Diabetes, a metabolic disease with vascular consequences due to accelerated atherosclerosis, is one of the 21st century's most prevalent chronic diseases. Characterized by inability to produce or use insulin, leading to hyperglycemia and insulin deficiency, diabetes causes a variety of microvascular (such as retinopathy and kidney disease) and macrovascular complications (including myocardial infarction and stroke) which reduce the quality of life and life expectancy of individuals with diabetes.
We describe the close relationship between diabetes, cardiovascular risk factors, and cardiovascular disease, and examine multifactorial approaches to diabetes treatment, including reducing cardiovascular risk in individuals with type 2 diabetes. Finally, we analyze new prospects for the treatment of type 2 diabetes, resulting from the development of novel antidiabetic drugs.
The aim of this review is that the clinician should assume the crucial role of guiding individuals with diabetes in the control of their disease, in order to improve their quality of life and prognosis. In view of the currently available evidence, the emergence of new glucose-reducing therapies with proven cardiovascular benefit means that the best therapeutic strategy for diabetes must go beyond reducing hyperglycemia and aim to reduce cardiovascular risk.
A diabetes mellitus (DM) é uma das patologias crónicas mais prevalentes no século XXI, constituindo uma doença metabólica com consequências vasculares por aceleração dos processos ateroscleróticos. Caracterizada pela incapacidade de produção ou utilização de insulina, e consequente hiperglicemia e insulinopenia, a DM ocasiona diversas complicações microvasculares, tais como retinopatia e nefropatia, e macrovasculares, incluindo enfarte agudo do miocárdio e acidente vascular cerebral, as quais põem em causa a qualidade e expectativa de vida da pessoa com diabetes. Descrevemos a estreita relação entre DM, fatores de risco cardiovascular e doença cardiovascular e examinamos a abordagem multifatorial para o tratamento dessa doença, incluindo a redução do risco cardiovascular na pessoa com DM tipo 2 (DM2). Por último, analisamos novas perspetivas para o tratamento da DM2, resultantes do desenvolvimento de novos fármacos antidiabéticos. Com esta revisão pretende-se que o clínico assuma o papel fundamental de orientar a pessoa com diabetes no controlo da sua doença, com vista a melhorar a sua qualidade de vida e o seu prognóstico. Tendo em conta os dados disponíveis atualmente, o aparecimento de novas terapêuticas anti-hiperglicémicas com comprovado benefício cardiovascular obriga a que a melhor estratégia terapêutica para a DM ultrapasse a redução da hiperglicemia e considere necessariamente a redução do risco cardiovascular.
Action to Control Cardiovascular Risk in Diabetes
Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified Release Controlled Evaluation
cardiovascular disease
cardiovascular outcomes trials
Diabetes Control and Complications Trial
dipeptidyl-peptidase 4
Food and Drug Administration
glucagon-like peptide 1
glycated hemoglobin
International Diabetes Federation
low-density lipoprotein
myocardial infarction
Portuguese National Diabetes Observatory
C-reactive protein
sodium-glucose cotransporter-2
UK Prospective Diabetes Study
Veterans Affairs Diabetes Trial
Diabetes is a metabolic disease with vascular consequences due to accelerated atherosclerosis that is characterized by inability to produce or use insulin, leading to hyperglycemia and insulin deficiency. Diabetes causes a variety of microvascular (such as retinopathy, kidney disease and neuropathy) and macrovascular complications (including myocardial infarction [MI], stroke and peripheral arterial disease.1–4
The International Diabetes Federation (IDF) reports that some 415 million adults between the ages of 20 and 79 years had diabetes in 2015, and predicts that this will rise to 642 million by 2040.2 The prevalence of diabetes in Portugal in adults aged 20-79 years (7.7 million individuals) was estimated in 2015 at 13.3%,4 around one in 10 adults and corresponding to over a million Portuguese. According to the Portuguese National Diabetes Observatory (OND), in 2015 the prevalence of diabetes had increased by 13.5% since 2009, and its incidence had also risen markedly in the previous four years, with estimates ranging from 591.5 to 699.5 new cases per 100000 individuals. This implies that in 2015 there were 61169-87234 new cases of diabetes.4
