Infection remains a major complication among heart transplant (HT) recipients, causing approximately 20% of deaths in the first year after transplantation. In this population, Aspergillus species can have various clinical presentations including invasive pulmonary aspergillosis (IPA), which has high mortality (53-78%).
AimsTo establish the characteristics of IPA infection in HT recipients and their outcomes in our setting.
MethodsOf 328 heart transplantations performed in our center between 1998 and 2016, five cases of IPA were identified. Patient medical records were examined and clinical variables were extracted.
ResultsAll cases were male, with a mean age of 62 years. The most common indication for HT was nonischemic dilated cardiomyopathy. Productive cough was reported as the main symptom. The imaging assessment was based on chest radiography and chest computed tomography. The most commonly reported radiological abnormality was multiple nodular opacities in both techniques. Bronchoscopy was performed in all patients and A. fumigatus was isolated in four cases on BAL culture. Treatment included amphotericin in four patients, subsequently changed to voriconazole in three patients, and posaconazole in one patient, with total treatment lasting an average of 12 months. Neutropenia was found in only one patient, renal failure was observed in two patients, and concurrent cytomegalovirus infection occurred in three patients. All patients survived after a mean follow-up of 18 months.
ConclusionsIPA is a potentially lethal complication after HT. An early diagnosis and prompt initiation of aggressive treatment are the cornerstone for better survival.
A infeção continua a ser a principal complicação dos doentes submetidos a transplante cardíaco (TC), originando aproximadamente 20% de mortalidade no primeiro ano pós transplante. Nesta população, a infeção Aspergillus pode causar diferentes quadros clínicos, incluindo a aspergilose pulmonar invasiva (API), com elevada mortalidade (53 a 78%).
ObjetivosEstabelecer as características da infeção por API nos doentes de TC e apresentar os respetivos resultados do nosso centro.
MétodosDe 328 transplantes cardíacos realizados no nosso centro entre 1998 e 2016, identificámos cinco casos de API. Os registos médicos dos doentes foram examinados e as variáveis clínicas foram analisadas
ResultadosTodos os casos corresponderam a doentes do sexo masculino com a idade média de 62 anos. A indicação mais comum para TC foi a miocardiopatia dilatada não isquémica. A tosse produtiva foi registada como principal sintoma. A avaliação radiológica baseou-se na radiografia e na tomografia computorizada ao tórax. A alteração radiológica mais comum foi, em ambas as técnicas, o registo de densidades nodulares múltiplas. A broncoscopia foi realizada em todos os doentes e o aspergillus fumigatus foi isolado em quarto casos de cultura BAL. O tratamento incluiu anfotericina em quatro doentes com mudança subsequente para voriconazol em três doentes e posaconazol em um doente, duração média do tratamento total de 12 meses. A neutropenia foi observada apenas num doente, a insuficiência renal em dois doentes e a infeção por CMV concomitante ocorreu em três doentes. Todos os doentes sobreviveram após um seguimento médio até 18 meses.
ConclusõesA API representa uma complicação potencialmente letal após TC. O diagnóstico precoce e a instituição também precoce de tratamento agressivo constituem a pedra angular para uma melhor sobrevivência.
Infection remains a major complication among transplant recipients, causing approximately 20% of deaths in the first year after transplantation, as well as being a major cause of long-term morbidity and mortality. In solid organ transplants, such as cardiac transplantation, for which immunosuppressants are prescribed indefinitely, physicians and patients perpetually negotiate the delicate balance between the risks of graft rejection and infection.1 In this immunosuppressed population, Aspergillus species are opportunistic pathogens that can cause aggressive infections including sinusitis, tracheobronchitis, pneumonia, necrotizing cellulitis, brain abscess, and disseminated disease. In heart transplant (HT) recipients, Aspergillus spp. have been reported as the most common cause of invasive fungal infection and frequently causes pneumonia2 with a high attributable mortality, ranging from 53% to 78%.3–5 Although invasive pulmonary aspergillosis (IPA) is a serious disease in this population, little is known about its natural history. The aim of this study was to further establish the characteristics of IPA infections and their outcomes in our setting.
