Transradial access is widely used for both diagnostic and interventional cardiac procedures. The use of transradial access offers several advantages, including decreased bleeding, fewer vascular complications, and reduced length of hospital stay and cost. However, the small size of the radial artery limits the size of the equipment that can be used via this approach. In this study we sought to investigate whether preprocedural manual heating of the radial artery facilitates radial artery puncture.
MethodsPatients undergoing transradial cardiac catheterization were randomized to subcutaneous nitroglycerin plus diltiazem or manual heating. The study endpoint was puncture score (score 1: easiest – puncture at first attempt; score 2: second attempt; score 3: third attempt; score 4: fourth attempt or more; score 5: puncture failed).
ResultsNinety consecutive patients were enrolled in the study, 45 allocated to the drug treatment group and 45 to the heating group. Patients underwent radial artery ultrasound before catheterization. Complications were rare: one hematoma (drug treatment group) and one radial artery occlusion (heating group). Baseline demographic and clinical characteristics were similar. Baseline radial artery diameter was similar in both groups (2.41±0.46 mm and 2.29±0.48 mm in the heating and drug treatment groups, respectively). However, the median puncture score was lower in the heating group (1; interquartile range 1-2) compared to the drug treatment group (2; interquartile range 1-3; p=0.001).
ConclusionsPreprocedural manual heating of the radial artery facilitates radial artery puncture in patients undergoing transradial cardiac catheterization.
O acesso transradial (ATR) é usado habitualmente quer para procedimentos diagnósticos quer de intervenção coronária. O uso de ATR oferece várias vantagens: redução das hemorragias, menos complicações vasculares, menor tempo de internamento e representa menos custos associados. Porém, o reduzido calibre da artéria radial limita o tamanho dos dispositivos que podem ser usados por este acesso. Neste estudo, investigamos se o prévio aquecimento da artéria radial facilita, ou não, a punção radial.
MétodosDoentes submetidos a cateterismo cardíaco por ATR foram aleatorizados para uma administração subcutânea de uma combinação de nitroglicerina e diltiazem ou, em alternativa, aquecimento manual da artéria radial. O endpoint do estudo foi o score de punção (score 1: punção simples à primeira tentativa; score 2: punção à segunda tentativa; score 3: punção à terceira tentativa; score 4: punção à quarta ou mais tentativa; score 5: punção radial falhada).
ResultadosNoventa doentes consecutivos foram incluídos no estudo – 45 no grupo de tratamento farmacológico e 45 no grupo de aquecimento manual. Os doentes fizeram avaliação ecográfica da artéria radial antes do cateterismo. As complicações ocorreram de forma rara: um hematoma (grupo tratamento) e uma oclusão radial (grupo aquecimento). As caraterísticas basais demográficas e clínicas foram semelhantes. O diâmetro basal da artéria radial foi semelhante em ambos os grupos (2,41 ± 0,46 mm e 2,29 ± 0,48 mm nos grupos de aquecimento e de tratamento, respetivamente). No entanto, o score de punção foi mais baixo no grupo aquecimento (1; intervalo interquartil 1-2) comparado com o grupo tratamento (2; intervalo interquartil 1-3; p=0,001).
ConclusõesO aquecimento manual da artéria radial facilita a punção radial em doentes submetidos a cateterismo cardíaco por via transradial.
The transradial access approach is effective for cardiac catheterization and percutaneous coronary intervention.1,2 It is becoming increasingly popular due to lower vascular complication rates, reduced costs, and earlier mobilization.3–6 Local complications remain low even in high-risk subgroups such as the elderly or obese, females, after acute myocardial infarction or under anticoagulation.7–10 The transfemoral approach is associated with greater procedural complications, particularly access-site major bleeding, which is becoming an increasingly important issue in the era of more potent antiplatelet and antithrombotic agents used to prevent cardiac ischemia, and is associated with more adverse clinical events, including mortality.11,12 Although the transradial approach is a demanding technique, with a steep learning curve due to a high number of procedural failures before gaining experience, at present it is the first-line access in many interventional cardiology centers.13–15 In a comparison of radial and femoral approaches in patients undergoing coronary angiography or intervention, a lower rate of access-related complications was observed with radial access.16 In the RIVAL study on patients with acute coronary syndrome, radial artery access reduced the composite primary outcome and mortality.12 The RIFLE-STEACS study showed that radial access in patients with ST-segment elevation acute coronary syndrome is associated with significant clinical benefits, in terms of both lower morbidity and cardiac mortality.17 In the MATRIX trial of patients with acute coronary syndrome undergoing invasive management, radial as compared with femoral access reduced net adverse clinical events, through a reduction in major bleeding and all-cause mortality.18 For these reasons, the radial approach is becoming increasingly popular.
