Chronic total occlusion (CTO) of the left main coronary artery (LMCA) is an infrequent finding. Revascularization is recommended in the presence of demonstrated viability or ischemia. Coronary artery bypass grafting (CABG) has long been considered the preferred option. Patients with previous CABG due to LMCA disease with occlusion of one graft and progression of the LMCA to CTO constitute a special population, as just one ischemic artery remains. For these patients, there is no other option for revascularization other than cardiac surgery (requiring resternotomy) or percutaneous coronary intervention (PCI) of the LMCA.
Methods and ResultsOut of 620 patients with CTO diagnosed in our center, we identified five with previous CABG due to LMCA disease for a retrospective case series. They had occlusion of one graft and progression of the LMCA to CTO. All five underwent PCI. Each patient received a functional classification for angina, myocardial ischemic tests, and a follow-up coronary angiogram during a median follow-up of 63 months. Coronary angiogram showed CTO of the semi-protected LMCA lesions with two CABGs previously performed in all patients, one occluded and the other patent. Three patients had occluded saphenous vein grafts to the circumflex coronary artery, and the rest had left internal mammary artery-left anterior descending artery CABG failure. Ischemia and viability were demonstrated. Surgery was ruled out due to high surgical risk. PCI due to CTO of the LMCA with drug-eluting stents was performed. In a five-year follow-up period, four patients remained asymptomatic and event free. One post-PCI death occurred from non-cardiovascular cause.
ConclusionsPCI due to CTO of the LMCA following CABG can be successful and safe and can provide sustained clinical improvements in selected cases.
A oclusão crónica total (OCT) do tronco comum (TC) coronário é um achado pouco frequente. A revascularização é recomendada na presença de viabilidade ou de isquemia comprovada. A coronary artery bypass grafting (CABG) tem sido durante muito tempo a opção preferencial. Os doentes com CABG prévia devida a doença do TC com oclusão de um enxerto e progressão para oclusão crónica total do tronco comum constituem uma população especial, uma vez que fica apenas uma artéria com isquemia. Para esses doentes não existe outra opção de revascularização além da cirurgia cardíaca – com necessidade de reesternotomia – ou a intervenção coronária percutânea do tronco comum.
Métodos e resultadosDos 620 doentes com oclusões coronárias totais diagnosticadas no nosso centro, identificamos como séries de casos retrospetivos, cinco com CABG prévia devida a doença do TC, que tinham uma oclusão de um enxerto e progressão da doença do TC para oclusão crónica total. Os cinco foram submetidos a intervenção coornária percutânea (ICP). Cada doente recebeu a classificação funcional de angina, de testes de isquemia do miocárdio e o seguimento com angiografía coronária durante o tempo médio de 63 meses de seguimento. O angiograma coronário mostrou oclusão coronária total das lesões semiprotegidas do TC com duas pontagens previamente feitas em todos os doentes, uma ocluída e a outra permeável. Três doentes tinham enxertos de veia safena para a artéria coronária circunflexa (Safena-CX) ocluídos e os restantes tinham insuficiência da pontagem com mamária interna esquerda para a artéria coronária descendente anterior (MIE-DA). Foi demonstrada isquemia ou viabilidade. A opção cirúrgica foi recusada devido ao elevado risco cirúrgico. Foi feita a ICP da oclusão coronária total do TC com stents revestidos de fármaco. Em cinco anos de seguimento, quatro doentes permaneceram assintomáticos e livres de eventos. Ocorreu uma morte após ICP devido a causa não cardiovascular.
ConclusõesA ICP de oclusão crónica total do TC após CABG pode ser bem-sucedida, segura, e pode fornecer melhorias clínicas mantidas em casos selecionados.
Chronic total occlusion (CTO) of the left main coronary artery (LMCA) is an infrequent finding on coronary angiograms. Its actual prevalence and incidence are unknown, although an incidence of 0.04% was reported in a large series.1,2
A more insidious clinical presentation, consisting of stable angina, unstable angina, and dyspnea, predominates in the presence of CTO of the LMCA, as opposed to acute lethal cardiac events resulting from acute thrombotic occlusion.1
With CTO of the LMCA comes a risk of major cardiovascular events, such as death from ischemic anterior myocardium, despite collateral circulation.2
Revascularization is recommended in the presence of demonstrated viability or ischemia in the area of the compromised perfused artery. Coronary artery bypass grafting (CABG) has long been considered the preferred option in this situation. Though limited evidence is available, promising results have been seen after percutaneous coronary intervention (PCI) using new-generation drug-eluting stents.2,3
Patients with a previous CABG due to LMCA disease with occlusion of one graft and progression of the LMCA to CTO constitute a special population, as just one ischemic artery remains (circumflex or left anterior descending artery), for which there is no other revascularization option other than cardiac surgery (requiring resternotomy) or PCI of the LMCA.
MethodsOut of 620 patients with CTO diagnosed in our center, we identified five with a previous CABG due to LMCA disease for a retrospective case series. They had occlusion of one graft and progression of the LMCA to CTO. All five underwent PCI. Each patient received a functional classification for angina, myocardial ischemic tests such as cardiac magnetic resonance imaging (cMRI), myocardial perfusion scintigraphy, and a follow-up coronary angiogram during a median follow-up of 63 months (range 16-118 months).
ResultsMedian age was 65 years (range 46-82 years), and all patients were male. All of them had at least three traditional cardiovascular risk factors and one had chronic renal disease (Tables 1 and 2).
