The monocyte to high-density lipoprotein cholesterol ratio (MHR) has recently been proposed as a new predictor and prognostic indicator in cardiovascular disease. The TIMI risk score predicts short-term mortality in ST-elevation myocardial infarction (STEMI) patients. However, there have been no studies regarding the association between MHR and TIMI score in patients with STEMI.
MethodsA total of 161 patients admitted to our hospital were prospectively enrolled between January 2014 and June 2016. Of these, 111 consecutive patients with a diagnosis of STEMI who underwent primary percutaneous coronary intervention (PCI) were selected as the STEMI group, and the remaining 50 patients, who had angiographically normal coronary arteries, were selected as the control group. The 111 STEMI patients were then divided into two subgroups based on TIMI scores.
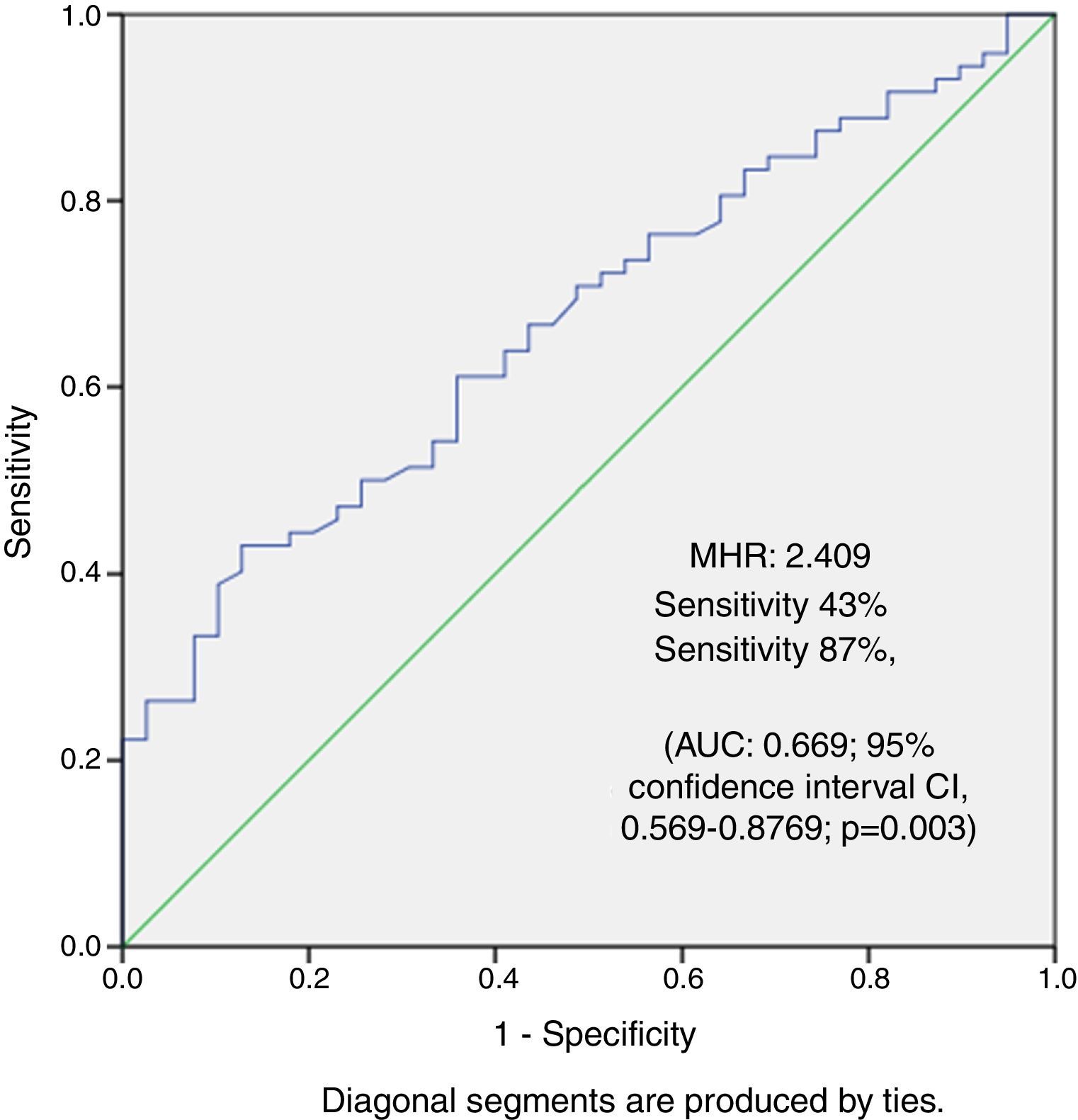
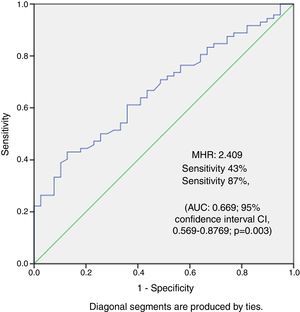
ResultsMHR was significantly higher in the STEMI group than in the control group (1.71±0.47 vs. 2.21±0.98, p=0.001) and was significantly higher in the high TIMI score group than in the low TIMI score group (1.80±0.59 vs. 2.42±1.09, p=0.001). In multivariate logistic regression analysis, MHR was the only independent predictor of acute STEMI and high TIMI score. In correlation analysis, there was a significant positive correlation between MHR and TIMI score in STEMI patients (r=0.479, p<0.001). The cutoff value of MHR for high TIMI score in patients with STEMI was 2.409, with a sensitivity of 43.06% and a specificity of 87.18% (AUC 0.669; 95% CI 0.569-0.8769; p=0.003) on ROC curve analysis.
ConclusionThis study indicates that MHR is independently and significantly associated with TIMI score in patients with STEMI. MHR is a novel inflammation-based marker and may be an independent predictor of future cardiovascular events in patients with STEMI.
A relação entre a contagem de monócitos e o nível de lipoproteína de alta densidade do colesterol (MHR) foi recentemente apresentada como um novo preditor e indicador prognóstico de doenças cardiovasculares. O score de risco TIMI prediz em curto prazo a mortalidade em doentes com STEMI. Contudo, não há estudo disponível acerca da associação entre o MHR e o score TIMI em doentes com STEMI.
Material e métodosForam recrutados 161 doentes prospetivamente entre janeiro de 2014 e junho de 2016. Dos 161 doentes, 111 foram admitidos consecutivamente no nosso hospital com o diagnóstico de STEMI e foram submetidos a PCI primária, foram designados como o grupo STEMI, os restantes 50 doentes fizeram angiografia com artérias coronárias normais e foram selecionados como grupo controle. Os 111 doentes com STEMI foram ainda divididos em dois subgrupos, de acordo com o score de risco TIMI.