The main problem is the difficulty of the initial puncture of a small and highly reactive artery. Radial spasm increases after subcutaneous injection of lidocaine during local anesthesia, because lidocaine at room temperature is colder than body temperature.
Cold stimulates the sympathetic nervous system and sympathetic stimulation causes vasoconstriction.19 Subcutaneous injections of lidocaine or other medications cause radial artery vasoconstriction, which hampers radial puncture, sheath insertion and coronary angiography. Manual heating inhibits cold-induced vasoconstriction and may decrease the duration of sheath insertion.
Topical and subcutaneous use of nitroglycerin before transradial access has been shown to facilitate radial access by increasing the diameter of the artery, improving palpability of the radial pulse and reducing arterial spasticity.20,21
The present study was a prospective randomized trial comparing manual heating of the radial artery vs. the combination of subcutaneous nitroglycerin plus diltiazem before transradial access in terms of the spasmolytic effect on the radial artery and ease of transradial access.
MethodsStudy populationBetween July 2015 and September 2015, a total of 106 consecutive patients who underwent a transradial approach due to suspected stable coronary artery disease were enrolled in the study. Patients with previous transradial coronary revascularization, acute coronary syndrome, abnormal pulse oximetry plethysmography test, hemodynamic impairment, uncontrolled hypertension, vasculopathy, or inability to tolerate nitroglycerin or lidocaine due to allergy or medication interactions were excluded. In total, 16 patients were excluded, and 90 patients were included and randomized.
Hypertension was defined as documented systolic blood pressure of ≥140 mmHg and/or diastolic blood pressure of ≥90 mmHg in at least two measurements or active use of any antihypertensive agent. Diabetes was diagnosed as fasting plasma glucose over 126 mg/dl or 2-h glucose over 200 mg/dl in any measurement or active use of an antidiabetic agent. Smoking was defined as current smoking. Patients’ weight and height were recorded and body mass index (BMI) was calculated as weight in kg divided by the square of height in m. Body surface area (BSA) was calculated using the Mosteller formula.
Blood samples were obtained from the antecubital vein after a 12-hour fasting period. A Coulter LH series analyzer (Beckman Coulter Inc., Hialeah, FL) was used to obtain a complete blood count. Plasma levels of triglycerides, high-density lipoprotein, low-density lipoprotein, glucose, and creatinine were assessed using an automated chemistry analyzer (Abbott Aeroset, USA) using commercially available kits (Abbott, USA).
The study complied with the principles of the Declaration of Helsinki and was approved by the local ethics committee. All patients provided written informed consent before the procedure.
Measurement of radial artery diameterAll patients underwent radial artery ultrasound before catheterization. The radial artery was measured using B-mode ultrasound (Mindray M7 system, Mindray Medical International Limited, Shenzhen, PRC), using a 7L4s linear probe (5-10 mHz) before the procedure. The radial artery was located, and radial diameters were measured 3 cm proximal to the styloid process at the R peak of the electrocardiogram. For each image, the mean of five measurements was obtained.
ProceduresPatients undergoing transradial cardiac catheterization were randomized to a combination of subcutaneous nitroglycerin plus diltiazem or to manual heating (Balbay maneuver). The operators were blinded to the study. The operator's assistant used one of the two methods, and then cardiac catheterization was performed by the operator. The baseline patency of the palmar arch was assessed with a combination of pulse oximetry and plethysmography as described by Barbeau et al.22 in all patients. Patients with a type D response on the Barbeau test were excluded from the study. Routine prior sedation with agents such as midazolam or diazepam was not used in the study. In the first study arm, 200 mg nitroglycerin plus 2 mg diltiazem subcutaneously was used at the time of local anesthesia (1% lidocaine subcutaneously) regardless of the presence of a faint radial pulse. In the other study arm, manual heating (Balbay maneuver) was applied to all patients regardless of the presence of a faint radial pulse. The Balbay maneuver is defined as heating the radial artery site for three minutes with the palm (Figure 1) after administration of 1% lidocaine for local anesthesia subcutaneously. An arterial sheath is then inserted into the artery. In the study we used the Seldinger technique with a single anterior wall puncture. The artery was punctured with a sharp hollow needle, the syringe was detached and the guidewire advanced through the lumen of the needle, and the needle was withdrawn. A 10-cm 6F hydrophilic sheath (Radifocus Introducer II, Terumo, Leuven, Belgium) was then passed over the guidewire into the vessel.23,24 After sheath insertion, a radial cocktail containing 2 mg diltiazem, 200 mg nitroglycerin and heparin 5000 IU diluted in a 10-ml syringe was injected gradually through the sheath side arm into the radial artery. Coronary angiography was performed using 6F catheters (Boston Scientific). All coronary angiograms were performed by two interventional cardiologists experienced in radial access.
