Nebivolol is a novel beta1-selective beta-blocker with vasodilator properties mediated through activation of the l-arginine–nitric oxide pathway. There is no published report of coronary artery spasm associated with nebivolol. We describe a 64-year-old female patient who developed unstable angina secondary to nebivolol-induced vasospastic angina which was also visible during coronary angiography.
O nebivolol é um novo beta-bloqueante β1-seletivo com propriedades vasodilatadoras mediadas pela ativação da via L-arginina/óxido nítrico. Não existem publicações relatando um espasmo das artérias coronárias associado ao nebivolol. Descrevemos o caso de uma doente com 64 anos de idade que desenvolveu angina instável por espasmo induzido pelo nebivolol que foi igualmente documentado durante a angiografia coronária.
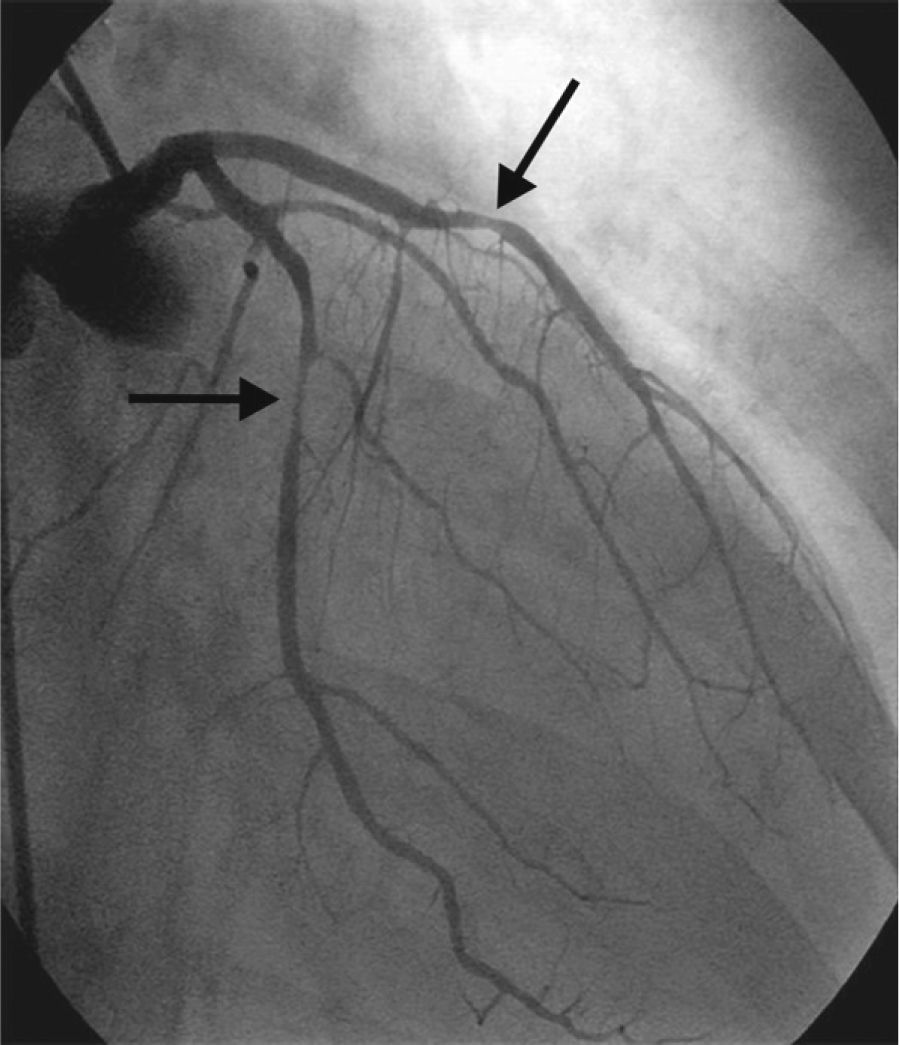
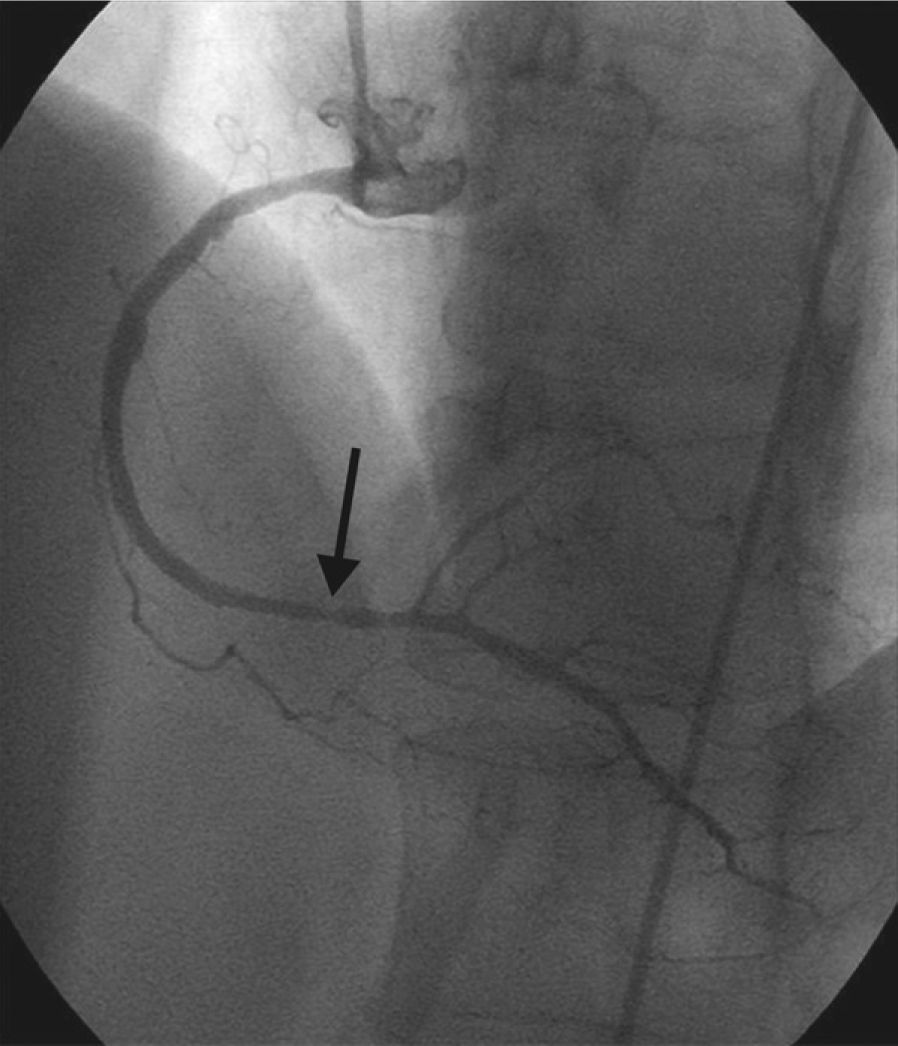
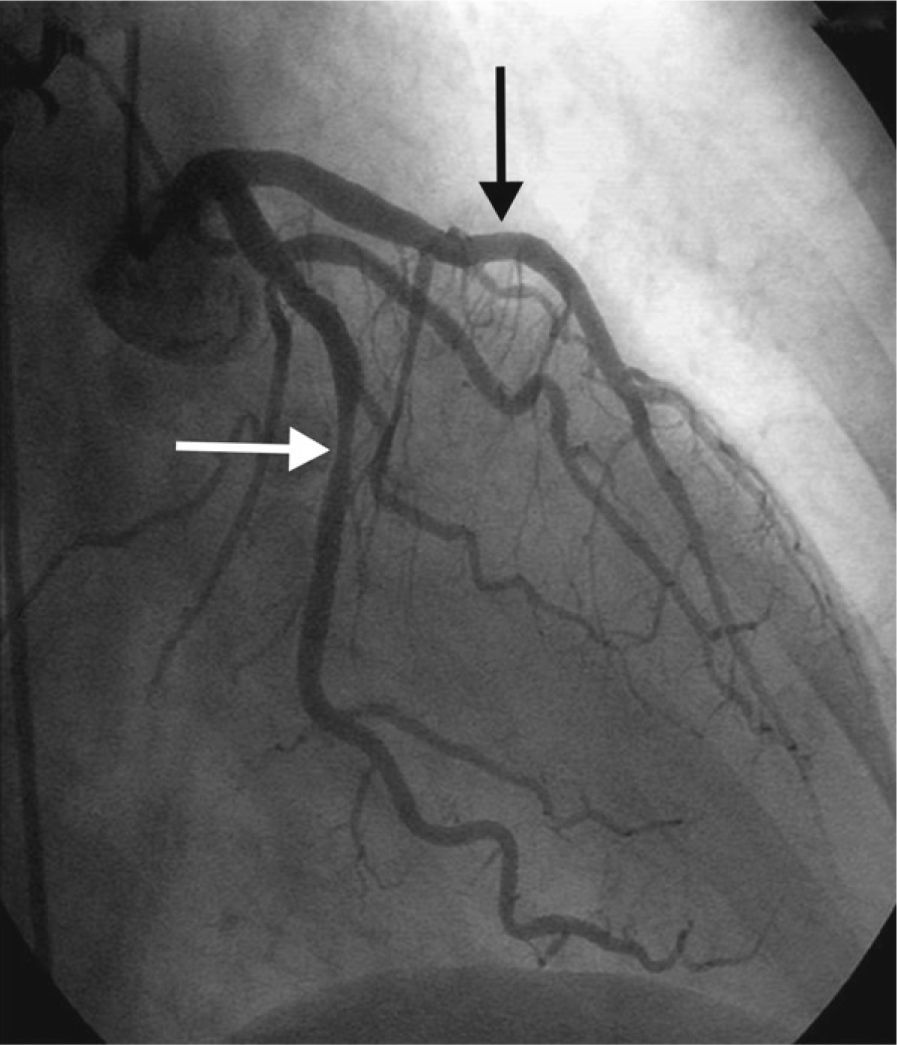
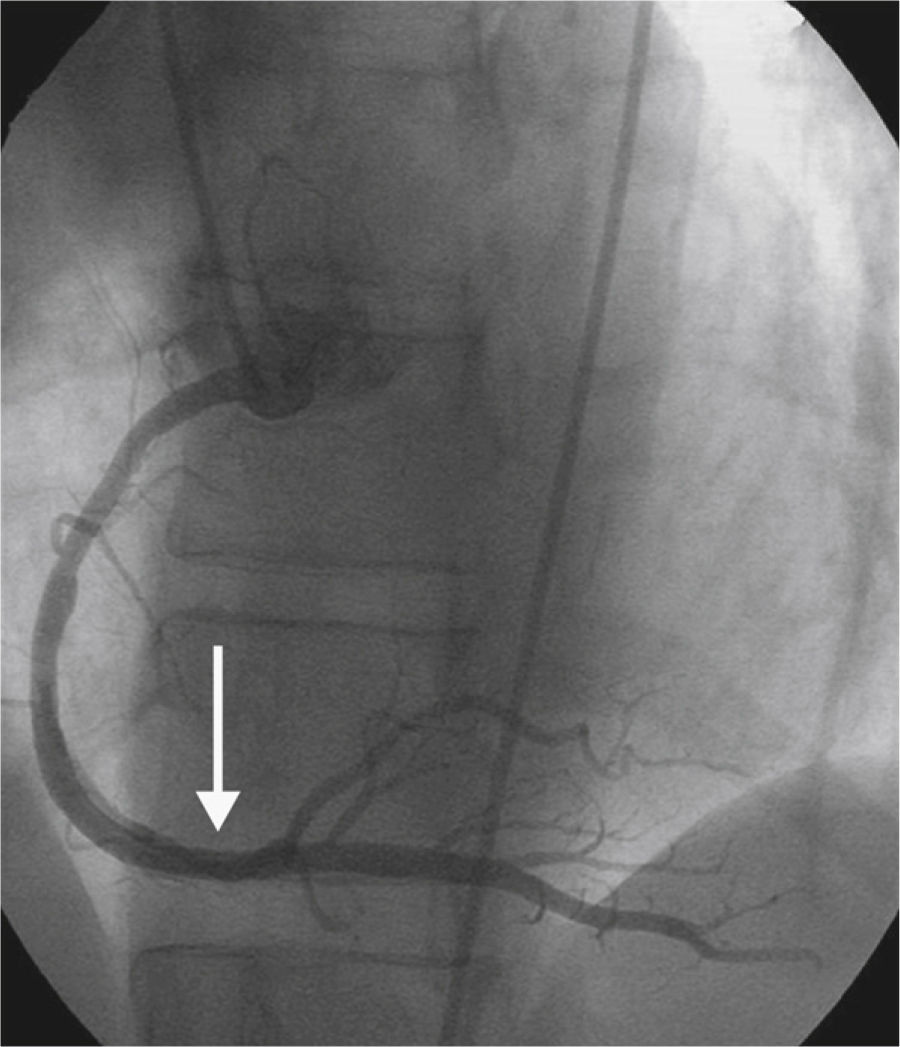
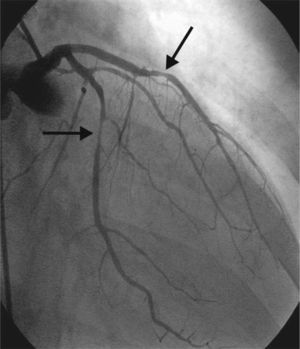
