Left ventricular noncompaction (LVNC) is now recognized as a distinct form of cardiomyopathy with a clinical presentation and natural history of its own. Common manifestations of LVNC include heart failure, ventricular arrhythmias and embolic events, but serious atrioventricular conduction disturbances are rarely reported in the literature. The authors describe the case of a 40-year-old woman who went to the emergency department due to syncope. The ECG revealed left bundle branch block (LBBB) and 2:1 atrioventricular block (AVB) and the patient was admitted for pacemaker implantation. During hospitalization she developed torsade de pointes and complete AVB with increased QTc. The echocardiogram showed images compatible with LVNC. This case provides additional evidence that LVNC may be complicated by 2:1 (or complete) AVB, intraventricular conduction disturbances (LBBB) and repolarization abnormalities (long QT). This combination of electrocardiographic changes has rarely been reported in the literature. We describe a series of affected patients, focusing on electrocardiographic characteristics.
O ventrículo esquerdo não compactado (VENC) tem sido reconhecido como uma forma distinta de miocardiopatia com uma apresentação clínica e história natural próprias. As manifestações comuns de VENC são insuficiência cardíaca, arritmias ventriculares e eventos embólicos. A presença de perturbações da condução auriculoventricular de maior gravidade encontra-se raramente descrita na literatura. Os autores descrevem o caso clínico de uma paciente com 40 anos de idade, que recorreu ao Serviço de Urgência por síncope. O ECG revelou bloqueio completo de ramo esquerdo do feixe de His e bloqueio auriculoventricular (BAV) 2:1, tendo sido internada para implantação de pacemaker. Durante o internamento, desenvolve fenómenos de torsade de pointes e de BAV completo com aumento do intervalo QTc. O ecocardiograma revelou imagens compatíveis com VENC. Com este caso, os autores fornecem evidência adicional de que a presença de VENC pode ser complicada por BAV 2:1 (ou completo), perturbações da condução intraventricular (BCRE) e da repolarização (QT longo), alterações eletrocardiográficas concomitantes pouco descritas na literatura. Descreve-se uma série de pacientes afetados, com foco nas características eletrocardiográficas.
Left ventricular noncompaction (LVNC) is a rare cardiomyopathy originally described in children1,2 but whose phenotypic characteristics are increasingly documented in adults.3–7 The most common symptoms of LVNC are heart failure (HF), ventricular arrhythmias and embolic events, but atrioventricular conduction disturbances are rarely reported in the literature.8–10
Case reportA 40-year-old woman went to the emergency department due to syncope during a meal, without prodrome and with spontaneous recovery, associated with progressive fatigue for around a month. She reported no chest pain or dyspnea. Personal history included complete left bundle branch block (LBBB) detected on a routine electrocardiogram (ECG) as part of a medical check-up at work three months before. There was no family history of sudden death and she was not taking any medication.
Physical examination showed the patient to be eupneic with no signs of respiratory difficulty. Cardiac auscultation revealed rhythmic sounds and no murmurs but bradycardia (40 bpm); pulmonary auscultation detected no abnormalities. Blood pressure was 100/75 mmHg. The rest of the physical examination was normal.
Laboratory tests, including blood and biochemical analysis, showed no relevant alterations and biomarkers of myocardial necrosis were normal.
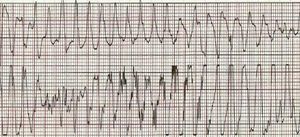
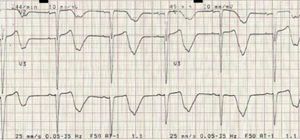
A 12-lead ECG revealed second-degree 2:1 atrioventricular block (AVB) with ventricular response of ±45 bpm and LBBB, and the patient was accordingly admitted for pacemaker implantation (Figure 1).
During hospitalization she developed cardiac arrest due to torsade de pointes (TdP) (Figure 2), reverted by cardiac massage. The ECG revealed 2:1 AVB (with a period of complete AVB), heart rate of ±45 bpm and increased QTc interval (Figure 3).
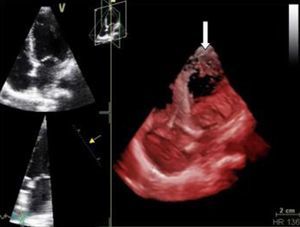
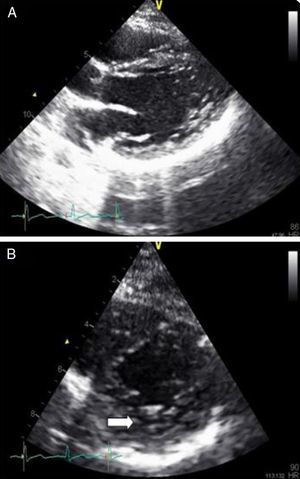
Echocardiography performed in the context of monitoring in the cardiac care unit showed a normal-size left ventricle with mildly impaired global systolic function (ejection fraction ±45%) and images compatible with LVNC at the apex (pronounced trabeculations and ratio of trabeculated to non-trabeculated layers >2, with blood flow on color Doppler) (Figures 4 and 5). Coronary angiography revealed no coronary disease.
A dual-chamber cardioverter-defibrillator was accordingly implanted for secondary prevention of sudden death.
The patient was discharged clinically stable and is currently well with no signs of HF. She is pacing dependent but no shocks have been detected. Screening of first-degree relatives showed normal ECG but echocardiography in her children showed images compatible with inferior and lateral LVNC (Figure 6), although high-resolution ECG showed no abnormalities. The results of the patient's genetic study are awaited.
