Psoriasis is a common chronic inflammatory disease associated with serious comorbidities. In recent years, increased mortality due to cardiovascular disease (myocardial infarction and stroke) has been documented in patients with severe psoriasis. Patients with psoriasis have a higher prevalence of traditional cardiovascular risk factors such as diabetes, hypertension, dyslipidemia and obesity, but it has been suggested that the chronic inflammatory nature of psoriasis is also a contributing and potentially an independent risk factor for the development of cardiovascular disease.
The authors highlight the need for early identification and treatment of psoriasis‐related comorbidities and cardiovascular disease, as well as effective treatment of psoriasis, in order to reduce the underlying systemic inflammation, and also the importance of a multidisciplinary approach of severe psoriasis patients to optimize the diagnosis, monitoring and treatment of various comorbidities, so as to prevent cardiovascular events.
A psoríase é uma doença inflamatória crónica, comum, associada a comorbilidades importantes. Nos últimos anos tem sido demonstrado que os doentes com psoríase grave têm um risco aumentado de mortalidade por doenças cardiovasculares, como enfarte agudo do miocárdio ou acidente vascular cerebral. Por um lado os doentes com psoríase têm uma prevalência aumentada de fatores de risco cardiovasculares como diabetes, hipertensão, dislipidemia e obesidade, e por outro, a natureza inflamatória da doença parece contribuir e ser um fator de risco independente para o desenvolvimento de doença cardiovascular.
Os autores pretendem alertar para a necessidade da identificação precoce e tratamento das diversas comorbilidades associadas à psoríase e doença cardiovascular, assim como o tratamento correto e eficaz da psoríase, diminuindo a inflamação sistémica subjacente, e para a importância de uma abordagem multidisciplinar na tentativa de otimizar o diagnóstico, monitorização e tratamento das diversas comorbilidades, prevenindo os eventos cardiovasculares.
Psoriasis is a common chronic inflammatory skin disease that affects 1%–3% of the general population.1 It affects both sexes equally and people of all ages, with incidence peaks in early adult life (20s) and in later adult life (50s and 60s).2,3 Usually it is clinically distinct and consequently easy to diagnose, being characterized by sharply demarcated erythematous plaques covered by silvery‐white scales preferentially on the elbows, knees, scalp, umbilicus and lumbar area.4 The majority of patients, approximately 80%, have limited disease (<10% body surface area), but approximately 20% have more extensive skin involvement (>10% body surface area).5 Although psoriasis is rarely life‐threatening, its psychological impact on patients’ quality of life is similar to that for diabetes, cancer or heart disease.6 However, while most patients report its negative impact on their quality of life, psoriasis appears to be more than skin deep. As understanding of its pathophysiology has evolved, from a disorder of keratinocytes to dysregulation of the immune system mediated by cytokines, psoriasis has come to be considered a systemic inflammatory disorder associated with numerous medical comorbidities.7
Large epidemiologic studies have found that patients with psoriasis have a higher prevalence of traditional cardiovascular risk factors such as diabetes, hypertension, dyslipidemia, smoking, obesity and metabolic syndrome compared with the general population.8–12 Importantly, even after adjusting for these risk factors, psoriasis has been associated with clinically significant increased risk of cardiovascular disease (myocardial infarction [MI] and stroke) and cardiovascular mortality13–20 (Table 1). For this reason, patients with severe psoriasis appear to have a 6‐year reduction in life expectancy.21
Severe psoriasis and cardiovascular mortality, myocardial infarction and stroke.
| Outcome | Patients, n | HR or RR (95% CI) | Confounders controlled |
| Cardiovascular mortality | |||
| Abuabara, 201014 | Severe psoriasis: 3603Controls: 14 330 | HR 1.57(1.26–1.96) | Age and gender |
| Ahlehoff, 201115 | Severe psoriasis: 2793Controls: 4 478 926 | RR 1.65(1.33–2.05) | Age, gender, comorbidities, medication and socioeconomic status |
| Myocardial infarction | |||
| Gelfand, 200616 | Severe psoriasis: 3837Controls: 556 995 | HR 7.08(3.06–16.36) | Age, gender, hypertension, diabetes, cholesterol, smoking, prior myocardial infarction and body mass index |
| Mehta, 201118 | Severe psoriasis: 3603Controls: 14 330 | HR 1.53(1.26–1.85) | Age, gender, hypertension, diabetes, cholesterol and smoking |
| Ahlehoff, 201219 | Severe psoriasis: 2793Controls: 4 478 926 | RR 1.45(1.10–1.90) | Age, gender and medical comorbidities (individual comorbidities not reported) |
| Stroke | |||
| Gelfand, 200920 | Severe psoriasis: 3603Controls: 14 330 | HR 1.43(1.10–1.87) | Age, gender, hypertension, diabetes, cholesterol, smoking and neurovascular disease |
| Ahlehoff, 201219 | Severe psoriasis: 2793Controls: 4 478 926 | RR 1.65(1.33–2.05) | Age, gender, social demographics and medical comorbidities (individual comorbidities not reported) |
CI: confidence interval; HR: hazard ratio; RR: relative risk.
