Percutaneous coronary intervention (PCI) of heavily calcified lesions is a challenge for the interventional cardiologist and is associated with a high rate of restenosis and target lesion revascularization (TLR). Adequate lesion preparation by rotational atherectomy followed by drug-eluting stent implantation has shown favorable results.
ObjectiveTo report the recent experience of our center with rotational atherectomy (RA) of complex and heavily calcified coronary lesions.
MethodsWe retrospectively analyzed consecutive patients who underwent PCI with RA in our center between January 2009 and December 2010. A total of 42 patients were included, 65% of whom had been previously refused for coronary artery bypass grafting due to unfavorable coronary anatomy or high surgical risk. RA was performed using the standard Boston Scientific Rotablator® system. The procedure was performed ad-hoc in 50% of patients and transradial access was used in 35%. Data were collected on immediate post-procedural events and major cardiac events during follow-up – cardiovascular death, myocardial infarction, TLR and recurrent angina.
ResultsOf 1650 PCIs performed in a 23-month period from January 2009, 42 (2.5%) involved RA; from a total of 42 patients (mean age 70.3±10.1 years, 67% male, 55% diabetic), three had left main disease, six had three-vessel disease, 18 had two-vessel disease and the other 15 had single-vessel disease. Of the lesions treated, 71% were >20mm long and classified in 69% of cases as type C according to the ACC/AHA lesion classification, 4% being chronic total occlusions. The left anterior descending artery was treated in 56% of the procedures. The mean number of burrs used per lesion was 1.3 and a total of 69 stents were implanted, 81% of which were drug-eluting. During follow-up three patients had recurrent angina, one required TLR and two died due to a cardiovascular event. There was significant clinical improvement in 83% of patients.
ConclusionsThis study demonstrates that rotational atherectomy followed by stenting in heavily calcified lesions can nowadays be performed with high success rates and few complications, extending the possibility of coronary revascularization to a greater number of patients.
A intervenção coronária percutânea (ICP) de lesões gravemente calcificadas constitui um desafio para o cardiologista de intervenção, estando associada a maior taxa de reestenose e necessidade de reintervenção na lesão alvo. A preparação adequada das lesões pela técnica de aterectomia rotacional (AR), seguida da colocação de stent farmacoactivo, tem demonstrado resultados favoráveis.
ObjectivoReportar a experiência recente do nosso centro na utilização de AR para o tratamento de lesões coronárias complexas e calcificadas.
Material e MétodosAnalisámos retrospectivamente uma série de doentes consecutivos submetidos a ICP com recurso a AR no período de Janeiro de 2009 a Dezembro de 2010. Foram incluídos 42 doentes (dts), dos quais 65% tinham sido recusados para cirurgia por apresentarem múltiplas comorbilidades ou anatomia coronária desfavorável. A AR foi realizada utilizando o sistema Rotablator® da Boston Scientific. O procedimento foi realizado ad-hoc em 50% dos casos e utilizou-se a via radial em 35% dos dts. Foi avaliada a ocorrência de eventos no pós procedimento imediato e realizado follow-up (FUP) com avaliação de eventos cardiovasculares major após a alta hospitalar – morte cardiovascular (MCV), enfarte agudo do miocárdio, reintervenção na lesão alvo (RLA) e recorrência de angina (RA).
ResultadosDe um total de 1650 ICP realizadas durante um período de 23 meses desde Janeiro de 2009, 42 (2,5%) envolveram a técnica de AR. Num total de 42 doentes submetidos a AR (70,3±10,1 anos, 67% homens, 55% de diabéticos), três apresentavam doença (DC) de tronco comum (TC), seis dts DC de 3 vasos, 18 dts DC de 2 vasos e 15 dts DC de 1 vaso. As lesões tratadas (71%>20mm) classificaram-se como tipo C em 69% e oclusão total crónica em 4%. Intervencionou-se a descendente anterior em 56% dos casos. Utilizou-se uma média de 1,3 olivas por lesão e implantaram-se no total 69 stents, 81% dos quais eram farmacoactivos. Verificou-se RA em três dts, RLA em apenas um dt e MCV em dois dts. Em 83% dos doentes verificou-se melhoria da classe funcional.
ConclusãoA utilização da AR na ICP de lesões gravemente calcificadas, seguida de colocação de stent, é um procedimento seguro e com uma elevada taxa de sucesso, permitindo a revascularização coronária a um maior número de doentes.
