Ebstein anomaly is a congenital disease frequently associated with atrial septal defects, which can generate a right-to-left shunt, leading to systemic desaturation and right ventricular failure.
We describe the case of a 68-year-old man with central cyanosis due to Ebstein anomaly and a patent foramen ovale. An atrial septal occluder was initially implanted after having performed prolonged test occlusion of the interatrial communication. In this case, device embolization occurred due to high right pressure.
Percutaneous closure of atrial septal defects in the presence of a right-to-left shunt can offer a significant clinical improvement in selected cases. In patients with Ebstein anomaly, the implantation of atrial septal defect closure devices may be desirable, due to the larger size of the waist, which may provide better stability in the event of an increase in right pressure.
A anomalia de Ebstein é uma cardiopatia congénita complexa frequentemente associada a comunicação interauricular, com shunt direito-esquerdo, provocando desaturação sistémica e falência ventricular direita.
Apresentamos o caso de um doente de 68 anos, com cianose central devido a anomalia de Ebstein e Foramen ovale patente, em que foi implantado um dispositivo de encerramento de comunicação interauricular, após teste de oclusão de comunicação interauricular. Neste caso, utilizou-se inicialmente um dispositivo do encerramento do Foramenovale, que embolizou no contexto de pressões elevadas à direita.
O encerramento percutâneo das comunicações interauriculares na presença de shunt direito-esquerdo pode oferecer uma melhoria clínica significativa em casos selecionados. Em doentes com anomalia de Ebstein, a implantação de dispositivos de encerramento da comunicação interauricular pode ser preferível, devido às suas caracteríticas morfológicas, permitindo maior estabilidade contra o aumento de pressões à direita.
Ebstein anomaly (EA) is a rare congenital heart disease consisting of a low implantation of the tricuspid valve, with hypoplasia of the right ventricle and other anomalies such as pulmonary valve stenosis and ventricular preexcitation. Additionally, in 80-94% of patients, an atrial septal defect (ASD) is present and can generate a right-to-left shunt due to high pressure in the right cavities and tricuspid insufficiency. This shunt generates systemic desaturation; however, it also contributes to the right-side overload discharge enabling a hemodynamic balance in these patients. The percutaneous closure of these defects may contribute to improving systemic saturation, after having ensured that the right ventricle can tolerate the pressure increase.
Case reportWe present the case of a 68-year-old man with metastatic parotid carcinoma and central cyanosis (oxygen saturation of 75% at baseline with domiciliary oxygen therapy) with EA and a patent foramen oval (PFO). A previous transesophageal echocardiogram (TEE) described a severely dilated right ventricle with moderate systolic dysfunction and an atrial septal aneurysm check with a PFO generating a right-to-left shunt. Magnetic resonance imaging demonstrated an incompletely developed tricuspid septal leaflet, with a low implantation of the valve, moderate tricuspid insufficiency, and a PFO with a long membrane.
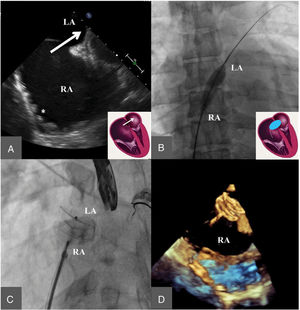
We planned the percutaneous closure of the PFO with transitory balloon occlusion to ensure accurate right ventricular tolerance of the PFO closure. Due to the clinical characteristics of the patient, with difficult intubation secondary to the parotid tumor, transthoracic echocardiogram (TTE) was used to motorize the procedure. After canalizing the right femoral vein and the right radial artery, pulmonary artery pressure was measured, ruling out significant pulmonary hypertension. Balloon occlusion of the PFO was then performed, maintaining an inflated 18 mm balloon for 10 minutes through the foramen. A significant improvement in peripheral oxygen saturation was observed, with good hemodynamic tolerance (Figure 1).
