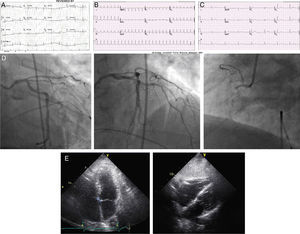
A 69‐year‐old man with a history of tobacco abuse was referred to our hospital with 3/10 chest pain for 12 hours, a normal ECG (Figure 1A) and a slight increase in cardiac enzymes. En route, he developed palpitations without increase in chest pain. On arrival his ECG showed atrial fibrillation with a ventricular response of 160 bpm (Figure 1B). After one hour on intravenous diltiazem infusion he converted to a junctional rhythm at 30–50 bpm with resolution of symptoms (Figure 1C). Cardiac catheterization with temporary pacemaker back‐up revealed an occluded small non‐dominant right coronary artery with mild left coronary atherosclerosis and collaterals to the right system (Figure 1D). Two‐dimensional echocardiography revealed normal left and right ventricular function with a dilated right atrium (Figure 1E). Due to persistence of the junctional rhythm a dual chamber pacemaker was implanted. Positioning of the atrial lead in ten different right atrial positions at high amplitude revealed absence of atrial electrical activity. This was thought to be secondary to right atrial stunning or infarction. The right atrial lead was left in place and the pacemaker was set in VVI mode.
Right atrial infarction is a rare entity which is commonly overshadowed by inferior or right ventricular infarction and is usually diagnosed on autopsy.1–3 In our case, occlusion of a small non‐dominant right coronary artery resulted in isolated right atrial infarction with chamber dilation, loss of electrical activity and junctional escape rhythm, and preserved biventricular function.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.