ResultadosO MHR foi significativamente mais alto no grupo STEMI quando comparado com o grupo controle (1,71±0,47 versus 2,21±0,98, p=0,001) e foi significativamente mais alto no subgrupo de alto risco TIMI, quando comparado com o subgrupo de baixo risco TIMI (1,80±0,59 versus 2,42±1,09, p=0,001). O modelo de regressão logística multivariável demonstrou que o MHR só foi preditor independente no grupo STEMI com score TIMI de alto risco. Na análise de correlação, houve uma correlação positiva significativa entre o MHR e o score TIMI em doentes com STEMI (r=0,479, p<0,001). O valor de cut-off do MHR para o score TIMI alto em doentes STEMI foi 2,409 com uma sensibilidade de 43,06% e uma especificidade de 87,18% (AUC, 0,669; 95% com um intervalo de confiança de [CI], 0,569-0,8769; p=0,003) na análise de curva de ROC.
ConclusõesEste estudo indicou que o MHR está independente e significativamente associado ao score TIMI em doentes com STEMI. O MHR é um novo marcador de base inflamatória e pode ser um preditor independente de eventos cardiovasculares futuros em doentes com STEMI.
ST-elevation myocardial infarction (STEMI) is a significant cause of morbidity and mortality in patients with coronary heart disease. Patients with STEMI are at high risk for complications and poor outcome, including death. All patients with STEMI should undergo early risk stratification soon after admission. Multiple methods have been developed for risk stratification in STEMI. Complicated multivariable models developed for predicting mortality in patients with STEMI identify independent clinical predictors and quantify their relative contribution to mortality risk.1 One widely used and easily accessible model is the Thrombolysis in Myocardial Infarction (TIMI) risk score for STEMI, which is readily applied in routine clinical practice and is able to predict both early (30-day) and one-year mortality.2
The TIMI score was created and validated in a sample of patients with ST-segment elevation myocardial infarction. It is based on ten rapidly calculated clinical indices to provide a score between 0 and 14 points. The parameters included in the score are age, systolic blood pressure <100 mmHg, diabetes, angina, history of hypertension, heart rate >100 bpm, weight <67 kg, Killip class II-IV, anterior STEMI or left bundle branch block (LBBB), and time to treatment >4 hours. Time to treatment is defined as time from symptom onset to first balloon inflation.