In 2012, diabetes was the direct cause of 1.5 million deaths worldwide,5 making it the sixth leading cause of death, while in 2015 it contributed to five million deaths.3 Given that certification of death from diabetes is frequently imprecise, various studies have shown that diabetes is probably the direct cause of 10-15% of all deaths.6,7
Cardiovascular disease (CVD) is the leading cause of diabetes-related death; over 70% of patients with type 2 diabetes die of CVD. As a consequence, the diabetes epidemic will be followed by an epidemic of CVD attributable to diabetes that may reverse the current decline in cardiovascular mortality in countries like Portugal.8,9
CVD is also the leading cause of hospital admission in diabetic individuals. In 2015, the main causes of hospitalization for more than 24 hours in diabetic individuals in Portugal were diseases of the circulatory system (26%), followed by respiratory disease (15%) and diseases of the digestive system (10%).4 Some 24% of hospitalizations for decompensation or complications of diabetes were due to alterations in peripheral circulation.4 Furthermore, OND data show that diabetic patients accounted for 29.5% of admissions for stroke and 32.4% of admissions for MI, and that mortality in diabetic patients suffering MI was higher than overall mortality from MI (8.3% vs. 7.6%).4
The above data depict an increasing burden from diabetes in our society, not only due to the number of people affected, but also because these people will have a greater likelihood of suffering an atherosclerotic cardiovascular event, which is the leading cause of hospitalization and mortality in individuals with diabetes.1,10–12
The close relationship between diabetes and CVD means that the clinician should assume the crucial role of guiding individuals with diabetes in the prevention and control of their disease, in order to improve their quality of life and prognosis.
Diabetes, cardiovascular risk factors and cardiovascular diseaseDiabetes has long been recognized as an independent risk factor for CVD, with various landmark studies such as the Framingham study11,12 documenting increased cardiovascular risk in diabetic patients. Studies recently analyzed by the IDF3 show that diabetic individuals have a greater risk of ischemic heart disease, cerebrovascular disease, peripheral vascular disease and CVD-related mortality. The increase in risk ranges from 1.7 to 4.5 in men and from 1.8 to 9.5 in women compared to men and women without diabetes.3,13–15
The greater cardiovascular risk in diabetic individuals leads to a high prevalence of CVD in this population, ranging from 14.8% to 40.5% between the ages of 55 and 66 years. The prevalence of ischemic heart disease in diabetic individuals was between 12.0% and 31.7% in studies of populations with mean ages between 51 and 69 years, while the prevalence of stroke was between 3.5% and 10.4% in populations with mean ages between 53 and 67 years.3
In view of the potential impact of CVD on the quality of life and life expectancy of individuals with diabetes, the clinical approach to the individual with diabetes should aim to control all cardiovascular risk factors, several of which, including obesity, sedentary lifestyle, dyslipidemia and hypertension, are more frequent in diabetic people, especially those with type 2 diabetes, than in the general population.3,16,21 The therapeutic goals for blood pressure and low-density lipoprotein cholesterol (LDL-C) are stricter in patients with diabetes.17 However, control of risk factors is frequently worse in diabetic than in non-diabetic patients. For example, the EUROASPIRE IV survey showed that only 54% of coronary patients diagnosed with diabetes had blood pressure <140/90 mmHg, as opposed to 68% of non-diabetic patients,18 while in the PINNACLE registry only 61.6% of those with diabetes aged 40-75 years without known CVD were taking a statin.19
It has been shown that various pathophysiological factors involved in the development of type 2 diabetes, including oxidative stress, vascular inflammation and endothelial dysfunction, may also contribute directly to the development of CVD.16,20,21