In a study including more than 130 000 patients with psoriasis, Gelfand et al. found that the adjusted relative risk (RR) of MI in 30‐year‐old patients with mild psoriasis compared with controls was 1.29 (95% confidence interval [CI], 1.14–1.46), but rose to 3.10 (95% CI, 1.98–4.86) in severe forms of the disease.16 Remarkably, the risk persisted after adjustment for major risk factors for MI, suggesting that psoriasis itself confers an independent risk of MI. Using the same database, the authors observed that patients with severe psoriasis had an increased risk of cardiovascular mortality (defined as mortality caused by MI, stroke, or peripheral vascular disease) that was independent of traditional risk factors (hazard ratio [HR] 1.57; 95% CI, 1.26–1.96). The relative risk of cardiovascular mortality was modified by age, with a higher RR in younger individuals (2.69 for 40‐year‐olds [95% CI, 1.45–4.99] and 1.92 for 60‐year‐olds [95% CI, 1.41–2.62]), suggesting a process of accelerated cardiovascular disease in younger severe psoriasis patients.17 The authors also estimated that severe psoriasis confers an additional 6.2% absolute risk of 10‐year major adverse cardiac events compared to the general population, with important therapeutic implications for cardiovascular risk stratification and prevention in patients with severe psoriasis.18
Psoriasis appears to be an independent risk factor for subclinical atherosclerosis, as an increased prevalence of subclinical atherosclerosis, diagnosed using various surrogate markers including carotid artery intima‐media thickness, arterial stiffness, flow‐mediated dilatation and nitroglycerin‐induced dilatation or aortic elasticity, has been reported in several studies comparing with non‐psoriatic populations, controlled for age, gender and traditional cardiovascular risk factors.22–24 Psoriasis has also been associated with significantly increased frequency of coronary artery calcification in a study that matched patients for age, gender and known cardiovascular risk factors, not only identifying psoriasis as an independent risk factor for coronary artery calcification but also demonstrating the systemic nature of the disease.25
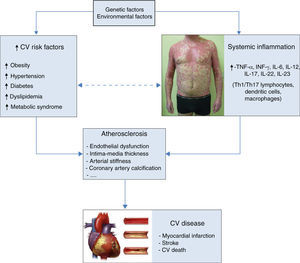
The connection between psoriasis and atherosclerosis may be due to a common genetic basis, an increased prevalence of traditional cardiovascular risk factors, and the chronic inflammation that occurs in patients with psoriasis, as inflammation has a central role in both diseases (Figure 1). Psoriasis is nowadays considered a T‐cell mediated disease rather than a keratinocyte disease, and the role of T cells in the pathology of the disease demonstrates the extent of systemic involvement. Th‐1, Th‐17 and Th‐22 cell populations are expanded and stimulated to release inflammatory cytokines, including TNF‐α, IL‐17 and IL‐22.26 Thus the inflammation that drives psoriatic pathology is systemic, and there is evidence that it contributes to immunologic and metabolic changes that aggravate and perpetuate psoriasis as well as to the development of comorbidities.27 Both conditions are associated with T‐lymphocyte mediated adaptive immune events and mechanisms involving innate immunity. Reduced numbers and activity of T‐regulatory cells and the resulting hyperactivity of Th1/Th17 subsets are encountered in both psoriasis and atherosclerosis, while common innate immune mechanisms include lesional complement activation and toll‐like receptor‐mediated events leading to cytokine‐driven inflammation.28,29 The term ‘psoriatic march’ has been used to describe this process, which proceeds in a stepwise manner, beginning with genetic and possibly environmental factors that initiate disease‐specific immunologic pathways leading to psoriasis and subsequent comorbidities as a consequence of chronic inflammation. In this model, systemic inflammation associated with psoriasis enhances insulin resistance, causing endothelial dysfunction, atherosclerosis and possible coronary events.30 Another important factor implicated in the accelerated atherosclerosis observed in psoriasis is the atherogenic side‐effects of several systemic agents used to treat psoriasis, such as retinoid‐induced dyslipidemia and cyclosporine‐induced hypertension.