Demographic/clinical characteristics.
| Case | Age | Gender | Angina grading scale | Hypertension | Chronic renal failure | Type 2 diabetes | Dyslipidemia | Smoker | Baseline LVEF | EuroSCORE II |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 48 | Male | III | Yes | No | Yes | Yes | Yes | 45% | 4.7% |
| 2 | 70 | Male | II | Yes | No | No | Yes | Yes | 40% | 6.7% |
| 3 | 46 | Male | II | Yes | No | Yes | Yes | Yes | 40% | 7.17% |
| 4 | 82 | Male | II | Yes | Yes | Yes | Yes | Yes | 30% | 34.39% |
| 5 | 72 | Male | II | Yes | No | Yes | Yes | Yes | 50% | 7.88% |
LVEF: left ventricular ejection fraction.
Coronary angiographic findings, myocardial ischemic tests performed and follow-up.
| Case | LIMA-LAD CABG | SVG-CX CABG | LRA-OM CABG | Myocardial ischemic tests (cMRI or cardiac SPECT) | Type of stent | Follow-up |
|---|---|---|---|---|---|---|
| 1 | Yes | No | Yes | Yes | Cypher | 118 months |
| 2 | Yes | Yes | No | Yes | Xience | 60 months |
| 3 | Yes | Yes | No | Yes | Xience | 58 months |
| 4 | Yes | Yes | No | Yes | Xience | 63 months |
| 5 | Yes | Yes | No | No | Xience | 16 months |
CABG: coronary artery bypass grafting; cMRI: cardiac magnetic resonance imaging; LIMA-LAD: left internal mammary artery-left anterior descending artery; LRA-OM: left radial artery-obtuse marginal artery; SPECT: single-photon emission computed tomography; SVG-CX: saphenous vein-circumflex coronary artery.
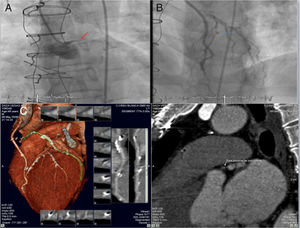
Three patients presented with new-onset crescendo angina reaching III/IV on the Canadian Cardiovascular Society (CCS) angina grading scale, and two had acute coronary syndrome (non-ST elevated myocardial infarction). The coronary angiogram showed CTO of the semi-protected LMCA lesions with two coronary artery bypass grafts previously performed in all patients, one occluded and the other patent (Figure 1). Three patients had saphenous vein grafts to the circumflex coronary artery that were CABG occluded and two patients had left internal mammary artery-left anterior descending artery CABG failure. A coronary CT angiography was performed in one patient to better visualize the CTO (Figure 1).
(A and B) Coronary angiogram showing chronic total occlusion of the left main coronary artery and critical left anterior descending lesion proximal to left internal mammary artery anastomosis; (C) coronary computed tomography angiography showing a short (9 mm), hardly calcified chronic total occlusion lesion: in the middle of the occlusion 100% of the coronary lumen (186 Hounsfield units) was calcified and, in the distal part, 75% of the wall circumference (933 Hounsfield units) was calcified.
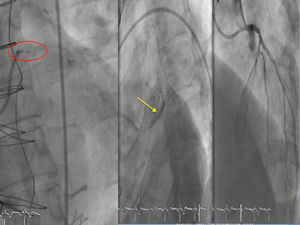
Severe left ventricular dysfunction (LVD) was found in one patient, and moderate LVD was found in three. Ischemia and viability were demonstrated in four patients by cMRI with adenosine (one patient) or perfusion scintigraphy (three patients). Surgery was ruled out either because of patient refusal or because of high surgical risk. Four patients with semi-protected lesions successfully underwent anterograde PCI of the LMCA with drug-eluting stents using the standard antegrade wire escalation technique (Figure 2). No debulking technique was used in patients with heavily calcified left main (LM) lesion. The retrograde technique was used in one patient through the septal channel. In this case, LM occlusion was located at the ostium.
In a five-year follow-up, four patients remained asymptomatic (CCS Grade I for angina and New York Heart Association Class I) and event-free (no major adverse cardiac events). Perfusion defects were not detected in repeat cMRIs with adenosine or perfusion scintigraphies, and no coronary disease progression was found at 63-month follow-up. Three patients experienced a 10% improvement in left ventricular ejection fraction.
Unfortunately, one death occurred 1.4 years post-PCI from non-cardiovascular cause (cancer).
DiscussionThe need for repeated interventional procedures in patients after CABG is determined by the durability of the bypass graft and progressive atherosclerosis of native coronary arteries. It has been assumed that changes in intracoronary circulation following the insertion of bypasses lead to the progression of native artery stenotic lesions to CTO.3
This case series is significant because this special population often suffers from refractory angina. Moreover, mortality is extremely high without intervention.3 Traditionally, a new surgical bypass approach was considered to be the treatment of choice for these patients. However, in daily practice, the high surgical risk profile resulting from multiple comorbidities and re-intervention commonly leaves PCI as the only feasible option.
With the advent of new drug-eluting stents and improvements in techniques, PCI can be a successful and safe procedure in this setting and can provide sustained clinical improvements, as observed in our small series.
AuthorshipAll authors had access to the data and played a role in writing this manuscript.
Conflicts of interestThe authors have no conflicts of interest to declare.