The monocyte to high-density lipoprotein cholesterol (HDL-C) ratio (MHR) has emerged as a novel prognostic marker that has been reported to be related to cardiovascular outcomes in various cardiovascular diseases.3–5 Monocytes are a source of various cytokines associated with inflammatory processes. It has been found that monocytes and differentiated macrophages can modulate inflammatory cytokines and tissue remodeling in the pathophysiology of coronary artery disease (CAD).6 By contrast, the major function of HDL-C is to protect peripheral tissues through the removal of cholesterol and to suppress monocyte activation and the proliferation and differentiation of monocyte progenitor cells.7,8
To the best of our knowledge, there have been no studies investigating the relationship between MHR and TIMI risk score in STEMI patients. In this study, we aimed to investigate this relationship and its possible prognostic value for clinical risk stratification in STEMI patients.
MethodsStudy populationA total of 161 patients admitted to our hospital were prospectively enrolled between January 2014 and June 2016. Patients with a previous history of coronary revascularization, active infection, severe liver disease, autoimmune disease, cancer, hematological disorders, severe valvular disease, or inflammatory or infectious disease were excluded. After application of these exclusion criteria, a total of 161 patients remained in the study sample. Of these, 111 consecutive patients with a diagnosis of STEMI who underwent primary percutaneous coronary intervention (pPCI), and 50 patients who had angiographically normal coronary arteries randomly enrolled by two different experienced cardiologists without knowledge of the patients’ demographic and laboratory data, were included in this study. First, the study population were divided into two groups according to clinical presentation. The 111 STEMI patients who underwent pPCI were selected as the STEMI group, and the 50 patients with angiographically normal coronary arteries comprised the control group. Second, the 111 patients with STEMI were divided into two subgroups, based on TIMI scores: low (0-1) and high (≥2), calculated on the basis of median scores on admission.
All the controls had been referred for coronary angiography as outpatients due to symptoms suggestive of CAD and/or abnormal noninvasive stress tests (exercise electrocardiography or myocardial perfusion imaging). The diagnosis of STEMI was based on typical chest pain and new ST-segment elevation at the J point in ≥2 contiguous leads (≥0.2 mV in V1 through V3 and ≥0.1 mV in other leads) or new-onset LBBB. All patients received oral aspirin 300 mg, a loading dose of 600 mg clopidogrel and 70 U/kg of unfractionated heparin intravenously in the emergency department.
The study complied with the Declaration of Helsinki and was approved by the hospital's ethics review board. Informed consent was obtained from all participants.
Study protocolInformation on demographics, cardiovascular history, and risk factors (smoking, hypertension, and diabetes) was obtained from the patients’ medical records. Hypertension was defined as receiving antihypertensive therapy and/or blood pressure >140/90 mmHg. Diabetes was diagnosed on the basis of use of antidiabetic therapy or postprandial blood glucose >200 mg/dl or fasting plasma glucose ≥126 mg/dl at any time. A 12-lead ECG was recorded in the intensive care unit for each patient.
Laboratory parametersA complete blood count and biochemical analysis were obtained from blood samples taken by antecubital vein puncture at admission to the emergency room before pPCI. An automated blood cell counter (Beckman Coulter analyzer, Brea, CA, USA) was used to determine the blood count parameters of hemoglobin, white blood cells (WBC), neutrophils, lymphocytes, monocytes, and platelets. The blood biochemical parameters measured were glucose, creatine, total cholesterol, triglycerides, low-density lipoprotein cholesterol (LDL-C), HDL-C, total protein, albumin, aspartate aminotransferase (AST), alanine aminotransferase (ALT), sodium (Na), and potassium (K).
