The use of non-invasive mechanical ventilation (NIMV) reduces the rate of intubation and mortality in patients with acute pulmonary edema (APE).1 High flow nasal cannula oxygen (HFNC) may offer an alternative to ventilatory support in patients with APE2,3 with theoretical advantages related to patient adaptation, comfort and less of a need for staff training to achieve optimal therapy. However, clinical efficacy and safety of HFNC compared to NIMV in APE is not well established.
We performed a prospective, observational study between November 2018 and January 2020. Forty-seven patients with criteria of non-hypercapnic APE were classified into two groups according to the initial therapy: Continuous positive airway pressure (CPAP)/NIPPV versus HFNC. The selected ventilatory therapy was at the discretion of the treating clinician and patients with cardiogenic shock, hemodynamic instability, hypercapnic respiratory failure (partial pressure of carbon dioxide >45 mmHg) were excluded. The device used for NIMV ventilation was a V V60® (Philips, Respironics Inc, MA, USA), whereas for HFNC therapy an Airvo™ 2 (Fisher & Paykel Healthcare, East Tamaki, New Zealand) was used. Primary composite endpoint was death or need for orotracheal intubation within 30 days after admission. The secondary endpoints were length of hospital stay, admission to the critical care unit and composite of orotracheal intubation/change of therapy secondary to respiratory worsening.
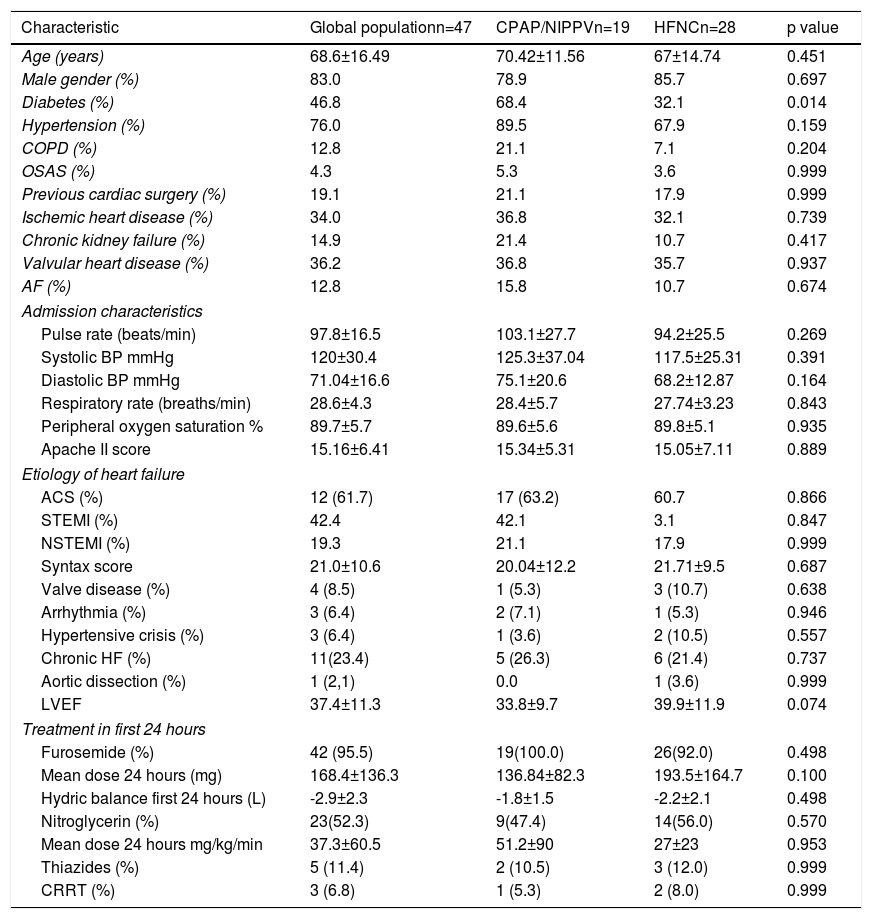
The mean age was 68.8±13.1 years, 83% male. Twenty-eight (59.6%) patients received HFNC and 19 (40.4%) NIPPV-CPAP as initial treatment for APE. De novo acute heart failure (HF) was the initial presentation in 76.6% and 61.7% was secondary to acute coronary syndrome. Disease severity at admission was similar in both groups (Table 1). In patients treated with HFNC, initial flow was 44.3±22.7 L/min and 37°C. In the case of CPAP treatment, the initial pressure was 7±2 cmH20 and in NIPPV patients, the inspiratory pressure was 14±4 and expiratory 6±2 cmH20.