Patients with type 2 diabetes have greater atherosclerotic plaque burden and atheroma volume and smaller coronary artery luminal diameter than non-diabetic individuals.22 Coronary atherosclerosis is common in type 2 diabetes even in primary prevention, when there are no clinical manifestations of myocardial ischemia. In a study of 591 individuals with asymptomatic type 2 diabetes who underwent coronary computed tomography angiography, non-obstructive lesions (<50% stenosis) were found in 31.6% of cases, and only 28.4% were classified as having normal coronaries.23 The presence of obstructive coronary disease in this study was associated with worse prognosis, including higher rates of cardiac death, MI, unstable angina and coronary revascularization.23 In a 1980 study of asymptomatic diabetic patients with normal electrocardiogram who underwent myocardial perfusion scintigraphy, silent myocardial ischemia was identified in 27% of cases.24
There is a linear relationship between glycated hemoglobin (HbA1c) levels and macrovascular disease. Growing evidence from epidemiological studies supports the link between dysglycemia and risk of CVD, with risk of a cardiovascular event rising by 11-16% for every 1% increase in HbA1c.25 Data from the Swedish National Diabetes Register on over 18000 patients followed for more than five years show clearly that the risk of coronary artery disease, stroke and total mortality rises in parallel with HbA1c levels and that the risk is reduced when HbA1c is <7%.26
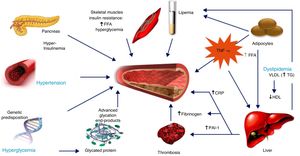
The increased cardiovascular risk in diabetic individuals is due to multiple factors, including hyperglycemia, insulin resistance or hyperinsulinemia, dyslipidemia, inflammation, oxidative stress, endothelial dysfunction, hypercoagulability and vascular calcification (Figure 1).16,20,21 Insulin resistance, both systemic and vascular, is associated with a higher incidence of hypertension and dyslipidemia, as well as with reduced glucose tolerance, promoting atherosclerotic processes and hence the development of CVD.25,27 In individuals with type 2 diabetes, insulin resistance is also associated with higher plasma free fatty acid levels, leading to hepatic overproduction of glucose and insulin, as well as increased triglyceride reserves.16,20 The increased triglyceride levels induced by insulin resistance link diabetes to increased risk for atherogenic dyslipidemia, another risk factor shared by type 2 diabetes and CVD.1,3
Factors contributing to raised cardiovascular risk in type 2 diabetes (adapted from Libby and Plutzky62). CRP: C-reactive protein; FFA: free fatty acids; HDL: high-density lipoprotein; LDL: low-density lipoprotein; PAI-1: plasminogen activator inhibitor-1; TG: triglycerides; TNF-α: tumor necrosis factor alpha; VLDL: very low-density lipoprotein.
Increased levels of inflammatory markers and mediators such as C-reactive protein (CRP) and interleukin-6 are associated with heightened risk of cardiovascular events. Various studies have established a link between these mediators, showing that increased levels of interleukin-1 and -6 and CRP are predictors of progression of type 2 diabetes, which could in fact be defined as a form of chronic autoinflammatory disease, due to the upregulation of interleukin-1 beta by beta cells of the pancreatic islets, leading to beta cell apoptosis.28
Endothelial dysfunction leads to platelet and leukocyte adhesion, thrombosis and inflammation. In the presence of elevated glucose levels, the bioavailability of nitric oxide (NO) is reduced, impairing vasodilation. Conversely, reduced NO synthase activity and hence diminished NO production are seen in insulin resistance and diabetes, leading to endothelial dysfunction.25 There is also evidence that hyperinsulinemia and hyperglycemia increase circulating tissue factor levels, which would explain the higher thrombotic risk in diabetic individuals.29
Hyperglycemia also accelerates vascular calcification. Individuals with diabetes have higher coronary calcium scores than those without and are thus at greater risk for recurrent atherothrombosis.26
In view of the above, there is now agreement that the approach to type 2 diabetes must go beyond reducing hyperglycemia and aim to reduce cardiovascular risk. The aim of this review is to examine approaches to treating type 2 diabetes in the light of recent evidence.