However, treatment aimed at reducing the severity of the skin disease would also reduce the inflammatory burden. The use of methotrexate and TNF‐α inhibitors has been reported to reduce the risk of cardiovascular events and cardiovascular mortality in patients with rheumatoid arthritis.31 In psoriasis, the data are more limited. Improvement in cardiovascular risk biomarkers (high‐sensitivity C‐reactive protein, vascular endothelial growth factor and the adipokines resistin and adiponectin) has been documented in patients with severe psoriasis responding to continuous systemic therapy, showing that patients’ metabolic state improved with inflammatory control.32 Preliminary evidence suggests that TNF‐α inhibitors may improve endothelial function in psoriasis populations and epidemiologic studies show that they may also reduce the risk of adverse cardiovascular events.33,34
Despite increasing evidence of the association between psoriasis and cardiovascular disease and the importance of identifying and modifying psoriasis‐associated cardiometabolic comorbidities in order to decrease cardiovascular events and mortality, it appears that this has not been fully implemented in clinical practice. A high prevalence of underdiagnosis and undertreatment of cardiovascular risk factors was recently documented in a large cohort of patients (n=2899) with moderate to severe psoriasis enrolled in a phase III clinical trial of ustekinumab; even when these cardiovascular risk factors had been diagnosed there was a high rate of failure to achieve treatment goals in accordance with published guidelines.35 Additionally, although in 2008 the National Psoriasis Foundation and the American Journal of Cardiology released guidelines for screening and treatment of cardiovascular risk factors in patients with psoriasis, Parsi et al., assessing cardiovascular risk factor screening practice in patients with psoriasis and awareness of primary care physicians and cardiologists of worse cardiovascular outcomes in these patients, found that less than half of these physicians screened patients with psoriasis for cardiovascular risk factors in accordance with the guidelines or were aware of the higher rate of major adverse cardiovascular events in patients with psoriasis compared with the general population, although cardiologists were significantly more likely to screen psoriasis patients for dyslipidemia and were more likely to be aware of their increased cardiovascular risk. Increased experience caring for patients with psoriasis was associated with better adherence to screening guidelines.36 Increasing the volume of publications in internal medicine and cardiology journals highlighting the association between psoriasis and cardiovascular disease could be a way to improve awareness in the non‐dermatology community.
To summarize, the risk of cardiovascular morbidity and mortality is higher in patients with psoriasis than in the general population. Unlike other inflammatory diseases, psoriasis is readily apparent to physicians, both dermatologists and non‐dermatologists, which should facilitate prompt evaluation for cardiovascular risk factors and cardiovascular disease.
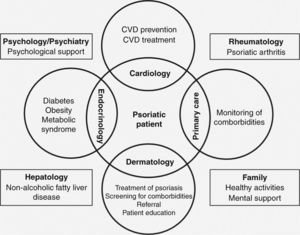
A multidisciplinary approach should be adopted in the care of patients with psoriasis, particularly in severe cases with multiple comorbidities or cardiovascular disease. Dermatologists are in an important, sentinel‐like position, able to detect and respond to early indications of cardiovascular risk factors and comorbidities in psoriasis patients. They should be able to recognize these risk factors, advise and educate patients, and whenever necessary refer them to cardiologists for appropriate treatment. At the same time, cardiologists and other physicians should be aware of this association and the beneficial effect of treating psoriasis on cardiovascular outcomes, and when appropriate refer patients to a dermatologist (Figure 2).
All psoriasis patients should be encouraged to correct their modifiable cardiovascular risk factors, particularly obesity and smoking, and to adopt healthy lifestyle behaviors such as regular exercise. Patients with moderate to severe psoriasis patients, even if otherwise healthy, should be recognized as being at moderately increased risk of cardiovascular disease, and should probably be managed as patients at intermediate risk of cardiovascular disease.
Efforts are needed to develop appropriate treatment strategies and referral networks to ensure appropriate management of these comorbidities, which will likely lead to improvements in patient outcomes.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.