Coronary angiography and percutaneous coronary interventionEvery patient admitted with chest pain to the emergency department of our teaching and research hospital is assessed initially by a cardiologist. All patients underwent coronary angiography by the femoral approach using the standard Judkins technique. Iopromide as a contrast agent (Ultravist 370, Bayer Schering Pharma, Germany) and a 6F diagnostic catheter were used in all patients. STEMI patients received 300 mg aspirin, a loading dose of 600 mg clopidogrel and maintenance dose of 75 mg, and a 5000 IU bolus (70 IU/kg) of unfractionated heparin during pPCI. pPCI was performed on the culprit artery only except in cases of cardiogenic shock.
Statistical analysisSPSS for Windows, version 21.0 (IBM SPSS, Inc., Chicago, IL, USA), was used for all statistical calculations. Normality of data distribution was analyzed using the Kolmogorov-Smirnov test. Categorical variables were expressed as numbers and proportions, while continuous variables were expressed as means ± standard deviation. The chi-square test was used to compare groups regarding categorical variables. Normally distributed continuous variables were compared with the Student's t test. The correlation between baseline biomarkers was assessed with Spearman's correlation coefficient. Multivariate logistic regression analysis was used to determine independent predictors for high TIMI score. The predictive value of MHR for high TIMI score was analyzed by receiver operating characteristic curve (ROC) analysis.
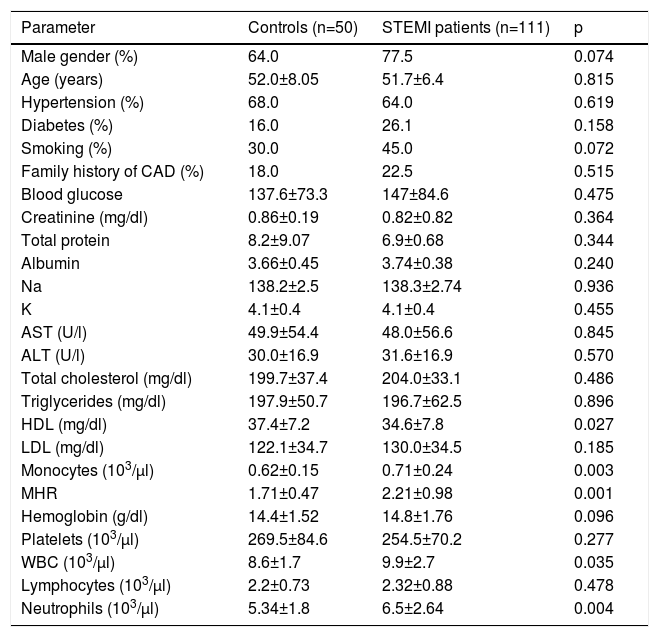
ResultsA total of 161 patients (118 male [73.3%]; mean age 51.8±6.9 years) were enrolled in the study. The baseline characteristics of the two groups according to clinical presentation are listed in Table 1. There were 50 patients (32 male [64%]; mean age 52.0±8.05 years) with normal coronary arteries and 111 patients (86 male [77.5%]; mean age 51.7±6.43 years) with acute STEMI. The control and STEMI groups were similar in terms of gender, smoking, family history, hypertension, diabetes, and age (Table 1). There were no significant differences between the two groups with respect to the serum biochemical parameters of glucose, creatinine, total cholesterol, triglycerides, LDL-C, total protein, albumin, AST, ALT, Na, and K (p>0.05 for all) except for HDL-C, which was significantly lower in the STEMI group (37.4±7.2 vs. 34.6±7.8 mg/dl, p=0.027). Regarding hematological parameters, there were significant differences between the groups: monocyte count (0.62±0.15 vs. 0.71±0.24×103/μl, p=0.003), MHR (1.71±0.47 vs. 2.21±0.98, p=0.001), WBC (8.6±1.7 vs. 9.9±2.7×103/μl, p=0.035) and neutrophil count (5.34±1.8 vs. 6.5±2.64×103/μl, p=0.004) were significantly higher in the STEMI group than in controls (Table 1).