MethodsWe conducted a retrospective chart review of patients who underwent HT at our center between 1998 and 2016 and subsequently developed invasive pulmonary aspergillosis (IPA). Cases were identified according to the clinical practice guidelines of the Infectious Diseases Society of America for IPA6 and the revised EORTC/MSG criteria7 for defining invasive fungal infection, including IPA. The diagnosis was considered definite when the patient had positive histology and culture of a sample obtained from the same site, or negative histology (or not performed) and positive culture results of a sample obtained by protocol-specified invasive techniques such as bronchoalveolar lavage (BAL). A serum galactomannan index of 1 or higher was regarded as positive and suggested a diagnosis of IPA.
Data collection included age, gender, primary cardiac diagnosis, date of transplantation, immunosuppressive regimen, cytomegalovirus serological status, antifungal prophylaxis, known risk factors for IPA (including neutropenia), radiographic features, serum galactomannan level, bronchoscopy and microbiology data (Tables 1 and 2).
Demographic and clinical characteristics and laboratory features of the study population.
| Case | Age, years | Gender | Indication | Days since HT | Prednisone dose | Immunosuppression | Leukocytes/neutrophils | Creatinine (mg/dl) |
|---|---|---|---|---|---|---|---|---|
| 1 | 59 | Male | Dilated cardiomyopathy | 5 | 60 | Cyclosporine + mycophenolate | 9.5 | 1.6 |
| 2 | 70 | Male | Dilated cardiomyopathy | 12 | 50 | Tacrolimus + mycophenolate | 14.5 | 0.9 |
| 3 | 51 | Male | Chagas cardiomyopathy | 116 | 15 | Tacrolimus + azathioprine | 8.1 | 1.0 |
| 4 | 61 | Male | Valvular cardiomyopathy | 189 | 7.5 | Tacrolimus + mycophenolate | 2.9/1.2 | 1 |
| 5 | 71 | Male | Ischemic cardiomyopathy | 55 | 20 | Tacrolimus + mycophenolate | 12.2/10.8 | 1.6 |
HT: heart transplantation.
Clinical course and treatment.
| Case | Symptoms | Initial serum galactomannan level | Concurrent CMV infection | Confirmation test | Fungal prophylaxis | Chest radiography | CT scan | Treatment | Rejection |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Asymptomatic | 0.13 | Yes | BAL culture: A. fumigatus | Micafungin | None | Multiple micronodular opacities | Amphotericin B | 1A |
| 2 | Productive cough | 4.23 | No | BAL culture: A. fumigatus | Fluconazole | Multiple nodular opacities | Multiple nodular opacities and a 45-mm mass with peripheral halo | Voriconazole + caspofungin | 1A |
| 3 | Productive cough and fever | 4.73 | Yes | PCR (A. fumigatus) | Fluconazole | Multiple nodular opacities | Multiple nodular opacities (<10 mm) | Amphotericin + caspofungin | 1B |
| 4 | Asymptomatic | 0.91 | No | BAL culture: A. fumigatus | Fluconazole | Unilateral nodular opacities | Multiple nodular opacities (<10 mm) | Voriconazole + anidulafungin | 1A |
| 5 | Chest pain | 5.0 | Yes | BAL culture: A. fumigatus | Fluconazole | Unilateral nodular opacities | Ground-glass pattern | Amphotericin B | 1A |
BAL: bronchoalveolar lavage; CMV: cytomegalovirus; CT: computed tomography; PCR: polymerase chain reaction.
At our institution, all patients by protocol receive induction therapy with basiliximab and high doses of corticosteroids. Basiliximab is administered 4-6 hours after delivery of the extracorporeal pump. The initiation of calcineurin inhibitors is delayed until day 3 post-HT. Maintenance immunosuppressive therapy consists of corticosteroids, calcineurin inhibitors and cell cycle inhibitors. This regimen is based on the recommendations of the International Society of Heart and Lung Transplantation guidelines for the care of HT recipients.8
In our HT protocol, all patients without risk factors for infection by filamentous fungi are administered fluconazole 100 mg/day during the first month, from day 1 post-transplant. Patients at risk for infection by filamentous fungi (at least one of the following risk factors: administration of immunosuppression; acute renal failure requiring hemodialysis; colonization by filamentous fungi such as Aspergillus; retransplantation or double transplantation [heart and kidney or heart and liver]) receive antifungal prophylaxis with liposomal amphotericin B or micafungin.
In all patients under antifungal prophylaxis, fungal culture and staining with calcium fluoride from sputum or respiratory secretions, chest X-rays and blood antigen for Aspergillus are performed once a week while hospitalized. If the chest radiography is doubtful, high-resolution chest computed tomography (CT) is performed.