Percutaneous coronary intervention (PCI) of heavily calcified lesions is a challenge for the interventional cardiologist and is associated with a high rate of restenosis and target lesion revascularization (TLR). Significant calcification and atherosclerotic plaque morphology often make crossing the lesion by balloon or stent difficult1 due to reduced vascular wall distensibility, which can lead to coronary dissection, poor expansion or incomplete stent apposition after angioplasty.2,3 Adequate lesion preparation by rotational atherectomy (RA) to modify heavily calcified plaques and thus facilitate stent placement and appropriate expansion has shown favorable results.4,5 Bare-metal stent implantation following RA of calcified lesions has high rates of immediate success but is associated with significant restenosis.6 However, recent studies have demonstrated that use of drug-eluting stents after RA significantly reduces restenosis and need for TLR.7
The aim of this study is to report the recent experience of our center with RA of calcified coronary lesions and preferential use of drug-eluting stents.
MethodsWe retrospectively analyzed consecutive patients with symptomatic coronary disease who underwent PCI with RA of heavily calcified and angiographically significant lesions (≥50% stenosis) between January 2009 and December 2010. The decision to perform RA prior to angioplasty was based on the presence of severe calcification on fluoroscopy, with a view to avoiding any difficulties in crossing the lesion and achieving adequate balloon predilation.
Intravascular ultrasound (IVUS) was used whenever disease severity permitted, to clarify the degree of calcification and extent of lesions, vessel caliber, location of calcification (superficial and/or deep), and involvement of bifurcations or ostia, as well as to assess the final result (confirmation of correct stent expansion and apposition).
The choice of vascular access (radial or femoral artery) depended on whether problems were encountered with cannulation or catheter support during diagnostic catheterization, as well as the possible need for devices and techniques that required larger caliber introducers. Thus, a femoral approach was preferred if the use of >1.5mm burrs was anticipated as these require introducers of ≥7F, and radial access was chosen for ≤1.5mm burrs, with 6F introducers.
All patients were medicated with aspirin (100–150mg/day) and clopidogrel (loading dose 300mg followed by 75mg/day), together with unfractionated heparin (70U/kg) during the procedure. A continuous perfusion of saline with verapamil, nitrates and heparin was administered through the coronary system to prevent thrombus formation and coronary spasm leading to no reflow.
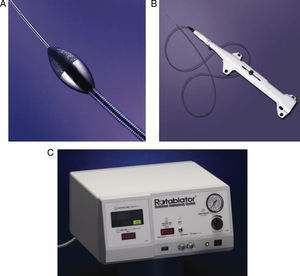
RA was performed using a Boston Scientific Rotablator® system, which includes a 0.009-in. RotaWire guide wire, a RotaLink advancer and a console, compressed air supply and Dynaglide foot pedal (Figure 1).
Facilitated expansion was used, in which the smallest possible caliber burr is used to modify the plaque surface and allow adequate balloon expansion prior to stent placement. The burr was introduced via a catheter using Dynaglide to prevent friction and placed immediately proximal to the stenosis to avoid damaging the normal segment of the vessel. Plaque ablation was performed using a “pecking” technique at a mean rotational speed of 140 000rpm. Each application was of 15–20s, and was interrupted immediately if a reduction of more than 5000rpm was observed (reflecting increased resistance and overheating of the vessel). Lesion preparation was followed by balloon predilation (at low pressure to avoid dissection) and stent implantation. While preference was given to drug-eluting stents, bare-metal stents were used if there were contraindications to prolonged dual antiplatelet therapy. The procedure was deemed successful when stent placement in the lesion was achieved with angiographic confirmation of <20% residual stenosis and TIMI 3 flow.
We analyzed procedure time, duration of hospital stay, and major cardiovascular events – myocardial infarction (defined as troponin I elevation of >3 times baseline value), cardiovascular death, TLR or stroke – before discharge. Patients were followed up by telephone or in routine consultations, and data collected on cardiovascular death, myocardial infarction, TLR and recurrent angina.
ResultsOf 1650 PCIs performed in a 23-month period from January 2009, 42 (2.5%) included RA. The clinical and demographic characteristics of the study population are shown in Table 1. Mean age was 70.3±10.1 years, 28 patients were male (67%) and 23 were diabetic (55%); 65% had been previously refused for coronary artery bypass grafting due to unfavorable coronary anatomy or high surgical risk.
