs e uma complicação vascular. Não se registaram MACCE entre as 4 e as 24 horas nem aos 30 dias. Às 24 horas, dois doentes do Grupo-APD tiveram recurso não planeado ao hospital. Entre os dias 1-30, mais doentes do Grupo-APD tiveram visitas não planeadas (9,3% versus 0,9%, p=0,02). Um doente do Grupo-PNH foi recateterizado. Não houve reinternamentos nem reintervenções.
ConclusãoA alta no próprio dia, a doentes selecionados, submetidos a ICP eletiva é viável e segura.
Elective percutaneous coronary intervention (PCI) has become a widely performed procedure with a highly improved safety profile. In the 1990s, the possibility of same day discharge (SDD), in selected patients, began to be studied.1 In the subsequent decades, with rapid technical and pharmacological advancements — routine stent use,2 antiplatelet agents,3 transradial access4 — multiple studies showed that this approach, in certain cases, was both safe and preferred by patients.5,6
Furthermore, hospital resources, especially available beds, are currently scarce, and the admission of patients to the wards after an elective angioplasty increases procedure-associated costs.7 In spite of this, the strategy of SDD after non-complicated, elective PCI is far from being routine or generalized practice.8
To the best of our knowledge, this is the first report comparing the outcomes of patient between ONS or SDD strategy after elective PCI at a high-volume Portuguese center.
MethodsThis prospective, observational, single center cohort study included consecutive patients who underwent an elective (scheduled or ad-hoc) PCI over one year.
All procedure-related data were registered in a database, in accordance with a previously established protocol. This registry includes demographic, clinical and coronary anatomy data, as well as interventional procedure characteristics. Coronary interventions were performed following standard procedures at the operator's discretion.
Standard practice at our center dictates that patients are placed in a recovery room (RR) post coronary intervention, where they stay until hospital discharge. Exceptions include cases where admission to the coronary care unit (CCU) or intermediate care unit is determined by clinical or procedure-related complications. The RR is a nurse-led ward with eight beds. Physician support is provided by an interventional cardiologist or the physician responsible for the CCU. Current practice does not include post procedure electrocardiogram (ECG) or enzyme assay, unless there is clinical suspicion of complications.
We report the results of all post-PCI patients admitted to the RR, after a comparison of the clinical and procedural characteristics and outcomes of the ONS and SDD patient groups.
This study was approved by the hospital ethics committee and all patients gave informed consent.
Patient managementThe minimum defined period of in-hospital surveillance was of four hours post procedure. The possibility of SDD was determined by the operating physician based on clinical and periprocedural criteria. The protocol, approved by the interventional cardiologists, recommends ONS in the presence of the following clinical diagnoses: congestive heart failure (CHF); renal failure (serum creatinine value above 2.5 mg/dl, if known); hemodialysis patients and other cases of clear patient frailty. With regard to the characteristics of the interventional procedure, SDD was not advised in the following scenarios: left main PCI; bifurcation PCI involving double stent technique; chronic total occlusion (CTO) PCI; graft (vein or arterial) angioplasty; rotational atherectomy; glycoprotein (Gp) IIb/IIIa use of inhibitors; non-stent procedure (balloon angioplasty); very long procedures or excessive use of contrast; cases in which serious hemodynamic or electrical instability occurred. In the post procedure phase, any serious adverse event was an indication for ONS, if not for admission to the CCU or intermediate care unit. Despite these criteria, the operator was free to decide the patient's course in accordance with his or her own professional opinion and specific context. We recognize there are multiple non-protocol variables that can influence this decision (non-specified co-morbidities, fragility, particular social and family environment). When it was more comfortable for the patient, hospital stay was also offered to those whose procedure ended after 16:00 hours and would normally only leave the hospital after 20:00 hours. Patients with SDD were encouraged to get up and go on a light walk at least one hour before leaving the hospital.
Patients in the ONS group were assessed the next morning. SDD patients were contacted by telephone the next day. All patients were contacted by telephone 30 days post procedure.