Clinical and biochemical characteristics of patients with ST-elevation myocardial infarction and controls.
| Parameter | Controls (n=50) | STEMI patients (n=111) | p |
|---|---|---|---|
| Male gender (%) | 64.0 | 77.5 | 0.074 |
| Age (years) | 52.0±8.05 | 51.7±6.4 | 0.815 |
| Hypertension (%) | 68.0 | 64.0 | 0.619 |
| Diabetes (%) | 16.0 | 26.1 | 0.158 |
| Smoking (%) | 30.0 | 45.0 | 0.072 |
| Family history of CAD (%) | 18.0 | 22.5 | 0.515 |
| Blood glucose | 137.6±73.3 | 147±84.6 | 0.475 |
| Creatinine (mg/dl) | 0.86±0.19 | 0.82±0.82 | 0.364 |
| Total protein | 8.2±9.07 | 6.9±0.68 | 0.344 |
| Albumin | 3.66±0.45 | 3.74±0.38 | 0.240 |
| Na | 138.2±2.5 | 138.3±2.74 | 0.936 |
| K | 4.1±0.4 | 4.1±0.4 | 0.455 |
| AST (U/l) | 49.9±54.4 | 48.0±56.6 | 0.845 |
| ALT (U/l) | 30.0±16.9 | 31.6±16.9 | 0.570 |
| Total cholesterol (mg/dl) | 199.7±37.4 | 204.0±33.1 | 0.486 |
| Triglycerides (mg/dl) | 197.9±50.7 | 196.7±62.5 | 0.896 |
| HDL (mg/dl) | 37.4±7.2 | 34.6±7.8 | 0.027 |
| LDL (mg/dl) | 122.1±34.7 | 130.0±34.5 | 0.185 |
| Monocytes (103/μl) | 0.62±0.15 | 0.71±0.24 | 0.003 |
| MHR | 1.71±0.47 | 2.21±0.98 | 0.001 |
| Hemoglobin (g/dl) | 14.4±1.52 | 14.8±1.76 | 0.096 |
| Platelets (103/μl) | 269.5±84.6 | 254.5±70.2 | 0.277 |
| WBC (103/μl) | 8.6±1.7 | 9.9±2.7 | 0.035 |
| Lymphocytes (103/μl) | 2.2±0.73 | 2.32±0.88 | 0.478 |
| Neutrophils (103/μl) | 5.34±1.8 | 6.5±2.64 | 0.004 |
Data are presented as mean ± standard deviation, median (interquartile range), or n (%).
ALT: alanine aminotransferase; AST: aspartate aminotransferase; CAD: coronary artery disease; HDL: high-density lipoprotein; K: potassium; LDL: low-density lipoprotein; MHR: monocyte to high-density lipoprotein cholesterol ratio; Na: sodium; STEMI: ST-elevation myocardial infarction; WBC: white blood cells.
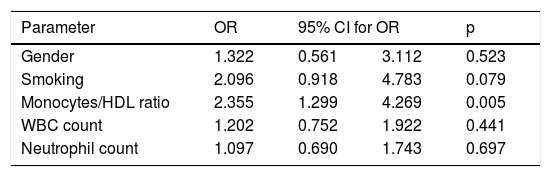
Multivariate logistic regression analysis including male gender, smoking, MHR, WBC, and neutrophil count demonstrated that MHR was the only independent predictor of STEMI (Table 2).
Independent predictors of ST-elevation myocardial infarction.
| Parameter | OR | 95% CI for OR | p | |
|---|---|---|---|---|
| Gender | 1.322 | 0.561 | 3.112 | 0.523 |
| Smoking | 2.096 | 0.918 | 4.783 | 0.079 |
| Monocytes/HDL ratio | 2.355 | 1.299 | 4.269 | 0.005 |
| WBC count | 1.202 | 0.752 | 1.922 | 0.441 |
| Neutrophil count | 1.097 | 0.690 | 1.743 | 0.697 |
CI: confidence interval; HDL: high-density lipoprotein; OR: odds ratio; WBC: white blood cell.