Clinical characteristics.
| n | % | |
| Total number of patients | 42 | |
| Mean age (years) | 70.3±10.1 | |
| Male | 28 | 67 |
| Diabetes | 23 | 55 |
| Hypertension | 36 | 86 |
| Dyslipidemia | 26 | 62 |
| Current smoker | 4 | 9.5 |
| Ex-smoker | 6 | 14 |
| Renal failure | 9 | 21 |
| Previous infarction | 20 | 48 |
| Previous PCI | 11 | 26 |
| Previous CABG | 3 | 7 |
| Clinical presentation | ||
| Stable angina | 27 | 64 |
| Unstable angina | 5 | 12 |
| NSTEMI | 8 | 19 |
| STEMI | 2 | 5 |
CABG: coronary artery bypass grafting; NSTEMI: non-ST elevation myocardial infarction; PCI: percutaneous coronary intervention; STEMI: ST-elevation myocardial infarction.
Coronary angioplasty was elective in 50% of cases, and performed ad hoc following diagnostic coronary angiography in the remainder.
Access was exclusively femoral in 23 patients (55%) and radial in 15 (35%), with crossover from radial to femoral in four patients (10%). Angiographic characteristics are shown in Table 2. A total of 45 vessels were treated by RA, including the anterior descending artery in 25 patients (56%), the right coronary artery in 11 (24%) and the circumflex in 6 (13%). Angioplasty was concomitantly performed on the left main artery in three cases (7%), one of which was protected. Most lesions (71%) were >20mm long, and 88% were classified as type B2 or C. IVUS was used to characterize lesions in 35% of cases (15 patients), and confirmed the need for RA in all cases to remove heavy calcification of atherosclerotic plaques.
Pre-intervention angiographic characteristics.
| n | % | |
| Coronary disease | ||
| Single-vessel | 15 | 36 |
| Two-vessel | 18 | 43 |
| Three-vessel | 6 | 14 |
| Left main | 3 | 7 |
| Treated vessel | ||
| Anterior descending | 25 | 56 |
| Circumflex | 6 | 13 |
| Right coronary | 11 | 24 |
| Left main | 3 | 7 |
| Ostial lesion | 9 | 20 |
| Bifurcation | 8 | 18 |
| Chronic total occlusion | 2 | 4 |
| Classification of lesionsa | ||
| Type B1 | 5 | 12% |
| Type B2 | 8 | 19% |
| Type C | 29 | 69% |
Procedure characteristics are shown in Table 3. A single burr was used in 32 vessels (76%), while two were used in eight vessels (19%) and three in two vessels (5%). The most commonly used single burr was 1.25mm (62%); mean burr size was 1.43mm and mean burr-to-vessel ratio was 0.46. A total of 69 stents were implanted, 81% of which were drug-eluting.
Procedure characteristics.
| n | % | |
| Rotational atherectomy | ||
| No. of burrs per vessel (mean) | 1.26±0.49 | |
| Mean burr size (mm) | 1.43±0.24 | |
| Minimum burr size (mm) | 1.25 | |
| Maximum burr size (mm) | 2 | |
| Burr-to-vessel ratio | 0.46 | |
| Stent | ||
| Total stents implanted | 69 | |
| Drug-eluting stents | 56 | 81 |
| No. of stents per vessel (mean) | 1.76±0.82 | |
| Stent diameter, mm (mean) | 3.07±0.46 | |
| Total stent length, mm (mean) | 35.4±17.6 | |
| Use of Gp IIb/IIIa inhibitors | 3 | 7 |
| Angiographic success | 100 | |
Gp IIb/IIIa: glycoprotein IIb/IIIa receptor.
Complete revascularization was achieved in 17 patients (40%). There were no significant periprocedural complications, apart from one case of no reflow that responded immediately to intracoronary administration of adenosine and verapamil. Angiographic success was achieved in all procedures, and no major events occurred before discharge. Mean procedure time was 110.2±30min, with no differences between elective and ad hoc interventions. Mean hospital stay was 1.8±0.3 days.
Follow-up (mean 9±5 months) was achieved in 37 patients (88%); the other five were resident abroad and could not be contacted. Two patients died of cardiovascular cause approximately one year after the intervention. One patient underwent successful TLR eleven months after implantation of two drug-eluting stents in the right coronary artery, by drug-eluting balloon angioplasty of the restenosis. Three patients had recurrence of angina (CCS class II) between 12 and 20 months after the procedure, but there was no evidence of disease progression or stent restenosis on repeat coronary angiography, so medical therapy was intensified. One patient, with diffuse distal atheromatosis of several vessels, reported unchanged functional class despite PCI. In the remaining patients (83%), there was significant improvement in functional class (CCS class 0-I). No patient was rehospitalized for myocardial infarction.