Reducing cardiovascular risk in individuals with type 2 diabetesReducing blood glucose levels is crucial in individuals with type 2 diabetes, firstly because it is fundamental to reducing the impact of the small-vessel disease known as diabetic microangiopathy, and secondly because if not controlled, hyperglycemia is associated with increased cardiovascular risk and cardiovascular mortality.30 With the publication of the UK Prospective Diabetes Study (UKPDS) and the Diabetes Control and Complications Trial, it was recognized that intensive glycemic control therapy reduced the occurrence of cardiovascular events. However, although such therapy had been clearly shown to reduce microvascular complications, its benefits were less clear in relation to macrovascular complications.30–35
Three trials have been designed to test whether maintaining HbA1c below 6.5% leads to cardiovascular benefit: Action to Control Cardiovascular Risk in Diabetes (ACCORD),32 the Veterans Affairs Diabetes Trial (VADT),34 and Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified-Release Controlled Evaluation (ADVANCE). These trials failed to show that more intensive glycemic control reduced cardiovascular events in patients with established type 2 diabetes (mean duration more than 10 years).32,34 On the other hand, 10-year results of the UKPDS showed that blood glucose control reduced the long-term incidence of macrovascular complications and mortality in patients with newly diagnosed type 2 diabetes,31,33 although this effect was only observed after a mean follow-up of over 15 years.31 Similarly, follow-up of the VADT trial revealed long-term cardiovascular benefit.35 By contrast, increased long-term mortality was seen in the ACCORD trial.
Various explanations have been put forward to explain these differences in results, particularly that the cardiovascular benefits of intensive glycemic control focused on insulin use may be outweighed by associated adverse effects, including weight gain and hypoglycemic attacks.21,30,36 Another recently published explanation for the higher event rate in the intensive treatment arm of the ACCORD trial is the presence of two genetic variants that predicted cardiovascular risk: one within intron 1 of the MGMT (O-6-methylguanine-DNA methyltransferase) gene and the other upstream and proximal to three long intergenic noncoding RNAs (LINC1335, LINC1333, and LINC1331).37 Yet another hypothesis, which is more generally accepted, is that of the metabolic memory effect: after years of poor metabolic control it becomes difficult or even impossible to reverse the atherosclerotic process.38,39
Other studies have shown that certain antidiabetic drugs induce effects that can worsen cardiovascular risk, such as fluid retention in the case of the glitazones.40,41 At the same time, studies of multifactorial intervention such as the Steno-2 Study have shown that management of CVD in patients with type 2 diabetes consisting of treatment targeting hyperglycemia, hypertension and dyslipidemia, together with antiplatelet therapy, significantly reduces mortality.42
A multifactorial approach in fact appears to be the most appropriate strategy in diabetes. Current evidence indicates that lifestyle modification brings some benefit,17,30,44–46 while intensive glycemic control (keeping HbA1c below 6.5%) reduces microvascular complications and cardiovascular risk in patients with type 2 diabetes, except in the elderly, those with established CVD and other sensitive populations.17,43,45,46 Blood pressure control, in particular ensuring that systolic blood pressure does not exceed 130-140 mmHg,17,21,43 further reduces micro- and macrovascular complications such as stroke, retinopathy and albuminuria.17,47 Improvements in lipid profile are essential for reducing cardiovascular risk, and strict lipid-lowering therapy is recommended for patients with type 2 diabetes in order to keep LDL-C levels below 100 mg/dl (70 mg/dl for very high risk patients),48 and the use of lipid-lowering agents should be considered for patients aged under 40 years.3,17 In individuals with diabetes and hypertriglyceridemia, the guidelines recommend that non-high-density lipoprotein cholesterol levels be kept less than 30 mg/dl above the maximum recommended LDL-C level.17