Study endpointThe study endpoint was puncture score, defined as score 1: successful puncture at first attempt; score 2: second attempt; score 3: third attempt; score 4: fourth attempt or more; score 5: puncture failed.
Statistical analysisSPSS 21.0 for Windows (IBM SPSS Inc., Chicago, IL, USA) was used for statistical analysis. Continuous variables were expressed as means ± standard deviation and categorical variables were expressed as numbers and percentages. The Kolmogorov-Smirnov test was used to test normality of distribution and the Student's t test and the Mann-Whitney U test were used to compare parametric and nonparametric continuous variables, respectively. Differences between treatment groups for categorical variables were analyzed using the chi-square test. A p value <0.05 was considered significant.
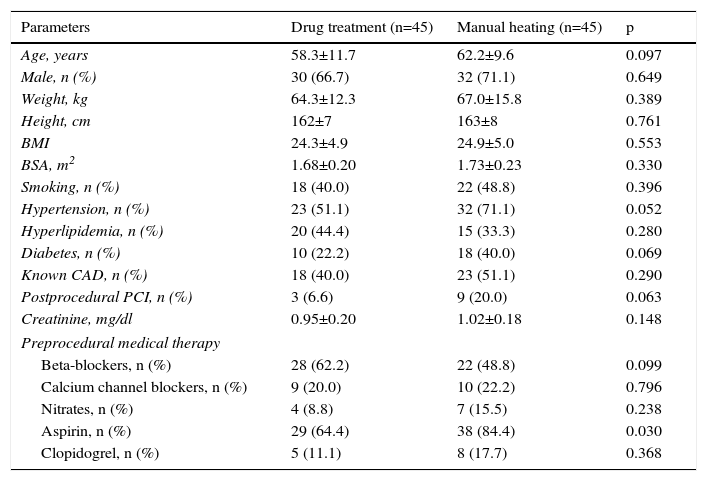
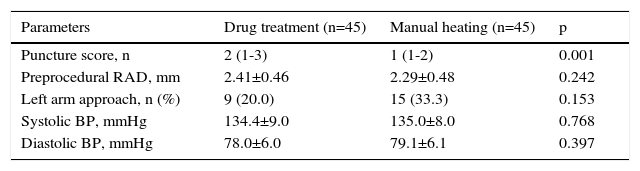
ResultsA total of 90 patients were enrolled in the study, 45 randomized to subcutaneous nitroglycerin plus diltiazem and 45 to manual heating (Balbay maneuver). The mean age of the participants was 60.2±10.8 years and 68.8% were male. Baseline characteristics and laboratory parameters were similar between groups with the exception of aspirin use (p>0.05). Patients’ weight, height, BMI, and BSA were similar between the groups (p>0.05) (Table 1). Complications were rare: one hematoma in the drug treatment group and one radial artery occlusion in the heating group. Baseline radial artery diameter was similar between the groups (2.41±0.46 vs. 2.29±0.48 mm; p=0.242). There was also no difference between the groups in blood pressure (p>0.05). Puncture score was lower in patients with manual heating than in those treated with subcutaneous nitroglycerin plus diltiazem (2 [1-3]) vs. 1 [1-2]; p=0.001) (Table 2). Successful puncture of the radial artery at the first attempt was significantly more common in the manual heating group (p=0.001) (Table 3).
Baseline characteristics and laboratory parameters of the study population.