Baseline characteristics of the patients according to the modality of noninvasive ventilation therapy.
| Characteristic | Global populationn=47 | CPAP/NIPPVn=19 | HFNCn=28 | p value |
|---|---|---|---|---|
| Age (years) | 68.6±16.49 | 70.42±11.56 | 67±14.74 | 0.451 |
| Male gender (%) | 83.0 | 78.9 | 85.7 | 0.697 |
| Diabetes (%) | 46.8 | 68.4 | 32.1 | 0.014 |
| Hypertension (%) | 76.0 | 89.5 | 67.9 | 0.159 |
| COPD (%) | 12.8 | 21.1 | 7.1 | 0.204 |
| OSAS (%) | 4.3 | 5.3 | 3.6 | 0.999 |
| Previous cardiac surgery (%) | 19.1 | 21.1 | 17.9 | 0.999 |
| Ischemic heart disease (%) | 34.0 | 36.8 | 32.1 | 0.739 |
| Chronic kidney failure (%) | 14.9 | 21.4 | 10.7 | 0.417 |
| Valvular heart disease (%) | 36.2 | 36.8 | 35.7 | 0.937 |
| AF (%) | 12.8 | 15.8 | 10.7 | 0.674 |
| Admission characteristics | ||||
| Pulse rate (beats/min) | 97.8±16.5 | 103.1±27.7 | 94.2±25.5 | 0.269 |
| Systolic BP mmHg | 120±30.4 | 125.3±37.04 | 117.5±25.31 | 0.391 |
| Diastolic BP mmHg | 71.04±16.6 | 75.1±20.6 | 68.2±12.87 | 0.164 |
| Respiratory rate (breaths/min) | 28.6±4.3 | 28.4±5.7 | 27.74±3.23 | 0.843 |
| Peripheral oxygen saturation % | 89.7±5.7 | 89.6±5.6 | 89.8±5.1 | 0.935 |
| Apache II score | 15.16±6.41 | 15.34±5.31 | 15.05±7.11 | 0.889 |
| Etiology of heart failure | ||||
| ACS (%) | 12 (61.7) | 17 (63.2) | 60.7 | 0.866 |
| STEMI (%) | 42.4 | 42.1 | 3.1 | 0.847 |
| NSTEMI (%) | 19.3 | 21.1 | 17.9 | 0.999 |
| Syntax score | 21.0±10.6 | 20.04±12.2 | 21.71±9.5 | 0.687 |
| Valve disease (%) | 4 (8.5) | 1 (5.3) | 3 (10.7) | 0.638 |
| Arrhythmia (%) | 3 (6.4) | 2 (7.1) | 1 (5.3) | 0.946 |
| Hypertensive crisis (%) | 3 (6.4) | 1 (3.6) | 2 (10.5) | 0.557 |
| Chronic HF (%) | 11(23.4) | 5 (26.3) | 6 (21.4) | 0.737 |
| Aortic dissection (%) | 1 (2,1) | 0.0 | 1 (3.6) | 0.999 |
| LVEF | 37.4±11.3 | 33.8±9.7 | 39.9±11.9 | 0.074 |
| Treatment in first 24 hours | ||||
| Furosemide (%) | 42 (95.5) | 19(100.0) | 26(92.0) | 0.498 |
| Mean dose 24 hours (mg) | 168.4±136.3 | 136.84±82.3 | 193.5±164.7 | 0.100 |
| Hydric balance first 24 hours (L) | -2.9±2.3 | -1.8±1.5 | -2.2±2.1 | 0.498 |
| Nitroglycerin (%) | 23(52.3) | 9(47.4) | 14(56.0) | 0.570 |
| Mean dose 24 hours mg/kg/min | 37.3±60.5 | 51.2±90 | 27±23 | 0.953 |
| Thiazides (%) | 5 (11.4) | 2 (10.5) | 3 (12.0) | 0.999 |
| CRRT (%) | 3 (6.8) | 1 (5.3) | 2 (8.0) | 0.999 |
ACS: acute coronary syndrome; AF: atrial fibrillation; BP: blood pressure, CCRT: continuous renal replacement therapy; COPD: chronic obstructive pulmonary disease; CPAP: continuous positive airway pressure; HF: heart failure; HFNC: high flow nasal cannula; LVEF: left ventricular ejection fraction. MCS: mechanical circulatory support, NIPPV: noninvasive positive-pressure ventilation; OSAS: obstructive sleep apnea syndrome, STEMI: ST elevation myocardial infarction. NSTMI: non ST elevation myocardial infarction.