DiscussionPatients with LVNC usually have impaired left ventricular systolic function and generally present with symptoms of HF.1,2,4 Other associated cardiac alterations include endocardial thrombi, leading to systemic embolism, and arrhythmias. The high incidence of arrhythmias in LVNC is not explained by a known morphological abnormality, but it has been suggested that myocardial ischemia may play an important role in the development of systolic dysfunction and arrhythmias in these patients, as is seen in ischemic heart disease.11A variety of rhythm disturbances have been reported in LVNC, of which ventricular arrhythmias are the most common; they may be refractory to medical treatment and can be fatal.1–4,11–15
The literature shows that 88–94% of LVNC patients have alterations on the baseline ECG.2,3,16 In a series by Oechslin et al.,4 94% of the 34 adults studied presented abnormal ECGs and 56% had intraventricular conduction defects, most of them identified in patients who had died. In a series by Steffel et al.16 (n=78), only 13% of the patients had a normal ECG, while two (3%) had complete AVB block, 19% had LBBB, and 50% had prolonged QTc.
Wolff–Parkinson–White syndrome (WPW) and associated tachycardias have also been described in association with LVNC.1,2,14,17 Ichida et al.2 reported WPW syndrome in four of 27 patients with LVNC, and explained this association as a failed regression of developmental embryologic atrioventricular anatomical and electrical continuity during embryonic development in the non-compacted myocardium. Supraventricular tachycardias associated with WPW syndrome can thus trigger fatal ventricular tachycardia and fibrillation in patients with LVNC.1,17
In our series6 (n=20) (Table 1), there was one case of 2:1/intermittent complete AVB, three cases of LBBB, and six cases of increased QTc interval; two cases presented as ventricular tachycardia. Only two patients (10%) had a normal ECG, a similar proportion to that reported by Oechslin et al. There were no cases of WPW syndrome.
ECG abnormalities in our series of patients with LVNC (n=20; mean age 52.8 years; 71% male).
| n | Percentage | |
| Rhythm | ||
| Sinus | 15 | 75% |
| Atrial fibrillation | 5 | 25% |
| Ventricular arrhythmia at admission | ||
| No | 18 | 90% |
| Yes | 2 | 10% |
| AV conduction disturbances | ||
| No | 15 | 75% |
| 1st-degree AVB | 4 | 20% |
| 2nd-degree/complete AVB | 1 | 5% |
| Intraventricular conduction disturbances | ||
| No | 13 | 65% |
| Left anterior hemiblock | 3 | 15% |
| RBBB | 1 | 5% |
| LBBB | 3 | 1% |
| Repolarization disturbances – stressa | ||
| No | 10 | 50% |
| Yes | 7 | 35% |
| Repolarization disturbances – ischemiaa | ||
| No | 13 | 65% |
| Yes | 4 | 20% |
| Long QTc interval | ||
| No | 14 | 70% |
| Yes | 6 | 30% |
| Signs of left ventricular hypertrophya | ||
| No | 14 | 70% |
| Yes | 3 | 15% |
AV: atrioventricular; AVB: atrioventricular block; LBBB: left bundle branch block; RBBB: incomplete right bundle branch block.
The cause of intraventricular conduction disturbances and repolarization abnormalities in LVNC is unknown. Ichida et al.2 suggest that conduction disturbances such as LBBB and repolarization abnormalities such as increased QTc result from progressive endocardial fibrosis, and are often observed in adult patients because fibrotic changes develop gradually.8
With regard to the atrioventricular conduction disturbances observed in this case (second-degree/intermittent complete AVB), it is suspected that they may be caused by histological alterations in the conduction system itself8 alongside the endomyocardial fibrotic process. However, long QT complicating AVB, with concomitant ventricular arrhythmias such as TdP, is also frequently seen in association with conduction disturbances of any etiology, and may be aggravated by the presence of LVNC for the reasons described above.
The probability of patients under antiarrhythmic medication and/or with ionic imbalance developing long QT and TdP is increased by bradycardia due to reverse use-dependence of potassium channels.18 However, the role of bradycardia itself in the genesis of TdP is less clear.19,20 This question was addressed in a study19 of 14 patients with complete AVB, six of whom had a history of TdP. There was no difference in the frequency of ventricular escape rhythm between the two groups, but QTc was significantly longer in those with a history of TdP (0.59 vs. 0.48 s). After pacemaker implantation, QTc was still longer in those with a history of TdP, irrespective of whether the lower rate limit was set at 60 bpm (0.55 vs. 0.50 s) or 50 bpm (0.70 vs. 0.53 s).
ConclusionLVNC is often difficult to diagnose, but a high degree of clinical awareness is necessary due to its poor prognosis.
To the best of our knowledge, this is the first reported case of LVNC associated with LBBB, second-degree/intermittent complete AVB, ventricular arrhythmia and long QT syndrome. We therefore propose that a diagnosis of LVNC be considered in relatively young individuals who present with high-degree AVB and LBBB and with a relevant clinical history.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Rodrigues B, et al. Bloqueio completo de ramo esquerdo, bloqueio auriculoventricular, torsade de pointes e QT longo: será demasiado para uma rara miocardiopatia? Rev Port Cardiol. 2013. http://dx.doi.org/10.1016/j.repc.2012.06.018.