EndpointsPrimary endpoints were defined by a group of major adverse cardiovascular and cerebrovascular events (MACCE) — death, myocardial infarction (MI), stroke/transient ischemic attack (TIA), urgent re-intervention — and access site vascular complication requiring additional treatment, at 24 hours and 30 days. Secondary endpoints were defined as follows: unplanned hospital consultation (emergency department or outpatient clinic), readmission and recatheterization. For events taking place in the first 24 hours, timing of occurrence/detection was also registered: intra-procedure; early post procedure (<4 hours); late post procedure (4-24 hours).
StatisticsVariables are described as number and percentage or mean ± standard deviation. Differences between groups were compared using Fisher's exact test or chi-square test, as appropriate, for categorical variables and Student's t test for continuous variables. Values of p<0.05 were considered significant. Data analysis was performed using IBM SPSS 25.0 (IBM Corp. Armonk, NY, USA).
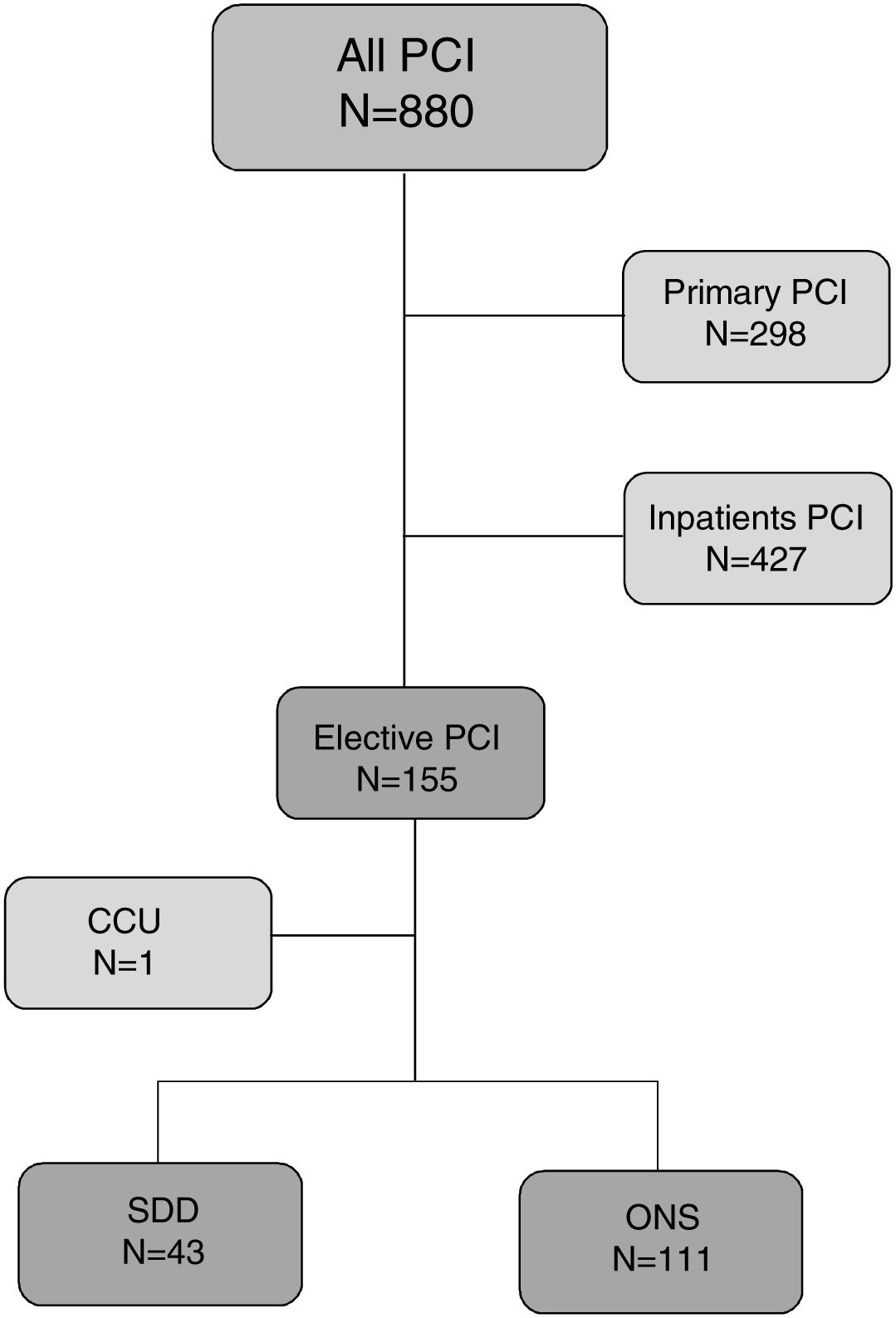
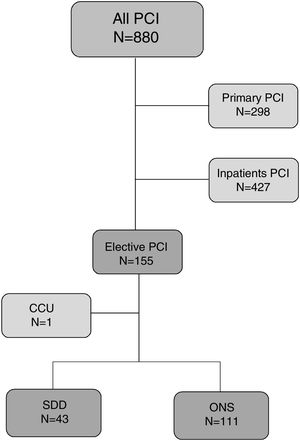