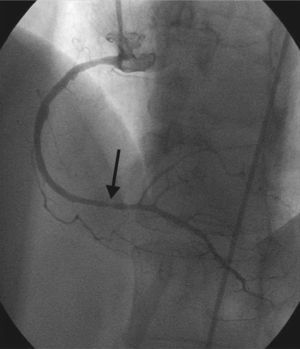
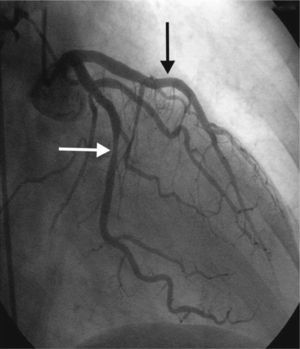
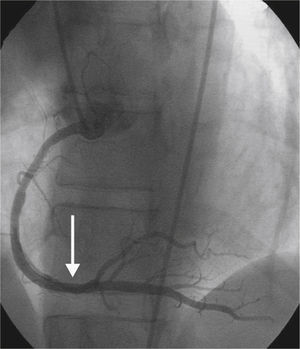
A 64-year-old white woman with a history of hypertension was admitted to hospital with new-onset chest pain consistent with angina. She had had multiple coronary angiograms (CA) four years previously for repeated episodes of typical chest pain and admissions. The CA showed non-obstructive coronary artery disease in the range of 40–50% in the left circumflex artery (LCx) which was confirmed to be non-obstructive by fractional flow reserve during the angiogram; no catheter-induced vasospasm occurred during the CA. Because of continued episodes of chest pain, she was taken off metoprolol and started on diltiazem 240mg once a day for possible vasospastic angina. She was then asymptomatic for the following four years, and also had a dobutamine stress echocardiogram, which was negative, about two months before the present admission for screening due to disease identified on her last CA. At this admission, she had new symmetrical