DiscussionPercutaneous treatment of heavily calcified coronary lesions presents technical difficulties that can significantly affect the final outcome of the procedure. Incomplete dilation of fibrocalcific stenotic lesions (reducing acute luminal gain) and repeated high-pressure balloon inflations increase the risk of restenosis and dissection or perforation of the vessel wall.8
IVUS can play an important role in accurate characterization of atherosclerotic plaques, by determining the degree of calcification and in particular its location. Lesions with superficial calcium respond more favorably to rotational atherectomy than to balloon dilation by itself.9,10
Various devices and techniques have been developed over the years to overcome the technical difficulties involved in coronary calcification, including RA. This technique uses a diamond-coated burr that rotates at high speed to abrade part of the fibrocalcific atherosclerotic plaque, leaving a smooth surface denuded of endothelium but preserving the media intact.11
Besides calcified lesions, RA has also been shown to be effective in other situations, including: (1) aorto and non-aorto ostial lesions, increasing success rates and reducing restenosis compared to stent implantation alone12–15; (2) chronic total occlusions, facilitating stent placement and also reducing restenosis16,17; (3) diffuse disease involving several bifurcations, significantly reducing loss of secondary vessels18,19; and (4) stent underexpansion despite high inflation pressure, through ablation of the stent-calcium complex, thus enabling implantation of a new stent.20
Successful RA thus improves arterial compliance and creates a passage for the balloon and stent.21 Using this technique prior to stent implantation effectively reduces the size of the atherosclerotic plaque and its axial distribution, thus decreasing the risk of restenosis and occlusion of collateral vessels in bifurcations.
In the pre-stent era, although RA facilitated balloon placement at the lesion site, the technique was associated with a high rate of restenosis and TLR, which reached 40% in some series.22 Balloon angioplasty combined with bare-metal stent implantation following RA reduced restenosis and TLR rates, but these still remained at around 20%.
The introduction of drug-eluting stents has led to more significant reductions in restenosis and TLR in both calcified and non-calcified lesions.23 Nevertheless, stent implantation in cases of complex coronary anatomy, particularly heavily calcified eccentric lesions, can be difficult and may be associated with significant complications, such as stent thrombosis or polymer degradation affecting drug release. Adequate lesion preparation prior to drug-eluting stent implantation is therefore essential to ensure correct stent expansion and reduce late complications. Several studies have demonstrated the efficacy of combining RA with drug-eluting stent implantation in the treatment of heavily calcified lesions.24,25 In a series by Rathore et al., this combination reduced restenosis and TLR by more than 50% compared to RA with bare-metal stents.7
The resurgence of RA in the drug-eluting stent era reflects the difficulties arising from the fact that older patients with more complex and calcified lesions are being treated. The high percentages of patients in our study population with diabetes, renal failure and multivessel disease, and who had been refused for coronary artery bypass grafting, highlight the importance of this technique in extending indications for revascularization. Although complete revascularization was not achieved in most cases, there was clear improvement in symptoms and quality of life, with low rates of periprocedural complications and major events during follow-up.
Use of radial access in a significant number of procedures resulted in shorter hospital stay and earlier ambulation. It was however necessary to cross over from radial to femoral access in four patients, since the caliber of the vessels involved (>3mm) required 1.75–2.00mm burrs and hence 7F introducers.
Although this was a retrospective study of a small patient sample, it should be noted that procedure times were similar for elective and ad hoc procedures. Rapid access to all the necessary material and a highly motivated team enable this type of complex intervention to be integrated easily into the daily activities of an interventional cardiology laboratory.
ConclusionsRotational atherectomy of heavily calcified coronary lesions, followed by drug-eluting stent implantation, presents a low rate of complications and favorable long-term results. RA can be used for ad hoc revascularization, with radial access, for almost all types of coronary anatomy, although specific training is essential for the whole catheterization laboratory team, and experience is a determining factor in minimizing complications.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Seca, L. O ressurgimento da aterectomia rotacional na era dos stents farmacoactivos – A experiência de um centro. doi:10.1016/j.repc.2011.09.015.