ResultsBetween 19 February 2018 and 22 February 2019, a total of 880 percutaneous coronary interventions were performed at our center. There were 298 (33.9%) primary angioplasties, 427 (48.5%) interventions to hospitalized patients and 155 (17.6%) elective PCIs. Of these 155 elective PCIs, one patient had a serious intraprocedural complication (coronary perforation and cardiac tamponade) that required immediate admission to the CCU. We analyzed 154 procedures admitted to the RR, from which 43 (27.9%) cases were discharged on the same day and 111 (72.1%) stayed overnight (Figure 1). Five patients had a repeat procedure: two for staged intervention of another vessel; three for new angioplasty attempt after an initial unsuccessful procedure (two CTO cases; one non-dilatable severely calcified lesion).
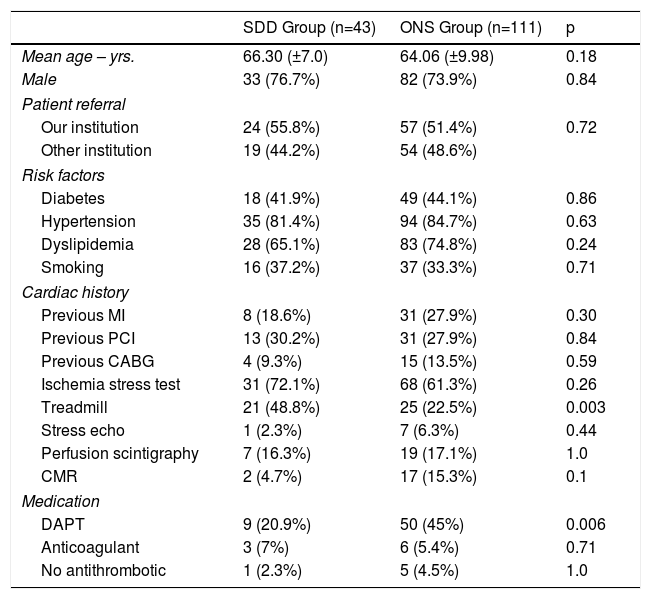
Baseline characteristics of the patients are shown in Table 1. There are no differences between groups concerning age, gender, cardiovascular risk factors and previous cardiac history. Overall there is no difference between the percentage of patients presenting with ischemia tests. However, when analyzing the treadmill stress test, this is performed more frequently in the SDD group. Double antiplatelet therapy prior to intervention is significantly more frequent in the ONS group.
Baseline characteristics.