These findings show that multifactorial intervention together with lifestyle modification can improve outcomes in individuals with type 2 diabetes.10 A Swedish study of 457473 individuals with type 2 diabetes over a median of 15 years of observation showed significant falls in cardiovascular outcomes and mortality over the study period.10 According to the authors, increasing emphasis on integrated care of patients with chronic disease, improved patient education in disease management, and advancements in clinical decision-making support have probably reduced the rates of cardiovascular complications among patients with diabetes.10 Advances in revascularization for coronary disease and increased use of glucose self-monitoring systems may also have played a role in improving the outlook for individuals with diabetes.10 Finally, the authors also attribute the substantial cardiovascular risk reduction seen in their study to improved management of risk factors such as hypertension, elevated LDL-C and HbA1c levels, and macroalbuminuria, associated with higher frequency of treatment with statins and antihypertensive medications. Recent studies have shown that larger reductions in cholesterol levels using ezetimibe or proprotein convertase subtilisin/kexin type 9 (PCSK9) are associated with reductions in cardiovascular events in patients with diabetes.17,43,45 The Steno-2 Study, in a follow-up of over 20 years, also demonstrated that an intensive multifactorial approach increased life expectancy in diabetic individuals by 7.9 years.42,49
When aiming to improve the cardiovascular prognosis of individuals with diabetes, the approach should always be personalized. However, there is strong evidence that management beyond glycemic control with multifactorial treatment, intensive in most patients, leads to better outcomes not only from a metabolic standpoint but also by preventing micro- and macrovascular complications.
Novel antidiabetic drugs: new prospects in the treatment of diabetesThe above data make it clear that treatment of individuals with type 2 diabetes should take into account the importance of reducing atherosclerotic cardiovascular events. The cardiovascular safety of antidiabetic drugs has therefore assumed even more importance than their effectiveness for glycemic control. Several reviews of the literature on these drugs have been published in recent years, detailing their cardiovascular risks and benefits,21,40,41,45,50–52 and there is evidence of a change in attitude among those developing new drugs to treat diabetes. Since reports emerged of a possible association between rosiglitazone and increased rates of cardiovascular events,40,41 the cardiovascular safety of such drugs has become a determining factor in the approval process. As of 2008, the US Food and Drug Administration (FDA) and the European Medicines Agency require evidence in the form of randomized clinical trials that new glucose-lowering drugs are not associated with an increase in cardiovascular risk in patients with type 2 diabetes.30,40,41 Cardiovascular outcomes trials (CVOTs) analyze safety in terms of major adverse cardiovascular events (MACE), usually with a primary composite outcome of cardiovascular death, non-fatal MI and non-fatal stroke. Some recent trials of new drugs – two glucagon-like peptide 1 (GLP-1) receptor agonists and two sodium-glucose cotransporter-2 (SGLT-2) inhibitors – have demonstrated superior cardiovascular efficacy as well as safety.21,30,41
Table 1 summarizes the results of the main CVOTs. Although these trials have in general demonstrated the non-inferiority of the novel antidiabetic drugs in terms of cardiovascular safety, not all have shown significant reductions in MI, cerebrovascular disease or cardiovascular mortality.21,40,41 The trials on the dipeptidyl peptidase 4 (DPP-4) inhibitors saxagliptin (SAVOR-TIMI 53),49 alogliptin (EXAMINE),53,54 and sitagliptin (TECOS),55 and on the GLP-1 receptor agonists lixisenatide (ELIXA)46 and extended-release exenatide (EXSCEL),56,57 did not show these drugs to be superior in reducing the primary outcome; although the trials varied in methodology, no significant differences in MACE were found between their treatment and control arms.
