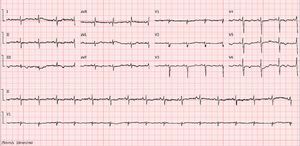
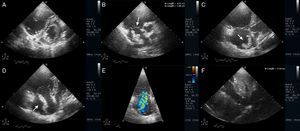
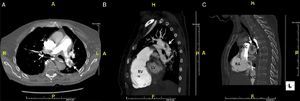
An 88-year-old woman was admitted with syncope and rapidly evolved with shock. Her medical history was notable for recent orthopedic surgery. The electrocardiogram showed ST-segment depression in the precordial and inferior leads (Figure 1). Rapid troponin I assay was positive. Bedside echocardiography revealed a dilated and dysfunctional right ventricle, with akinesia of the lateral wall and paradoxical interventricular septal motion (Figure 2A). Remarkably, a large, worm-like, mobile, free-floating right atrial mass was noted, insinuating through the tricuspid valve during systole (Figure 2B–D). Acute pulmonary embolism (PE) with right heart thromboembolus was strongly suspected, so prompt resuscitation and anticoagulant therapy were started, while emergency thoracic computed tomography angiography confirmed bilateral central emboli (Figure 3A–C). Despite the high bleeding risk, thrombolysis was undertaken, given the life-threatening condition, with gradual improvement in clinical status and no major bleeding complications. No right heart thromboembolus was found in the follow-up echocardiogram and the patient had an uneventful hospital course.
Electrocardiogram (ECG) showing ST-segment depression and T-wave inversion in the precordial and inferior leads. Importantly, detailed retrospective analysis of the admission ECG reveals a shift of the frontal QRS to the right, with a prominent S wave in lead I and an inverted T wave in lead III, as well as low QRS voltage in the right precordial leads and a pseudoinfarction pattern (Qr in V1 with poor R-wave progression/excessive clockwise rotation with rS up to V6), an indication of right ventricular overload/injury.
Transthoracic echocardiogram in left parasternal short-axis view depicting a dilated right ventricle with leftward septal shift, suggestive of right ventricular pressure overload (A). Parasternal short-axis view of the basal right ventricle (RV) (B) and RV modified apical 4-chamber view (C and D) showing a dilated right ventricle and a free-floating right atrial mass (about 4.01 × 1.96 cm). Severe tricuspid regurgitation due to annular dilatation (E) and dilated inferior vena cava with no respiratory variation (F) are also shown; estimated systolic pulmonary pressure was 54 mmHg (not shown). The findings were highly suggestive of acute pulmonary embolism with incidental right heart thromboembolus in transit.
A central bilateral intraluminal filling defect (arrows) is seen, consistent with pulmonary emboli (A – transaxial view; B and C – sagittal views). A thromboembolus (arrowhead) is also seen in the right atrium (C). IVC: inferior vena cava; LV: left ventricle; RA: right atrium; RV: right ventricle; SVC: superior vena cava.
Right heart thromboemboli in transit are an incidental finding in up to 20% of patients with acute high-risk PE, and are associated with hemodynamic compromise and worse prognosis, especially with mobile, worm-like type A thromboembolus. Bedside echocardiography is particularly helpful in making a rapid presumptive diagnosis, avoiding unnecessary delay in treatment. Their management remains controversial, with concerns of bleeding complications, fragmentation and new embolization with readily available thrombolytic therapy. Even so, their natural history should be borne in mind when evaluating bleeding risk, particularly in elderly patients, whose perceived risk could exclude them from a potentially life-saving therapy.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
Supplementary material associated with this article can be found in the online version available at doi:10.1016/j.repc.2012.07.008.