| SDD Group (n=43) | ONS Group (n=111) | p | |
|---|---|---|---|
| Mean age – yrs. | 66.30 (±7.0) | 64.06 (±9.98) | 0.18 |
| Male | 33 (76.7%) | 82 (73.9%) | 0.84 |
| Patient referral | |||
| Our institution | 24 (55.8%) | 57 (51.4%) | 0.72 |
| Other institution | 19 (44.2%) | 54 (48.6%) | |
| Risk factors | |||
| Diabetes | 18 (41.9%) | 49 (44.1%) | 0.86 |
| Hypertension | 35 (81.4%) | 94 (84.7%) | 0.63 |
| Dyslipidemia | 28 (65.1%) | 83 (74.8%) | 0.24 |
| Smoking | 16 (37.2%) | 37 (33.3%) | 0.71 |
| Cardiac history | |||
| Previous MI | 8 (18.6%) | 31 (27.9%) | 0.30 |
| Previous PCI | 13 (30.2%) | 31 (27.9%) | 0.84 |
| Previous CABG | 4 (9.3%) | 15 (13.5%) | 0.59 |
| Ischemia stress test | 31 (72.1%) | 68 (61.3%) | 0.26 |
| Treadmill | 21 (48.8%) | 25 (22.5%) | 0.003 |
| Stress echo | 1 (2.3%) | 7 (6.3%) | 0.44 |
| Perfusion scintigraphy | 7 (16.3%) | 19 (17.1%) | 1.0 |
| CMR | 2 (4.7%) | 17 (15.3%) | 0.1 |
| Medication | |||
| DAPT | 9 (20.9%) | 50 (45%) | 0.006 |
| Anticoagulant | 3 (7%) | 6 (5.4%) | 0.71 |
| No antithrombotic | 1 (2.3%) | 5 (4.5%) | 1.0 |
CABG: coronary artery bypass graft; CMR: cardiac magnetic resonance; DAPT: double antiplatelet therapy; MI: myocardial infarction; PCI: percutaneous coronary intervention.
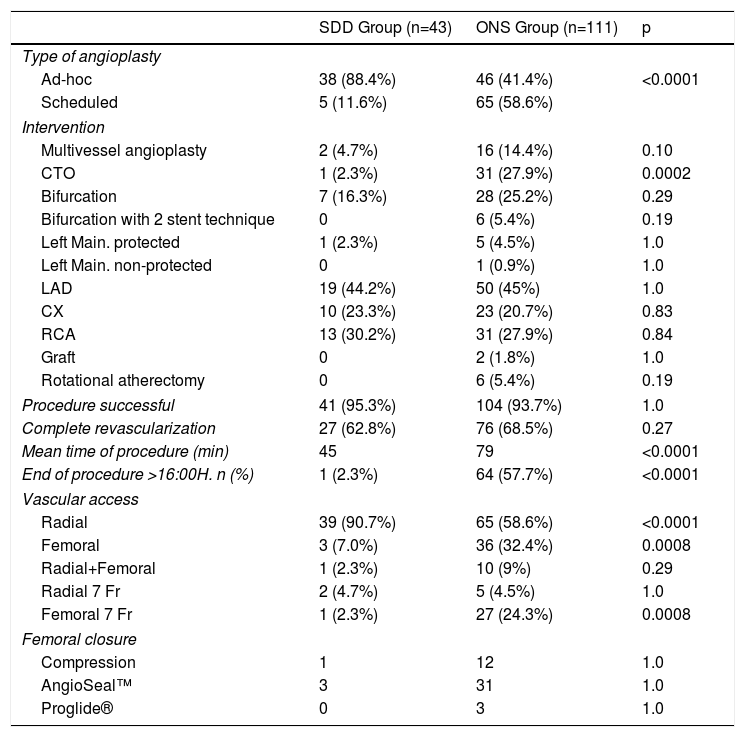
As for the characteristics of the interventional procedure (Table 2), there is a significantly greater percentage of patients in the ONS group who had a programmed angioplasty (58.6% vs. 11.6%; p<0.0001). The SDD group had 88.4% of the ad-hoc interventions. CTO intervention was also more frequent in the ONS group (27.9% vs 2.3%; p=0.0002). There are no differences in the rate of multivessel intervention or left main PCI. The success rate of the procedure is similar with 95.3% for the SDD group and 93.7% for the ONS group. The rate of complete revascularization is also similar in both groups (SDD: 62.8%; ONS: 68.5%).