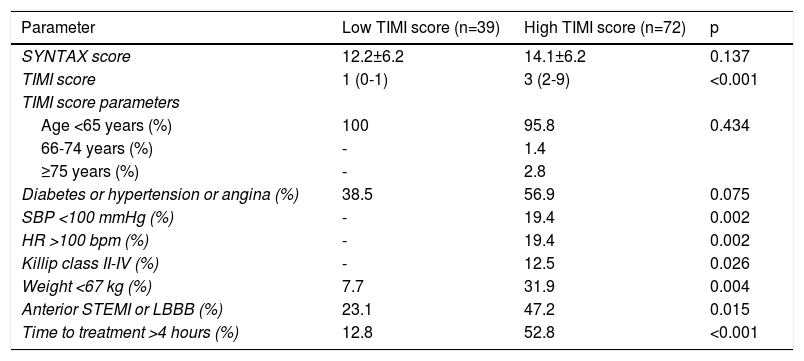
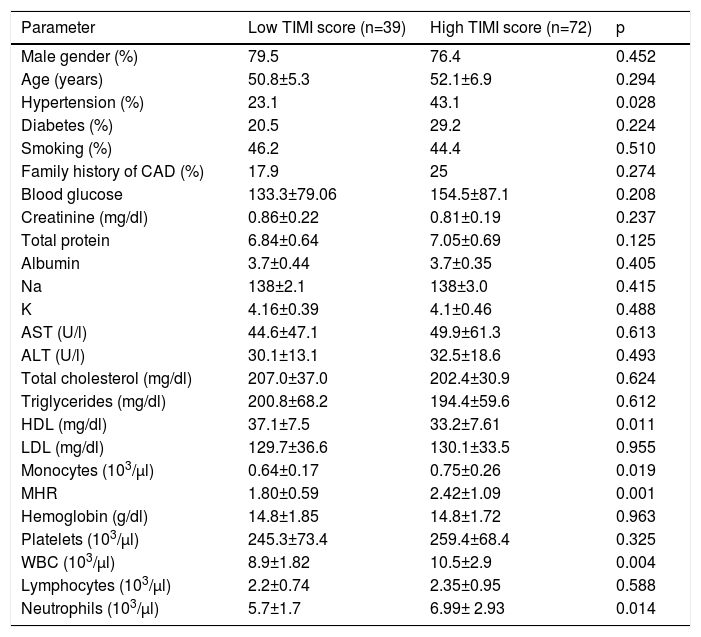
In the subgroup analysis, the 111 patients with STEMI treated by pPCI were divided into two groups according to TIMI score. There were 39 patients (31 male [79.5%]; mean age 50.8±5.3 years) in the low TIMI score group and 72 patients (55 male [76.4%]; mean age 52.1±6.9 years) in the high TIMI score group. SYNTAX scores and TIMI score parameters of the low and high TIMI score groups are shown in Table 3 and the baseline clinical and demographic characteristics of the study population based on TIMI score are shown in Table 4. The groups were similar in terms of age, gender, smoking, family history of CAD, and diabetes (p>0.05 for all) but not hypertension (p=0.028). The biochemical and hematological parameters were similar between the low and high TIMI score groups (p>0.05 for all) except for HDL-C, monocyte count, MHR, WBC and neutrophil count: HDL-C levels were significantly lower (37.1±7.5 vs. 33.2±7.61 mg/dl, p=0.011), and monocyte count (0.64±0.17 vs. 0.75±0.26×103/μl, p=0.019), MHR (1.80±0.59 vs. 2.42±1.09, p=0.001), WBC (8.9±1.82 vs. 10.5±2.9×103/μl, p=0.004) and neutrophil count (5.7±1.7 vs. 6.99±2.93×103/μl, p=0.014) were significantly higher in the high than in the low TIMI score group.
SYNTAX scores and TIMI score parameters of the low and high TIMI score groups.
| Parameter | Low TIMI score (n=39) | High TIMI score (n=72) | p |
|---|---|---|---|
| SYNTAX score | 12.2±6.2 | 14.1±6.2 | 0.137 |
| TIMI score | 1 (0-1) | 3 (2-9) | <0.001 |
| TIMI score parameters | |||
| Age <65 years (%) | 100 | 95.8 | 0.434 |
| 66-74 years (%) | - | 1.4 | |
| ≥75 years (%) | - | 2.8 | |
| Diabetes or hypertension or angina (%) | 38.5 | 56.9 | 0.075 |
| SBP <100 mmHg (%) | - | 19.4 | 0.002 |
| HR >100 bpm (%) | - | 19.4 | 0.002 |
| Killip class II-IV (%) | - | 12.5 | 0.026 |
| Weight <67 kg (%) | 7.7 | 31.9 | 0.004 |
| Anterior STEMI or LBBB (%) | 23.1 | 47.2 | 0.015 |
| Time to treatment >4 hours (%) | 12.8 | 52.8 | <0.001 |
bpm: beats per min; HR: heart rate; LBBB: left bundle branch block; SBP: systolic blood pressure; STEMI: ST-elevation myocardial infarction; TIMI: Thrombolysis in Myocardial Infarction.