anterolateral and inferior T inversion on the ECG consistent with ischemia; troponin levels were minimally elevated (0.3ng/ml). The patient had been seen by her primary care physician three days previously for a routine follow-up and was taken off diltiazem and started on nebivolol 10mg/day in addition to her medications of HCTZ 25mg and lisinopril 40mg/day, Lipitor 40mg, and enteric-coated aspirin 325mg/day for blood pressure (BP) control. In hospital she was started on nitro paste and intravenous (IV) heparin and her home medications continued. Because of continued chest pain in hospital and mildly elevated troponin I levels, she was scheduled for CA. She experienced chest pain at the beginning of the coronary angiogram, which initially revealed a 70% lesion and slow flow in the mid left anterior descending artery (LAD), a 90% lesion in the mid LCx and a 99% lesion in the ostium of the second obtuse marginal (OM2) (Figure 1, black arrow). The right coronary artery (RCA) had a distal 80–90% stenosis (Figure 2, black arrow). During preparation for percutaneous intervention in the LCx and OM2, intracoronary (IC) nitroglycerin was given for vessel sizing, after which there was resolution of the lesions in the LAD and decrease in the mid left LCx lesion to 50–60%, and resolution of the OM2 lesion, suggestive of significant reversible coronary artery spasm (Figures 3 and 4, white arrows). IC nitroglycerin was also administered in the RCA, in which lesion resolution was also seen. The coronary intervention was aborted, the patient's chest pain was resolved after IC nitroglycerin and she was started on IV nitroglycerin in the interim. Nebivolol was discontinued; diltiazem started in post-catheterization orders. She continued to have occasional episodes of chest pain for about 24hours after discontinuation of nebivolol. She was weaned from IV nitroglycerin the next day and started on oral isosorbide mononitrate. The following day the ECG changes resolved with no more episodes of chest pain; she was discharged home and was event-free in follow-up.