Interventional procedure characteristics.
| SDD Group (n=43) | ONS Group (n=111) | p | |
|---|---|---|---|
| Type of angioplasty | |||
| Ad-hoc | 38 (88.4%) | 46 (41.4%) | <0.0001 |
| Scheduled | 5 (11.6%) | 65 (58.6%) | |
| Intervention | |||
| Multivessel angioplasty | 2 (4.7%) | 16 (14.4%) | 0.10 |
| CTO | 1 (2.3%) | 31 (27.9%) | 0.0002 |
| Bifurcation | 7 (16.3%) | 28 (25.2%) | 0.29 |
| Bifurcation with 2 stent technique | 0 | 6 (5.4%) | 0.19 |
| Left Main. protected | 1 (2.3%) | 5 (4.5%) | 1.0 |
| Left Main. non-protected | 0 | 1 (0.9%) | 1.0 |
| LAD | 19 (44.2%) | 50 (45%) | 1.0 |
| CX | 10 (23.3%) | 23 (20.7%) | 0.83 |
| RCA | 13 (30.2%) | 31 (27.9%) | 0.84 |
| Graft | 0 | 2 (1.8%) | 1.0 |
| Rotational atherectomy | 0 | 6 (5.4%) | 0.19 |
| Procedure successful | 41 (95.3%) | 104 (93.7%) | 1.0 |
| Complete revascularization | 27 (62.8%) | 76 (68.5%) | 0.27 |
| Mean time of procedure (min) | 45 | 79 | <0.0001 |
| End of procedure >16:00H. n (%) | 1 (2.3%) | 64 (57.7%) | <0.0001 |
| Vascular access | |||
| Radial | 39 (90.7%) | 65 (58.6%) | <0.0001 |
| Femoral | 3 (7.0%) | 36 (32.4%) | 0.0008 |
| Radial+Femoral | 1 (2.3%) | 10 (9%) | 0.29 |
| Radial 7 Fr | 2 (4.7%) | 5 (4.5%) | 1.0 |
| Femoral 7 Fr | 1 (2.3%) | 27 (24.3%) | 0.0008 |
| Femoral closure | |||
| Compression | 1 | 12 | 1.0 |
| AngioSeal™ | 3 | 31 | 1.0 |
| Proglide® | 0 | 3 | 1.0 |
CTO: chronic total occlusion; CX: circumflex artery; LAD: left anterior descending artery; RCA: right coronary artery.
Radial access is much more common in the SDD group (90.7% vs. 58.6%; p<0.0001). Femoral access and use of a 7 French sheath are significantly higher in the ONS group (32.4% vs. 7%; p=0.0008 and 24.3% vs. 2.3%; p=0.0008, respectively). No differences in the type of vascular closure were observed.
Procedure time is significantly longer in the ONS group (79±44 min vs. 45±18 min; p<0.0001). Furthermore, the number of patients whose procedure ended after 16:00 hours is much higher in the ONS group (64 patients, 57.7%) than in the SDD group (1 patient, 2.3%).
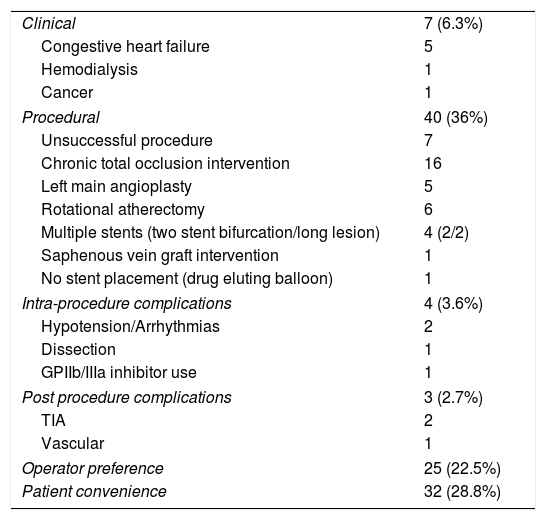
The reasons for ONS are presented in Table 3. In seven cases (6.3%) the clinical status of the patient was responsible for an ONS: five cases of CHF, one case of dialysis treatment and one case of lung cancer. Procedural causes were present in 40% of cases, particularly CTO intervention (16 cases), left main angioplasty (six cases, one of which was non-protected), use of rotational atherectomy (six cases). In seven cases the reason was an unsuccessful procedure. The following cases were also mentioned: double stent bifurcations, multiple stents in long lesions, saphenous vein graft PCI and drug eluting balloon angioplasty without stent placement. There were four cases (3.8%) with intraprocedural complications: one ventricular fibrillation, one hypotension and bradycardia requiring pharmacological intervention, one iatrogenic coronary dissection and one case of bailout use of eptifibatide. There were three cases (2.7%) of immediate post procedure complications: two patients suffered a TIA and one patient had a vascular access site complication (a large femoral hematoma following closure device failure) that required prolonged compression and a lengthened hospital stay.