Initial closure of the defect using a cribriform patent foramen ovale (PFO) device. A: Transesophageal echocardiogram image where a PFO can be observed, with right-to-left shunt (arrow) and hypertrabeculation of the right atrium (RA) (ventricularization of the RA) (asterisk). B: Transitory occlusion test. C&D: Cribiform PFO closure device released at the PFO, radioscopy image (C) and three-dimensional transesophageal echocardiogram (D).
We then decided to perform the percutaneous closure of the PFO using a cribriform occluder. A 9 French sheath was placed in the left atrium and a 25 mm Amplatzer Multi-Fenestrated Septal Occluder - “Cribriform” (AGA Medical Corporation, Golden Valley, MN, USA) was advanced through the PFO, with good apposition of the discs before delivery.
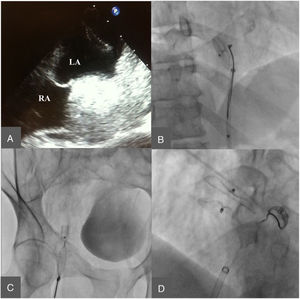
After release, the device was embolized into the left atrium and descending aorta. The right femoral artery was then canalized and the device was captured with a 30 mm gooseneck snare and externalized through the femoral artery. TEE was then performed under superficial sedation, showing an atrial septal aneurysm, with a wide PFO, and a large membrane distance generating an effective orifice of 18-20 mm. Finally, a 24 mm Amplatzer Septal Occluder (AGA Medical Corporation, Golden Valley, MN, USA) was implanted. Absence of shunt was confirmed via angiography and TTE before delivery (Figure 2). The procedure was concluded successfully and the patient was discharged the following day and prescribed treatment with 100 mg aspirin and 75 mg clopidogrel. In the following weeks there was a progressive improvement in his oxygen saturation, maintaining baseline levels over 90% and he was able to manage without domiciliary oxygen therapy.
Cribriform patent foramen ovale occluder embolization and extraction with final implant of the atrial septal defect (ASD) device. A: Transesophageal echography image where the device can be visualized with free movement at the left atrium. B: Device capture at the descending aorta. C: Device extraction through the right femoral artery. D: Final implant of the ASD device.
There are few publications on the percutaneous closure of ASD in patients with right-to-left shunt. The first reported cases were in pediatric patients, in whom a significant improvement in oxygen saturation and exercise tolerance was confirmed after percutaneous closure, even in the presence of a hypoplastic right ventricle.1,2
Jategoankar et al. described nine adults with EA and ASD defects, four of whom had right-to-left shunt and in whom a percutaneous closure of the defect was performed after a prolonged test occlusion of the interatrial communication at rest and under catecholamine stimulation.3 These authors recommended an exhaustive pre-procedure study of the patient, avoiding the closure of the defect in the presence of severe tricuspid regurgitation or pulmonary hypertension. In this series, two of the nine patients presented a PFO, which was closed using ASD devices.
Silva et al. described nine cases of EA with right-to-left shunt, in which temporary test occlusion was performed before the percutaneous closure, resulting in a significant improvement in oxygen saturation and functional capacity in all cases; mean follow-up was of five years.4
In this kind of patient, the anatomy of the interatrial septum must be analyzed exhaustively to select the appropriate device. Given the high right pressure, the PFO can present a large inter-membrane defect, generating large effective orifices, which should preferably be occluded using ASD defect devices. In this case, the TEE was initially avoided due to the high risk associated with intubation and the previous TEE; an intracardiac echo would have been very useful in this patient. In the reported cases, ASD devices are only occasionally used for PFO closures. The design of the ASD occluders, with longer discs and a wider waist, may also provide better stability against an increase in right pressure after the procedure.
ConclusionPercutaneous closure of ASD in the presence of a right-to-left shunt can offer significant clinical improvement in selected cases. In these patients, a balloon occlusion test is essential to evaluate the individual response to the ASD closure and to guarantee procedure safety. Additionally, the anatomy of the interatrial septum must be exhaustively analyzed to select the appropriate device for each case. The implantation of an ASD closure device may be desirable over the PFO devices in this kind of patients due to their design, characterized by longer disc length which may provide better stability against an increase in right pressure after the procedure.
Conflicts of interestThe authors have no conflicts of interest to declare.