After hospital discharge, patients are followed at our center every month for the first six months after HT, every two months from the sixth to the twelfth month, and then every six months indefinitely. At each visit a thorough clinical assessment is performed including routine laboratory analyses and a chest X-ray.
ResultsOf 328 HTs performed between 1998 and 2016, five cases of IPA were identified. All cases were male, with a mean age of 62 years (range 59-71 years). The most common indication for HT was nonischemic dilated cardiomyopathy. Antifungal prophylaxis was started in all patients, but two patients did not complete the course since IPA was diagnosed within 30 days of HT. One patient required prophylaxis with micafungin due to acute renal failure.
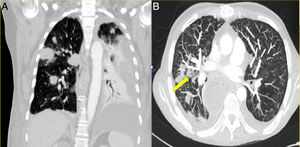
The median time from transplantation at diagnosis was 55 days. Productive cough was reported as the main symptom in two patients, one patient presented atypical chest pain and the two others were asymptomatic. In one of the asymptomatic patients the diagnosis was suspected from abnormal findings (unilateral nodular opacities) on the chest X-ray during a monthly protocol follow-up visit. In all patients, the imaging assessment was based on chest radiography and chest CT. The most commonly reported radiological abnormality was multiple nodular opacities in both imaging techniques, as shown in Figure 1. Halo sign was observed in one case (Figure 1b). Serum galactomannan level was abnormally high in three of the five patients. Bronchoscopy was performed in all patients and A. fumigatus was isolated in BAL culture in four cases. Aspergillus was identified by polymerase chain reaction (PCR) in one patient in whom nodular lesions on the chest X-ray aroused suspicion of IPA.
Initial antifungal treatment included amphotericin in four patients, subsequently changed to voriconazole in three cases, and posaconazole in one patient, with total treatment lasting an average of 12 months. Two patients required the addition of caspofungin and one of anidulafungin as salvage therapy. Neutropenia was found in only one patient. Renal failure, defined as creatinine >1.5 mg/dl, was observed in two patients, and concurrent cytomegalovirus (CMV) infection occurred in three patients. All patients survived after a mean follow-up of 18 months.
DiscussionSince the introduction of HT as a therapeutic modality for end-stage heart failure in 1968, Aspergillus has been recognized as a major opportunistic pathogen with a high attributable mortality.5 Our series of five IPA cases show unusually low mortality. There are several possible reasons for this. First, the number of reported cases is small, however 100% survival seems too optimistic and some fatality would be expected among them. Second, two patients were asymptomatic at the time of diagnosis, both with negative serum galactomannan, and hence treatment was initiated early. Also, four patients received combined treatment with two antifungals and only one patient was treated with just one drug.
The known risk factors for IPA in HT recipients include isolation of A. fumigatus in respiratory tract cultures prior to HT, reoperation, CMV disease, post-transplant hemodialysis, and cases of IPA in the institution two months before the transplant.7 In the study by Muñoz et al.,4 IPA-related mortality was 11/17 (65%), and total mortality was 17/27 (63%), but this cohort presented a high proportion of risk factors for IPA – hemodialysis 19%, bacterial infection 63%, and rejection episode 44%. Also in this cohort, 82% of patients received either OKT3 or antithymocyte globulin as induction therapy. As is known, the stronger the immunosuppression, the higher the risk of infection. None of our patients needed hemodialysis, nor were there any rejection episodes requiring an increase in immunosuppression. Likewise, our patients received basiliximab instead of OKT3 or antithymocyte globulin. Basiliximab is associated with fewer infections overall than OKT3 or antithymocyte globulin in solid organ transplantation.9
Although this case series may suffer from publication bias, we consider our results to be justified by early diagnosis based on serum galactomannan level and early bronchoscopy followed by initiation of aggressive treatment, as well as the patients’ clinical characteristics. Our findings can be attributed to improved outcomes resulting from early diagnosis, as has been demonstrated in patients with hematological malignancy and invasive fungal infection.
Finally, it seems clear that, as in many other fields of medicine, the prognosis of these patients is improving as more is learned about complications. Moreover, newer diagnostic techniques enable earlier initiation of treatment with modern therapeutic strategies. As Montoya et al.3 concluded, patients suffering IPA in recent years may have a better prognosis than those treated before. Is this the time that IPA mortality begins to fall?
ConclusionIPA is a potentially lethal complication after HT. An early diagnosis and prompt initiation of aggressive treatment are the cornerstone for better survival.
Conflicts of interestThe authors have no conflicts of interest to declare.