Clinical and biochemical characteristics of the low and high TIMI score groups.
| Parameter | Low TIMI score (n=39) | High TIMI score (n=72) | p |
|---|---|---|---|
| Male gender (%) | 79.5 | 76.4 | 0.452 |
| Age (years) | 50.8±5.3 | 52.1±6.9 | 0.294 |
| Hypertension (%) | 23.1 | 43.1 | 0.028 |
| Diabetes (%) | 20.5 | 29.2 | 0.224 |
| Smoking (%) | 46.2 | 44.4 | 0.510 |
| Family history of CAD (%) | 17.9 | 25 | 0.274 |
| Blood glucose | 133.3±79.06 | 154.5±87.1 | 0.208 |
| Creatinine (mg/dl) | 0.86±0.22 | 0.81±0.19 | 0.237 |
| Total protein | 6.84±0.64 | 7.05±0.69 | 0.125 |
| Albumin | 3.7±0.44 | 3.7±0.35 | 0.405 |
| Na | 138±2.1 | 138±3.0 | 0.415 |
| K | 4.16±0.39 | 4.1±0.46 | 0.488 |
| AST (U/l) | 44.6±47.1 | 49.9±61.3 | 0.613 |
| ALT (U/l) | 30.1±13.1 | 32.5±18.6 | 0.493 |
| Total cholesterol (mg/dl) | 207.0±37.0 | 202.4±30.9 | 0.624 |
| Triglycerides (mg/dl) | 200.8±68.2 | 194.4±59.6 | 0.612 |
| HDL (mg/dl) | 37.1±7.5 | 33.2±7.61 | 0.011 |
| LDL (mg/dl) | 129.7±36.6 | 130.1±33.5 | 0.955 |
| Monocytes (103/μl) | 0.64±0.17 | 0.75±0.26 | 0.019 |
| MHR | 1.80±0.59 | 2.42±1.09 | 0.001 |
| Hemoglobin (g/dl) | 14.8±1.85 | 14.8±1.72 | 0.963 |
| Platelets (103/μl) | 245.3±73.4 | 259.4±68.4 | 0.325 |
| WBC (103/μl) | 8.9±1.82 | 10.5±2.9 | 0.004 |
| Lymphocytes (103/μl) | 2.2±0.74 | 2.35±0.95 | 0.588 |
| Neutrophils (103/μl) | 5.7±1.7 | 6.99± 2.93 | 0.014 |
Data are presented as mean ± standard deviation, median (interquartile range), or n (%).
ALT: alanine aminotransferase; AST: aspartate aminotransferase; CAD: coronary artery disease; HDL: high-density lipoprotein; K: potassium; LDL: low-density lipoprotein; MHR: monocyte to high-density lipoprotein cholesterol ratio; Na: sodium; STEMI: ST-elevation myocardial infarction; WBC: white blood cells.
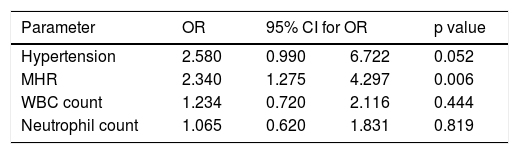
Multivariate logistic regression analysis including hypertension, MHR, WBC, and neutrophil count demonstrated that MHR was the only independent predictor of high TIMI score in patients with STEMI (Table 5). In correlation analysis, there was a significant positive correlation between MHR and TIMI score (r=0.479, p<0.001). The cutoff value of MHR for high TIMI score was 2.409, with a sensitivity of 43.06% and a specificity of 87.18% (area under the curve 0.669; 95% confidence interval 0.569-0.8769; p=0.003) on ROC curve analysis (Figure 1).
Independent predictors of high TIMI score in patients with ST-elevation myocardial infarction.
| Parameter | OR | 95% CI for OR | p value | |
|---|---|---|---|---|
| Hypertension | 2.580 | 0.990 | 6.722 | 0.052 |
| MHR | 2.340 | 1.275 | 4.297 | 0.006 |
| WBC count | 1.234 | 0.720 | 2.116 | 0.444 |
| Neutrophil count | 1.065 | 0.620 | 1.831 | 0.819 |
CI: confidence interval; MHR: monocyte to high-density lipoprotein cholesterol ratio; OR: odds ratio; WBC: white blood cell.