Summary of some of the main cardiovascular outcomes trials in patients with type 2 diabetes.
| Trial | Drug | Drug class | CV outcome | Individuals with type 2 diabetes | Mean follow-up (years) | Reference |
|---|---|---|---|---|---|---|
| SAVOR-TIMI 53 | Saxagliptin | DPP-4i | ≈ CV death, NF MI or NF stroke≈ CV death≈ NF MI≈ NF stroke | ≥40 years, with CVD or very high CV risk | 2.1 | 48 |
| EXAMINE | Alogliptin | DPP-4i | ≈ CV death, NF MI or NF stroke≈ CV death≈ NF MI≈ NF stroke | ≥18 years, ACS 15-90 days before | 1.5 | 54, 55 |
| TECOS | Sitagliptin | DPP-4i | ≈ CV death, NF MI, UA or NF stroke≈ CV death≈ NF MI≈ NF stroke | ≥50 years, with CVD | 3 | 56 |
| ELIXA | Lixisenatide | GLP-1ra | ≈ CV death, NF MI, UA or NF stroke≈ CV death≈ NF MI≈ NF stroke | ≥30 years, ACS in previous 180 days | 2.1 | 47 |
| LEADER | Liraglutide | GLP-1ra | ↘ CV death, NF MI or NF stroke↘ CV death↘ NF MI↘ NF stroke | ≥50 years, with CVD or HF≥60 years, very high CV risk | 3.8 | 49 |
| SUSTAIN-6 | Semaglutide | GLP-1ra | ↘ CV death, NF MI or NF stroke≈ CV death≈ NF MI↘ NF stroke | ≥50 years, with CVD≥60 years, pre-CVD | 1.99 | 64 |
| EXSCEL | Exenatide ER | GLP-1ra | ≈ CV death, NF MI or NF stroke≈ CV death≈ NF MI≈ NF stroke | ≥18 years, with any degree of CV risk | 3.2 | 58 |
| EMPA-REG OUTCOME | Empagliflozin | SGLT-2i | ↘ CV death, NF MI or NF stroke↘ CV death≈ NF MI≈ NF stroke | ≥18 years, with CVD | 3.1 | 59 |
| CANVAS | Canagliflozin | SGLT-2i | ↘ CV death, NF MI or NF stroke≈ CV death≈ NF MI≈ NF stroke | ≥30 years, with CVD≥50 years, with very high CV risk | 2.33 | 60 |
Adapted from Schnell et al.40
↘ significant reduction; ≈ non-significant effect; ACS: acute coronary syndrome; CV: cardiovascular; DPP-4i: dipeptidyl peptidase-4 inhibitor; ER: extended release; GLP-1ra: glucagon-like peptide 1 receptor agonist; HF: heart failure; MI: myocardial infarction; NF: non-fatal; SGLT-2i: sodium-glucose cotransporter-2 inhibitor; UA: unstable angina.
The pragmatic EXSCEL trial, the results of which were recently published,56,57 was carried out in a heterogeneous population that was close to that of real-world clinical practice, unlike those usually found in clinical trials. Furthermore, due to the complexity of the injection device used, 43% of subjects randomized to the exenatide treatment arm discontinued the trial regimen. In SAVOR-TIMI 53,47 the use of saxagliptin was associated with increased hospitalization for heart failure in patients with and without prior heart failure or renal failure, but there was no increase in mortality or the primary composite outcome.
On the other hand, other CVOTs have shown the superiority of two GLP-1 receptor agonists – liraglutide in the LEADER trial48 and semaglutide (approved by the FDA) in SUSTAIN-663 – and two SGLT-2 inhibitors, empagliflozin in the EMPA-REG OUTCOME trial58 and canagliflozin (for cardiovascular risk reduction) in CANVAS.59 These four antidiabetic drugs led to significant reductions in the incidence of MACE in patients with type 2 diabetes, most of whom had established CVD (Table 1). Current evidence demonstrates that the cardiovascular benefit of these drugs cannot be taken to be a class effect, given the conflicting results of these trials and the differences between the properties of the individual molecules.60 For example, since it was shown to reduce cardiovascular mortality and non-fatal MI and stroke while having a neutral effect on heart failure, liraglutide may act through mechanisms that slow the atherosclerotic process, providing direct protection against cardiovascular events.50,60
Differences between CVOTs should be taken into consideration when analyzing their results. Regarding the drugs themselves, although all four are GLP-1 receptor agonists, liraglutide and semaglutide are derived from human GLP-1, whereas lixisenatide and exenatide are derived from reptilian exendin-4; while from a pharmacokinetic standpoint, lixisenatide is short-acting, unlike liraglutide, exenatide and semaglutide. In addition, confounding factors affect comparisons between the trials, such as the 40% discontinuation rate in EXSCEL, much higher than in the other trials. Furthermore, in the placebo arm of the EXSCEL trial, 3.6% of patients received GLP-1 receptor agonists and 9.4% received SGLT-2 inhibitors, compared to 2.5% and 6.5%, respectively, in the exenatide arm, which may have masked the effect of the drug under study. It should also be borne in mind that in the CVOTs on the different GLP-1 receptor agonists, the proportion of subjects receiving secondary prevention therapy varied considerably.