Reasons for overnight stay (n=111).
| Clinical | 7 (6.3%) |
| Congestive heart failure | 5 |
| Hemodialysis | 1 |
| Cancer | 1 |
| Procedural | 40 (36%) |
| Unsuccessful procedure | 7 |
| Chronic total occlusion intervention | 16 |
| Left main angioplasty | 5 |
| Rotational atherectomy | 6 |
| Multiple stents (two stent bifurcation/long lesion) | 4 (2/2) |
| Saphenous vein graft intervention | 1 |
| No stent placement (drug eluting balloon) | 1 |
| Intra-procedure complications | 4 (3.6%) |
| Hypotension/Arrhythmias | 2 |
| Dissection | 1 |
| GPIIb/IIIa inhibitor use | 1 |
| Post procedure complications | 3 (2.7%) |
| TIA | 2 |
| Vascular | 1 |
| Operator preference | 25 (22.5%) |
| Patient convenience | 32 (28.8%) |
TIA: transient ischemic attack.
Patient convenience (28.8%) and operator preference (22.5%) combined were the main reasons for hospital stay. As for patient convenience, this is mainly caused by the late finish time of the procedure (after 16:00 hours), which meant a discharge after 20:00 hours.
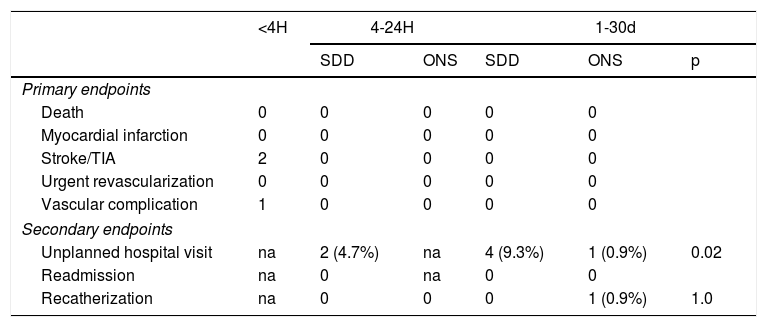
Primary and secondary endpointsOutcomes are reported in Table 4. Concerning the primary endpoint, we did not observe any events in the SDD group at 24 hours. As stated previously, there were two TIAs and one vascular complication in the ONS group. All these events occurred early post procedure, less than four hours after the end of the intervention (time frame defined as minimum for hospital observation). Between 1-30 days no events were recorded in either group. There were no reinterventions or vascular complications.
Outcomes.
| <4H | 4-24H | 1-30d | ||||
|---|---|---|---|---|---|---|
| SDD | ONS | SDD | ONS | p | ||
| Primary endpoints | ||||||
| Death | 0 | 0 | 0 | 0 | 0 | |
| Myocardial infarction | 0 | 0 | 0 | 0 | 0 | |
| Stroke/TIA | 2 | 0 | 0 | 0 | 0 | |
| Urgent revascularization | 0 | 0 | 0 | 0 | 0 | |
| Vascular complication | 1 | 0 | 0 | 0 | 0 | |
| Secondary endpoints | ||||||
| Unplanned hospital visit | na | 2 (4.7%) | na | 4 (9.3%) | 1 (0.9%) | 0.02 |
| Readmission | na | 0 | na | 0 | 0 | |
| Recatherization | na | 0 | 0 | 0 | 1 (0.9%) | 1.0 |
ONS: overnight stay; SDD: same day discharge; TIA: transient ischemic attack.
Regarding secondary endpoints, at 24 hours, unplanned hospital visits were recorded in two patients from the SDD group, one with a minor radial hematoma, the other with non-cardiovascular symptoms. Between 1-30 days, four patients from the SDD group and one patient from the ONS group attended the emergency department (9.3% vs. 0.9%; p=0.02). One patient from the ONS group had a repeat coronary angiography, showing good result from the index PCI, with a widely patent stent, without thrombosis or restenosis or disease progression in other vessels. There were no readmissions. All patients that came to the hospital were discharged the same day.
