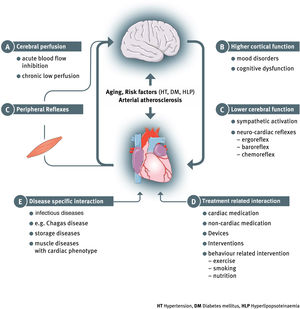
Heart failure (HF) has evolved from the classic understanding of a mere hemodynamic (pumping) failure, to a far more complex clinical syndrome. We know today that multiple organs and body systems are involved in the clinical presentation, progression and prognosis of HF. This evolution results not only from advanced scientific insight and clinical understanding of the disease, but also from factors such as improved medical care for acute cardiac events and an ageing society. Together this leads to a higher prevalence of the disease and greater longevity for patients with HF. Heart failure is particularly prevalent among the elderly; the mean patient age at initial diagnosis of HF is >70 years. Various morbidities can accumulate over life and HF patients often present with multiple comorbidities. These, however, often interact and exacerbate HF (such as arteriosclerosis, kidney impairment, chronic obstructive pulmonary disease, diabetes mellitus, muscle wasting, anemia and others) and contribute to the presentation of HF as a complex systemic clinical syndrome. Among the various heart-organ interactions in HF, prominence should be given to brain disorders due to the brain's central role in our biological and mental wellbeing. In fact, the heart and the brain are very closely connected via multiple and bidirectional links which form the basis for the concept of a “cerebral-cardiac syndrome” in HF.1 While stroke, cognitive decline, depression, anxiety or abnormal central reflexes derive from distinct aspects of cerebral function, they can all be seen as components of the global heart-brain interaction in HF. An integrated view of these multifaceted afferent and efferent links between the brain and the heart and the vascular system will be required for a deeper understanding of the significance of cerebral involvement in symptoms, progression and mortality in HF. Such an overview and taxonomy of heart-brain interactions was recently presented by the Heart Failure Association of the European Society of Cardiology (ESC) [Figure 1].2
Relevance of higher cerebral functions in heart failureHigher cognitive function and the psychological aspects of HF are increasingly in the focus of clinical studies. Despite the understanding of their impact on quality of life and on outcome, there is a paucity of therapeutic options. Cognitive impairment is common in HF syndromes with an estimated prevalence of 25%-75%.3,4 Yet, an even higher prevalence may be assumed as many cases are not recognized.5 Cognitive impairment is associated with a loss of independence, and a significantly impaired quality of life, lower treatment adherence and a worse prognosis.6 Many aspects of cognitive decline are still not fully understood. The early detection of subtle decline in cognitive function and the course of these injuries may be challenging targets.
In this issue, Rigueira et al. report on a prospective longitudinal study to address these issues in a single center cohort of patients after hospital admission for an acute event of HF decompensation.7 The authors observed that a six-fold higher risk of HF readmission is associated with cognitive injury, as assessed by the Montreal Cognitive Assessment. Moreover, in the follow up of these patients, recovery of cognitive performance is minimal at best. The latter remains an aspect of ongoing debate as previous studies reported recovery of cognitive function after acute episodes of HF decompensation, as well as little change or even a continued decrease in cognitive function in HF patients over time. This may underscore the diversity of disease course in individual cases and also highlight the need for careful, continued individual monitoring of cognitive function in patients with HF during long-term ambulatory care.
The authors further assessed depression and anxiety in their study and observed, in line with previous studies, a high prevalence of these psychological disorders. Depression in HF is common and is associated with poor quality of life, lower treatment adherence and self-care efforts, greater morbidity and mortality, increased hospitalization and higher health care costs.8,9 The prevalence of major depression is 20-40% in patients with HF, which is about four to five times higher than in the general population.10 The risk of depression increases with age, with advancing HF severity and is higher in women. Notably, despite the known significant impact of depression in HF, it remains an underdiagnosed aspect of HF syndrome.11 Early depressive symptoms, especially, may be overlooked in the routine care of HF patients. Current ESC guidelines on HF advise routine screening of HF patients for depression both during hospitalization and follow-up. Comprehensive care concepts to monitor changes in depression should include family members to ensure early recognition.
Therapeutic concepts to target depression and anxiety in HF remain a challenge despite the clear understanding of the significance of these mental disorders. The use of a range of antidepressant medications may be limited due to unfavorable effects on blood pressure or pro-arrhythmic potential.11 Two randomized controlled trials administered selective serotonin reuptake inhibitors which appear to be safe in HF (SADHART-CHF and MOOD-HF).12,13 These studies did not demonstrate superiority over placebo in reducing depressive symptoms in patients with HF in the short- and long-term. Therefore, non-pharmacological therapy, such as exercise training and cognitive behavioral therapy may be relevant options in HF, although their sustainability in long-term clinical practice is unknown.14
Key messageThe study by Rigueira et al. points out once more that cognitive impairment and depression are common comorbidities and complications in HF and they contribute to a worse symptom status, decreased quality of life and increased mortality. More studies are required to address these often overlooked mental aspects of HF for early diagnosis and to raise awareness of this complication among patients, their social network, the attending physician, and health care structures. Comprehensive care concepts in HF should include monitoring and targeting cognitive impairment and depression in order to slow down HF progression and to improve quality of life, symptom status and patient prognosis.
Conflicts of interestThe author has no conflicts of interest to declare.