Empagliflozin may have a different mechanism of action from that of liraglutide, since it reduces cardiovascular mortality (apparently by reducing heart failure) but not MI or stroke. This may be explained by its pleiotropic effects on cardiovascular risk factors, its diuretic, natriuretic and hemodynamic effects, and possibly by direct action on the circulatory apparatus.50,60 The rapid benefit from empagliflozin (in a matter of weeks) implies that it does not have significant effects on the atherosclerotic process, unlike what is suggested in the literature for liraglutide, but is superior to the latter drug in reducing cardiovascular mortality.50,60 Recently published results of the CANVAS trials on canagliflozin indicate that this drug significantly reduced the incidence of the primary composite outcome of death from cardiovascular causes, non-fatal MI, or non-fatal stroke, but not of these events separately (Table 1). They also reported an increased risk for amputation of toes, feet, or legs; the highest absolute risk was in patients with peripheral arterial disease or a history of amputation, but the risk was also independently associated with the drug.59
The World Health Organization and other international and national bodies, including the Portuguese Society of Diabetology,3,43–45,61 have stressed the need for more data concerning the cardiovascular benefits of other DPP-4 inhibitors, GLP-1 receptor agonists and SGLT-2 inhibitors. The final results of CVOTs on the new DPP-4 inhibitor linagliptin (CARMELINA and CAROLINA), the GLP-1 receptor agonist dulaglutide (REWIND), and the SGLT-2 inhibitor dapagliflozin (DECLARE-TIMI), are therefore eagerly awaited.
In view of the currently available evidence, we suggest that clinical decisions regarding treatment of type 2 diabetes should be based on the effects of the different antidiabetic drugs, taking into account their risks and benefits in the light of the latest results of the relevant CVOTs (Table 2). Particular drug associations, such as empagliflozin with liraglutide, may be of greater value for patients with type 2 diabetes and very high cardiovascular risk. The current guidelines of the American Diabetes Association recommend these two drugs for patients with pre-existing CVD,43 while the European Society of Cardiology recommends SGLT-2 inhibitors, particularly empagliflozin, for diabetic patients with CVD and for those with heart failure.17
Risks and benefits of antidiabetic drugs.
| Metformin | Sulfonylureas | Pioglitazone | DPP-4i | GLP-1ra | SGLT-2i | |
|---|---|---|---|---|---|---|
| Glycemic efficacy | +++ | +++ | +++ | ++ | +++ | ++ |
| Risk of hypoglycemia | Neutral | Moderate/severe | Neutral | Neutral | Neutral | Neutral |
| Body weight | Loss/neutral | Gain | Gain | Neutral | Loss | Loss |
| Significant effects | ||||||
| Overall CV safety | Neutral | Neutral (gliclazide, glimepiride) | NeutralMay reduce risk of stroke | Neutral | Benefit (liraglutide, semaglutide) | Benefit (empagliflozin, canagliflozin) |
| Chronic HF | Neutral | Increased risk | Increased risk | Neutral/possible risk (saxagliptin and alogliptin) | Neutral | Benefit (empagliflozin, canagliflozin) |
| Renal function | Contraindicated in renal failure if eGFR <30 ml/min/1.73 m2 | Increased risk of hypoglycemia | Dose adjustments advisable with renal dysfunction (except linagliptin); reduction of albuminuria | Exenatide not indicated if creatinine clearance <45 ml/min/1.73 m2; possible benefit (liraglutide) | Not indicated if eGFR <45 ml/min/1.73 m2 (canagliflozin) or <60 ml/min/1.73 m2 (dapagliflozin); possible benefit (empagliflozin) | |
| GI | Side effects | Side effects | ||||
| Orthopedic | Increased risk of fracture | Amputations in lower limbs (canagliflozin)Fractures (canagliflozin) | ||||
| Other | Lactic acidosis | Acute pancreatitis | Euglycemic ketoacidosis, UTI |
Adapted from Xu et al.41 and Garber et al.45
CV: cardiovascular; DPP-4i: dipeptidyl peptidase-4 inhibitors; eGFR: estimated glomerular filtration rate; GI: gastrointestinal; GLP-1ra: glucagon-like peptide 1 receptor agonists; HF: heart failure; SGLT-2i: sodium-glucose cotransporter-2 inhibitors; UTI: urinary tract infection.
