We have read with interest the letter by Yalta et al. concerning our paper “Basal type ‘broken heart’ in a postpartum woman: utility of speckle tracking echocardiography”, which refers to a case of basal Takotsubo syndrome (TTS) in a 34-year-old woman following cesarean section.1,2 We agree with the perspective reflected by the title of the letter regarding the multiple facets of the condition and the syndromic approach to it. This perspective concerns TTS in general and not only the basal variants, and it is adopted by the International Expert Consensus Document.3
Although the pathophysiology of TTS is not fully understood, sympathetic activation and catecholamine-mediated effects are generally considered to play a central role.3 Accordingly, the authors’ question about the patient's sinus bradycardia at presentation seems reasonable at first; however, no single evidence-based answer can be provided. A logical assessment of the specific patient should surely take into account her persistent slow heart rate after myocardial recovery, as revealed by the echocardiographic video in our paper.2 An imbalance between the sympathetic and parasympathetic nervous systems and sinus node dysfunction related to coronary spasm, endothelial dysfunction, and/or microcirculatory impairment have been implicated as potential mechanisms of bradycardia in various case reports.4,5 On the other hand, it is noteworthy that a higher heart rate at presentation has been associated with a worse outcome.6,7
Cesarean section has been described as a trigger of postpartum TTS.3,8 In a study by Citro et al., 13 out of 28 (46%) post-cesarean section cases of TTS were non-apical types and four (14%) cases were basal.8 Since the list of triggering factors for TTS is constantly growing, it is unknown whether the surgery itself acting as an additional stressor in the context of the peripartum condition is the sole trigger or whether perioperative management including medication has any effect, either separately or combined with this medical state.
The authors’ hypothesis of more severe adrenergic stimulation in non-apical TTS cases is mostly based on published case reports and there is a lack of relevant data coming from studies. Among 31 cases of TTS induced by subarachnoid hemorrhage in a study by Kumai et al., it was shown that reverse TTS (according to the revised Mayo Clinic criteria9) was associated with significantly higher plasma epinephrine levels than the classic apical pattern.10 However, no significant differences in norepinephrine levels or in clinical and prognostic characteristics were found. While little can be said about the severity of stress because of the lack of objective comparisons, there are some data on the frequency of stress. In studies by Song et al. and Ramaraj et al., reverse TTS was related to triggering stress in all cases, unlike in mid-ventricular or apical types.11,12 Additionally, it seems that non-apical TTS occurs more often in younger patients and in those with neurological disorders, while the susceptibility of females to TTS is widely accepted.3,13
As regards invasive coronary angiography in our case, no coronary lesions were observed, but there was some delayed contrast opacification in distal vessels, which was graded as Thrombolysis In Myocardial Infarction (TIMI) 2-3 flow. While the prognostic value of TIMI flow grade as a marker of microvascular function in TTS is not well established, Montone et al. showed an association between TIMI grade 2 flow and worse clinical outcome (more in-hospital complications and poorer long-term clinical outcome) in patients with TTS.14 Nevertheless, our patient's in-hospital and long-term outcome were excellent, experiencing neither arrhythmias nor heart failure.
Acute significant mitral regurgitation (MR) in cases of apical TTS was associated with adverse outcomes by Parodi et al.15 In their study, left ventricular ejection fraction at presentation and systolic anterior motion of the mitral valve were the only independent predictors of acute MR.15 Other mechanisms of MR in TTS that have been studied are papillary muscle displacement and leaflet tethering.16 Pending data from relevant studies specifically regarding basal types, we agree with Yalta et al.’s logical explanation primarily implicating mitral annulus dilatation as a result of basal ballooning. In our case, the mitral annulus diameter in the acute setting and on recovery was measured at 36mm and 28mm respectively (measurements in mid-diastole using parasternal long-axis view). Special reference should be made to the increased cardiac output related to pregnancy and the immediate postpartum period, which could have enhanced the severity of MR in this patient.
Our paper aimed to highlight longitudinal strain (LS) as an adjunctive diagnostic tool to conventional echocardiography, not as a substitute for it. Indeed, we believe that the characteristic bull's eye plot showing the impairment of basal LS values in a circumferential pattern sparing mid-ventricular and apical segments was of utmost importance in confirming the correct diagnosis. Besides, the use of strain imaging in the acute setting is recommended by the European Association of Cardiovascular Imaging for both left and right ventricles.16 Its value seems to be more evident in non-apical cases and in those without marked left ventricular segmental systolic impairment, both of which are harder to diagnose correctly. Certainly, measurement of segmental and global LS in the long term, along with conventional echocardiographic systolic measurements, is valuable and useful for the assessment of complete myocardial recovery. Unfortunately, further LS imaging beyond one month after the acute presentation is not available for our published case.
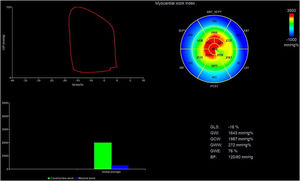
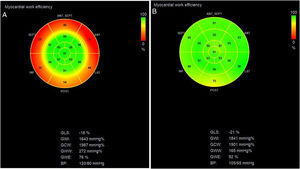
Finally, given the opportunity provided by this letter, we would like to update the case with the novel concept of myocardial work. The patient's global work index and global constructive work (GCW) were in the lower levels of the reference ranges reported by the NORRE study for her age (20-40 years) and female subgroup, while global wasted work (GWW) was high17 (Figure 1). As global work efficiency (GWE) is derived by dividing GCW by the sum of GCW and GWW,17 this parameter was significantly reduced (Figure 2A). This is not surprising given that the basal segments made little contribution to ejection. At one-month review, GWE increased from 76% to 92%, with apparent improvement of basal segments showing recruitment of their contraction and left ventricular recovery (Figure 2B).
Measurement of left ventricular myocardial work indices by two-dimensional transthoracic echocardiography in the acute phase. Results from myocardial work analysis: global work index (GWI): 1643 mmHg%, global constructive work (GCW): 1987 mmHg%, global wasted work (GWW): 272 mmHg%, global work efficiency (GWE): 76%. Reference ranges reported by the NORRE study for the age (20-40 years) and female subgroup: GWI 1800±251 mmHg%, GCW 2109±289 mmHg%, GWW 48-145 mmHg%, GWE 94-97%.17 The bull's-eye plot of myocardial work index shows very low values in basal segments (blue-coded areas) and an apparent increase in mid-ventricular and apical values. ANT: anterior wall; ANT_SEPT: anteroseptal wall; BP: blood pressure; GLS: global longitudinal strain; INF: inferior wall; LAT: lateral wall; POST: posterior wall; SEPT: septal wall.
Bull's-eye plots of left ventricular myocardial work efficiency derived by two-dimensional transthoracic echocardiography. (A) In the acute phase, there was significant reduction in regional values of basal segments (red-coded areas); (B) on review one month later, basal segments had recovered. Almost all myocardial walls contributed equally to left ventricular ejection, and global work efficiency (GWE) increased from 76% to 92%. ANT: anterior wall; ANT_SEPT: anteroseptal wall; BP: blood pressure; GCW: global constructive work; GLS: global longitudinal strain; GWI: global work index; GWW: global wasted work; INF: inferior wall; LAT: lateral wall; POST: posterior wall; SEPT: septal wall.
The authors have no conflicts of interest to declare.