Nebivolol is a beta1-selective adrenergic receptor antagonist (at doses up to 10mg/day) with intrinsic vasodilator properties by its action on beta3 receptors causing nitric oxide (NO)-mediated vasodilatation.1–4 In a comparative, randomized, double-blind study, while both nebivolol 5mg/day and bisoprolol 10mg/day reduced systolic and diastolic BP to a similar extent, only nebivolol reduced the systemic vascular resistance index (2854±201 to 2646±186dynscm−5m2; p<0.05).5 In another study, Gullu et al. compared coronary flow reserve (CFR) in hypertensive patients using 8-week nebivolol 5mg/day and atenolol 50mg/day; nebivolol induced a non-significant increase in CFR (from 2.45 to 2.56; p=0.09), while atenolol was associated with a significant reduction in CFR (from 2.46 to 2.21; p=0.006).6 In other studies nebivolol showed significantly increased hyperemic coronary blood flow velocities.7,8 Nebivolol has been also shown to improve left ventricular function, symptoms and brachial flow-mediated dilatation in patients with coronary slow flow.9,10
However, coronary artery vasoconstriction caused or exacerbated by beta-blockers is a well-known phenomenon.11,12 First- and second-generation beta-blockers such as propranolol, practolol, metoprolol, and atenolol have been shown in animal and human studies to reduce coronary blood flow at rest due to vasoconstriction and reduction of myocardial oxygen demand by decreasing heart rate and BP.13
Coronary artery spasm is the mechanism of ischemic episodes in variant angina. Among the reported factors involved in coronary artery spasm are endothelial dysfunction with decreased NO levels, rho/rho-kinase pathway-mediated increased vascular smooth muscle contractility, enhanced phospholipase C-δ1 protein activity inducing focal smooth muscle cell hypersensitivity, imbalance in autonomic nervous activity, increased oxidative stress, chronic low-grade inflammation, magnesium deficiency, and genetic susceptibility.14,15 In a double-blind study by Robertson et al. in six variant angina patients, propranolol significantly increased the duration of anginal episodes with associated ECG changes.11
Several mechanisms have been proposed for beta-blocker mediated vasospasm, including blockade of beta2 vasodilator tone, direct effects on the coronary arteries, predominance of unopposed alpha-adrenergic tone, and blockade of beta1 effects with concomitant reduction in myocardial metabolic demands. However, the most potent mechanism seems to be blockade of beta1 adrenergic tone. In an animal study the selective beta1 adrenergic receptor blocker atenolol and the combined beta1- and beta2-adrenergic receptor blocker proponolol had similar effects on LCx diameter, cross-sectional area, blood flow and late diastolic coronary resistance. They both increased late diastolic coronary resistance and reduced coronary cross-sectional area, which suggests that the major mechanism of coronary vasoconstriction is blockade of beta1-adrenergic tone.16
We believe that our case shows that although nebivolol has intrinsic NO-mediated vasodilator properties, it still has the propensity to cause coronary vasospasm with blockade of beta1-mediated vasomotor tone in susceptible individuals like our patient. Catheter-induced coronary vasospasm was also among the differential diagnoses in our patient, but this usually occurs at the tip of the catheter; although it can occasionally be seen in the mid RCA there is also simultaneous involvement of the proximal vessel at the catheter tip. Catheter-induced vasospasm is usually a result of excessive manipulation or deeper engagement of the catheter and/or the patient's sensitivity and may vary with catheter size and type. In our patient there was no excessive manipulation or deep engagement of the catheters; with no left main or proximal RCA involvement, all lesions were distal from the catheter tip, which makes it unlikely that this was catheter-induced coronary vasospasm. Our patient's unstable angina symptoms, which began three days after starting nebivolol, new ECG changes, continued chest pain even before CA with visible vasospasm during the CA and the following ECG and clinical improvement with discontinuation of nebivolol, are suggestive of nebivolol-induced coronary vasospasm.
Our unique case demonstrates nebivolol-induced coronary artery spasm in a patient with a history of possible vasospastic angina. Nebivolol can exacerbate vasospastic angina in susceptible patients and this needs to be considered in differential diagnosis in patients with new-onset chest pain after starting nebivolol.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the responsible Clinical Research Ethics Committee and in accordance with those of the Helsinki Declaration of the World Medical Association.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.