Advances in medicine lead to ever deeper understanding of many diseases. Research into diabetes has seen many developments, especially in the last 20 years, during which the clinical picture of the condition has changed from being purely glycocentric to one requiring a multifactorial metabolic approach that reflects the complexity of the disease.
While diabetes is among the most prevalent diseases of the 21st century, CVD remains the leading cause of death in Portugal, particularly in individuals with diabetes. The pathophysiological relationship between the two conditions is clear and it is thus essential to take especial care with the approach to the diabetic patient. Furthermore, both the literature and clinical experience dictate that treatment should be individualized to each patient. The new paradigm for treatment of type 2 diabetes is to choose drugs according to the patient's characteristics, with CVD risk being a paramount consideration. Although glycemic control is essential, the best strategy to reduce cardiovascular risk in individuals with type 2 diabetes is multifactorial, and the physician must pay close attention to other risk factors. When lifestyle modification, the initial step in diabetes treatment, is inadequate, there is now strong evidence that the mechanisms of action of certain antidiabetic drugs provide additional benefits.
Glycemic control must be effective without risking hypoglycemia and without exacerbating other cardiometabolic risk factors, in order to reduce diabetes-related cardiovascular morbidity and mortality. The emergence of new glucose-reducing drugs with proven ability to reduce cardiovascular events is thus of particular importance in the treatment of individuals with type 2 diabetes.
The possibility, today within reach, of managing diabetes by effective glycemic control and thus reducing its impact on quality of life and the incidence of cardiovascular and cerebrovascular events, offers the prospect of a near future in which the burden of this disease on society may be significantly diminished.
FundingNovo Nordisk funded medical writing services for this article, provided by Scientific ToolBox Consulting. The positions expressed in this paper are those of the authors and do not necessarily reflect those of Novo Nordisk.
Conflicts of interestThe authors declare the following potential conflicts of interest: Carlos Aguiar has received honoraria for consulting from AstraZeneca, Boehringer Ingelheim, Novo Nordisk and Tecnimede; Rui Duarte has received honoraria for speaking and consulting and has served as a member of advisory boards or received training or research grants from Abbott, AstraZeneca, Boehringer Ingelheim, Lilly, Medinfar, MSD, Novartis, Novo Nordisk, Sanofi and Tecnimede; and Davide Carvalho has received honoraria for speaking and consulting and has served as a member of advisory boards for AstraZeneca, Bial, Boehringer Ingelheim, Lilly, Merck Serono, MSD, Novartis, Novo Nordisk, Sanofi and Servier.
Please cite this article as: Aguiar C, Duarte R, Carvalho D. Nova abordagem para o tratamento da diabetes: da glicemia à doença cardiovascular. Rev Port Cardiol. 2019;38:53–63.





 CRP: C-reactive protein; FFA: free fatty acids; HDL: high-density lipoprotein;
CRP: C-reactive protein; FFA: free fatty acids; HDL: high-density lipoprotein; 