| Parameters | Drug treatment (n=45) | Manual heating (n=45) | p |
|---|---|---|---|
| Age, years | 58.3±11.7 | 62.2±9.6 | 0.097 |
| Male, n (%) | 30 (66.7) | 32 (71.1) | 0.649 |
| Weight, kg | 64.3±12.3 | 67.0±15.8 | 0.389 |
| Height, cm | 162±7 | 163±8 | 0.761 |
| BMI | 24.3±4.9 | 24.9±5.0 | 0.553 |
| BSA, m2 | 1.68±0.20 | 1.73±0.23 | 0.330 |
| Smoking, n (%) | 18 (40.0) | 22 (48.8) | 0.396 |
| Hypertension, n (%) | 23 (51.1) | 32 (71.1) | 0.052 |
| Hyperlipidemia, n (%) | 20 (44.4) | 15 (33.3) | 0.280 |
| Diabetes, n (%) | 10 (22.2) | 18 (40.0) | 0.069 |
| Known CAD, n (%) | 18 (40.0) | 23 (51.1) | 0.290 |
| Postprocedural PCI, n (%) | 3 (6.6) | 9 (20.0) | 0.063 |
| Creatinine, mg/dl | 0.95±0.20 | 1.02±0.18 | 0.148 |
| Preprocedural medical therapy | |||
| Beta-blockers, n (%) | 28 (62.2) | 22 (48.8) | 0.099 |
| Calcium channel blockers, n (%) | 9 (20.0) | 10 (22.2) | 0.796 |
| Nitrates, n (%) | 4 (8.8) | 7 (15.5) | 0.238 |
| Aspirin, n (%) | 29 (64.4) | 38 (84.4) | 0.030 |
| Clopidogrel, n (%) | 5 (11.1) | 8 (17.7) | 0.368 |
BMI: body mass index; BSA: body surface area; CAD: coronary artery disease; PCI: percutaneous coronary intervention. Data are given as mean ± SD or n (%).
Preprocedural radial artery parameters of the study population.
| Parameters | Drug treatment (n=45) | Manual heating (n=45) | p |
|---|---|---|---|
| Puncture score, n | 2 (1-3) | 1 (1-2) | 0.001 |
| Preprocedural RAD, mm | 2.41±0.46 | 2.29±0.48 | 0.242 |
| Left arm approach, n (%) | 9 (20.0) | 15 (33.3) | 0.153 |
| Systolic BP, mmHg | 134.4±9.0 | 135.0±8.0 | 0.768 |
| Diastolic BP, mmHg | 78.0±6.0 | 79.1±6.1 | 0.397 |
BP: blood pressure; RAD: radial artery diameter. Data are given as mean ± SD, n (%) or median (interquartile range).
Our study demonstrated that the Balbay maneuver after local anesthesia in the setting of radial access for coronary angiography or angioplasty was feasible, facilitated radial artery puncture and may decrease the duration of sheath insertion. This result was observed with operators highly experienced in transradial access, and could be generalized for less experienced operators, including those training in the technique. This is the first study to demonstrate the feasibility of preprocedural manual heating of the radial artery.
The radial access was first used in 1989. This approach showed real advantages, with fewer bleeding and vascular complications, earlier mobilization and earlier discharge from the hospital. But insertion of a radial sheath in the radial artery may be technically difficult because of small artery caliber, arterial vasospasm and low patient pain threshold. The radial artery has a small diameter (2.3-3.4 mm) and is composed of concentric smooth muscle layers, with dense alpha-1 adrenergic innervation.25–27 Spasm is the major complication of radial access and occurs mainly in females when there are painful and repeated punctures.
Tarhan et al. reported that hypothermia plays an important role in radial artery vasospasm.28 It is important to determine the main factors that cause abnormal vasoconstrictor activation in the vessel, which include trauma from the lidocaine injector, temperature changes, and release of vasoconstrictors and certain hormones. For a transradial approach, lidocaine or other subcutaneous pharmacological agents such as nitrates or calcium channel blockers injected into the radial access site are at room temperature. Room temperature (around 22-24°C) is always colder than body temperature. Exposure to cold stimulates cold receptors in the skin, which causes cold thermal sensations and stimulates the sympathetic nervous system. Sympathetic stimulation causes vasoconstriction in skin, arms and legs.19 This physiological response of the body after lidocaine or other subcutaneous injections causes radial artery vasoconstriction, which hampers radial puncture, sheath insertion and coronary angiography. Manual heating may decrease the duration of sheath insertion.
In our study we performed the Balbay maneuver to counteract the vasoconstrictor effects of cold. Manual heating of the radial access site results in vasodilation, a stronger radial pulse and greater likelihood of successful radial artery puncture with the Seldinger needle. Puncture scores were lower in patients with manual heating than in those treated with subcutaneous nitroglycerin plus diltiazem. This result shows that the Balbay maneuver after lidocaine injection facilitates radial puncture and sheath insertion. The technique is cheap, involving no additional cost, and can be performed by anyone. We believe that the Balbay maneuver could be routinely used in transradial coronary catheterization.
Our study is limited by being in a single center with a small sample, and so further investigation is needed. It was also not a double-blind study; only the operators were blinded. Furthermore, there was no control group who did not undergo either subcutaneous nitroglycerin plus diltiazem injection or manual heating.
ConclusionManual heating of the radial artery site significantly reduced the number of radial puncture attempts. Preprocedural manual heating of the radial artery area by the Balbay maneuver is feasible and facilitates radial artery puncture in patients undergoing transradial cardiac catheterization.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.