DiscussionWe intend to provide a contemporary report of elective PCI at a large volume Portuguese center. During this study, the number of serious complications recorded was low, with only four of 155 (2.6%) patients having experienced a meaningful event (one cardiac tamponade, two TIAs and one vascular complication), despite inclusion of complex PCI cases, such as CTO, left main, bifurcations and multivessel angioplasty. Only one patient was admitted to the wards (CCU). All relevant complications were intraprocedural or early after procedure, which shows that, in our experience, a four-hour observation period post-PCI is sufficient for surveillance of serious procedure-related events. This result is corroborated by other published studies6,9 that use either a four- or six-hour intervals. All 147 patients (94.8%) without immediate (<4 hours) complications had an event free course up until 24 hours.
Discharge timing after PCI has not received particular attention in society guidelines on coronary revascularization. For example, the latest European Society of Cardiology revascularization guidelines from 2018 make no mention of the length of hospital stay after elective PCI. The only document addressing this issue is an expert consensus document published in 2009 by the Society of Cardiovascular Angiography and Interventions (SCAI).10 In this document, SDD is only recommended in very restricted circumstances — no comorbidities, under 70 years of age, normal left ventricular function, single vessel disease, single vessel PCI, single stent use less than 28 mm in length. Our protocol did not follow these recommendations as we felt they did not reflect current practice. We accepted a much larger variety of clinical, anatomical and procedural characteristics, leaving the final decision to the operator responsible for the procedure.
Two metanalyses11,12 gathered information from multiple observational and randomized studies, showing equivalence between SDD and ONS strategies. Despite this evidence, SDD is not widespread practice and its acceptance is widely variable among interventional cardiologists.13 Nevertheless, when used continuously, the results are positive and SDD can be applied safely, as shown recently in a study by Rubimbura et al. reporting over ten years of experience.14
Our initial experience shows that the general approach to patient guidance after the procedure was quite conservative. Many patients, with no clinical or procedural criteria (as per approved protocol) excluding SDD, stayed overnight because of operator preference or personal convenience. Nevertheless, we must recognize that the ONS group had more complex procedures, as indicated by significantly more CTO cases and significantly superior procedure duration. Also, it is noteworthy that more than half of the patients (57.7%) of the ONS group finished their procedure after 16:00 hours. This is in most part related to operators scheduling their PCI cases for the afternoon. We believe that if the department schedule allowed for an earlier start in these cases, a much larger number of patients could be discharged on the same day. It is also worth noting that the preferential use of radial access allows the adoption of the “cardioLounge” or “radiallounge”15 concept for the short stay of these patients, with evident gains in usage of space and patient comfort.
Although the majority of cases were performed transradially (67.5%), our series shows that femoral access does not preclude SDD, especially when vascular closure devices are used successfully. We had only one femoral complication, despite this route being associated with more complex cases. This is similar to published data demonstrating that the access site (radial or femoral) does not influence the safety of SDD.16,17
The few patients that had unplanned hospital visits did not present with any serious procedure-related event. Most cases were non-procedure-related; others were easily managed with patient reassurance.
Patient education by health care providers is crucial for the success of the SDD strategy. A careful and detailed explanation of the procedure follow-up and the clear identification of symptoms and signs to monitor, is of paramount importance to patient adherence and can prevent unnecessary hospital visits.
Study limitationsThis is a non-randomized, observational single center study comprising data from only one year of practice. Operators were free to make independent decisions and we cannot exclude wide variation in strategy among interventional cardiologists.
Nonetheless, this study provides a real-life picture of a large volume Portuguese center and reports the initial experience of a structured program of SDD for non-complicated elective PCI patients. The challenge now facing us into the future is to ensure these cases are managed safely as outpatients, improving hospital results and patient satisfaction.
ConclusionThis study shows that the application of a SDD strategy on selected patients, after non-complicated elective PCI, is viable and safe. A four-hour post procedure period of surveillance seems to be sufficient to exclude serious complications.
Cardiology departments and hospital management should evolve by considering allocated space, resources and job planning to maximize this strategy.
Conflicts of interestThe authors have no conflicts of interest to declare.