There were some important findings in our study. First, MHR was significantly higher in patients with STEMI and was associated with higher TIMI risk score. Second, MHR was an independent predictor of STEMI and of high TIMI score in patients with STEMI.
The TIMI score predicts mortality in STEMI patients, a TIMI score of 9 having particular short-term prognostic value. According to Walsh et al.,9 pPCI can be performed in an elderly population who have a high-risk TIMI score with low mortality and marked symptomatic benefit. The TIMI risk score is based on clinical information that is available at the time of hospital arrival and is suitable for early risk stratification at the bedside, but in the Intravenous nPA for Treatment of Infarcting Myocardium Early (InTIME II) trial, the TIMI score was not the best predictor of poor outcome because of the small sample size.10 Gonzalez-Pacheco et al. found a C-statistic of 0.80 for the predictive value of the TIMI risk score for in-hospital mortality. Also in a meta-analysis, the pooled C-statistic value for the TIMI score from 15 validation studies including 134557 patients with STEMI was 0.77.11 Intense secondary prevention improves outcomes in STEMI patients, and the RESPONSE (Randomized Evaluation of Secondary Prevention by Outpatient Nurse SpEcialists) trial showed that usual care plus six-month nursing through outpatient visits improved risk factor prevalence and reduced estimated long-term mortality risk.12 Popovic et al.13 found that the TIMI risk score has a poor discriminatory prognostic value in patients with effective early revascularization. Morrow et al.14 demonstrated C-statistic values ranging from 0.76 to 0.81 across time points. In a large American registry the accuracy of the TIMI risk score was as high as 0.80 in patients treated with pPCI. Morrow et al.15 also demonstrated that high TIMI risk scores for STEMI predict high 30-day mortality.
The inflammatory response plays an important role in the progression of atherosclerosis. Various studies have shown the association of CAD and white blood cell counts. Bath et al.16 reported that monocytes from hypercholesterolemic patients, as opposed to controls, were more sensitive to stimulation by chemoattractant agents with respect to chemokinesis. This may explain the increased involvement of monocytes in hypercholesterolemia-related atherogenesis. Murphy et al.17 reported that HDL-C and its major protein component apolipoprotein A-I exert anti-inflammatory effects on human monocytes by inhibiting the activation of CD11b. HDL-C inhibits LDL-C oxidation by reducing monocyte chemotaxis and monocyte chemoattractant protein 1 expression, and HDL-C thereby influences the inflammatory index. Kalantar-Zadeh et al.18 examined the role of HDL-C in promoting the proinflammatory potential of LDL-C in 189 patients with chronic kidney disease followed for 30 months and found a higher adjusted hazard ratio for death in patients with a higher HDL-C proinflammatory index. Besides its anti-inflammatory properties, HDL-C is also an important marker for the prognosis of cardiovascular disease.19 Kanbay et al.20 reported that MHR increased with decreasing estimated glomerular filtration rate in predialytic chronic kidney disease patients and that a higher MHR was associated with a worse cardiovascular profile and was an independent predictor of major cardiovascular events during follow-up. Recently, MHR has been described as a novel marker for major adverse outcomes with prognostic importance for predicting in-hospital and long-term major adverse cardiovascular events in STEMI patients.11,21
LimitationsThe primary limitation of the present work that it is a single-center study with a relatively small number of patients. In addition, the mean age of the study population was relatively young and all study data were collected at a single point in time, and thus may not reflect changes over time. Therefore, longitudinal studies that make comparisons over time are needed to verify these results.
All subjects in the control group had normal coronary arteries documented by coronary angiography. However, due to the study's selection criteria, some subjects in the control group may have had microvascular disease. The fact that we had many exclusion criteria also resulted in a limited number of subjects. Further studies are required for the study's findings to be applied in clinical practice.
ConclusionsThis is the first study in the literature focusing on the relationship between MHR and TIMI risk score in STEMI patients. The fact that a significant relation was found between TIMI score and MHR in this study is important. Our study added a new observation, that MHR may be valuable for prediction of in-hospital and short-term major adverse cardiovascular events in patients with STEMI.
Conflicts of interestThe authors have no conflicts of interest to declare.