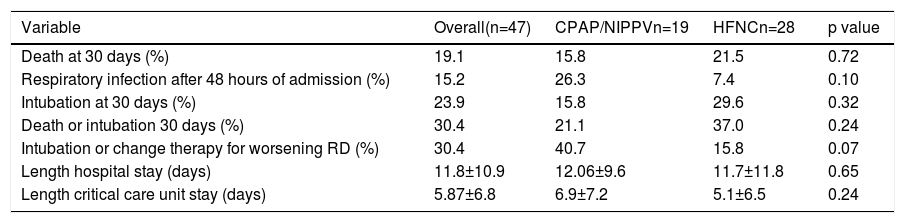
There was no significant difference in 30-day mortality or combined objective of death/intubation in HFNC vs. NIMV (21.5 vs. 15.8 p=0.72) and (37.0 vs. 21.1% p=0.24). However the failure of therapy, defined as the combined objective of intubation or change of therapy due to respiratory worsening, was more frequent in the HFNC group (40.7 vs. 15.8 p=0.07). In-hospital or coronary care unit long stay was no different between both groups (Table 2).
Primary and secondary ends point comparing noninvasive positive-pressure ventilation and high flow nasal cannula.
| Variable | Overall(n=47) | CPAP/NIPPVn=19 | HFNCn=28 | p value |
|---|---|---|---|---|
| Death at 30 days (%) | 19.1 | 15.8 | 21.5 | 0.72 |
| Respiratory infection after 48 hours of admission (%) | 15.2 | 26.3 | 7.4 | 0.10 |
| Intubation at 30 days (%) | 23.9 | 15.8 | 29.6 | 0.32 |
| Death or intubation 30 days (%) | 30.4 | 21.1 | 37.0 | 0.24 |
| Intubation or change therapy for worsening RD (%) | 30.4 | 40.7 | 15.8 | 0.07 |
| Length hospital stay (days) | 11.8±10.9 | 12.06±9.6 | 11.7±11.8 | 0.65 |
| Length critical care unit stay (days) | 5.87±6.8 | 6.9±7.2 | 5.1±6.5 | 0.24 |
CPAP: continuous positive airway pressure; HFNC: high flow nasal cannula; RD: respiratory distress; NIPPV: noninvasive positive-pressure ventilation.
In this study, HFNC was not associated with increased 30-day mortality in patients with non-hypercapnic APE, but was associated with non-significant increase in treatment failure secondary to respiratory worsening. These findings could be explained for several reasons related to the physiological effects of positive end-expiratory pressure (PEEP) over compliance, alveolar recruitment, decrease of left ventricular afterload and right ventricular preload.4,5 Although HFNC seems to have an impact on RV preload, PEEP is often inconsistent, depending on the flow delivered and patient collaboration. This effect could explain that despite the good results in hypoxemic respiratory failure of other causes,5 it has no benefit in APE.6 Although the use of HFNC possibly does not provide benefits in the treatment of APE over NIMV, it could have better results in decompensated HF over conventional oxygen2,3,6 or in weaning from NIMV therapy. Randomized studies are needed.
Conflicts of interestNone declared.