This study was designed to investigate the differences in pulsatile hemodynamics, echocardiographic findings, 24-h Holter monitoring and heart rate variability parameters of dipper patterns in children with newly diagnosed essential hypertension.
MethodsThis study included 30 children with newly diagnosed essential hypertension and 30 healthy controls. The essential hypertension cohort was divided into dippers and non-dippers. Physical examinations, 24-hour ambulatory blood pressure monitoring, 24-h Holter monitoring, 24-h heart rate variability, conventional 2-dimensional and Doppler echocardiography, and tissue Doppler imaging were performed. Pulse wave analysis using an oscillometric monitor was conducted to measure augmentation index (AIx) and pulse wave velocity (PWV).
ResultsIn patients with essential hypertension, left ventricular (LV) wall thickness and LV mass index were increased. There were no significant differences in LV mass index and LV wall thickness based on the dipping patterns. Time domain values and the standard deviation of all RR intervals (SDNN) were substantially lower in the essential hypertension group. SDNN values were considerably lower in the non-dipper group compared with the dipper group. In terms of frequency domain measures, low frequency measured in daytime values was much lower in the essential hypertension group compared with the control. The dipper patterns revealed that low frequency measured in nighttime values was also substantially lower in the non-dipper group. Pulse wave analysis and AIx values were notably higher in the essential hypertension patient group and those with non-dipper status.
ConclusionSDNN values, which reflect parasympathetic activity, were markedly lower in children with hypertension and the non-dipper group than healthy controls and the dipper group, respectively. Also, parameters related to arterial stiffness, such as PWV and AIx values were significantly higher in children with hypertension and the non-dipper group.
Correlacionar, em crianças com hipertensão essencial (HE) recentemente diagnosticada, as características da onda de pulso, do ecocardiograma, do ECG dinâmico de 24 horas e de parâmetros de variabilidade da frequência cardíaca com os padrões dipper/não dipper.
MétodosEste estudo incluiu 30 crianças com HE recentemente diagnosticada e 30 controlos saudáveis. As crianças com HE foram também divididas em dois grupos: dippers e não dippers. Foi efetuado exame físico, ecocardiograma modo M. bidimensional e Doppler de fluxo e tecidular, monitoração por Holter de 24 horas, análise da variabilidade da frequência cardíaca (VFC) durante 24 horas e monitoração ambulatória da pressão arterial de 24 horas. Foi igualmente realizada a análise da onda de pulso com equipamento oscilométrico para medir o índice de aumentação (IA) e a velocidade da onda de pulso (VOP).
ResultadosOs doentes com HE apresentaram espessura parietal ventricular esquerda (VE) e índice de massa VE aumentados. Não foram registadas diferenças significativas entre o índice da massa VE e a espessura da parede e os padrões dipper/não dipper. Os valores do domínio temporal, o desvio-padrão de todos os intervalos RR (SDNN) foram significativamente inferiores no grupo com HE. Os valores SDNN foram significativamente inferiores no grupo não dipper quando comparado com o grupo dipper. Relativamente às medidas do domínio da frequência, as medições da baixa frequência (BF) efetuadas durante o dia foram significativamente mais baixas no grupo com HE do que no grupo controlo. De acordo com os padrões dipper, os valores de BF durante a noite foram também significativamente inferiores quando comparados com o grupo não dipper. A VOP e o IA foram significativamente superiores nos doentes com HE e com estado não dipper.
ConclusãoOs valores SDNN, que refletem atividade parassimpática, foram significativamente inferiores nas crianças com HE e no grupo não dipper em relaçao ao grupo controle e dipper, respetivamente. Do mesmo modo, os parâmetros relacionados com a rigidez arterial, tais como a VOP e os valores do IA, foram significativamente superiores nas crianças com HT e no grupo não dipper.
Hypertension is a chronic health problem for adults and children worldwide and appears to target all endothelial tissues, leading to multiple end-organ damage, particularly affecting the cardiovascular (CV) system. High blood pressure (BP) in childhood has been described as a risk for hypertension in early adulthood. Essential hypertension is identifiable in children and adolescents. The prevalence of high BP in children is close to 3%, and unfortunately, this figure is rising. The increasing prevalence of pediatric hypertension is particularly concerning due to the proven association between atherosclerosis and higher BP levels.1 Ambulatory blood pressure monitorization (ABPM) is more valuable than office BP for measuring BP accurately in children and adolescents, and also for evaluating pediatric cardiovascular mortality and morbidity.2 The use of ABPM has been on the rise since the publication of the first consensus recommendations for children and adolescents.3 Elevated BP is associated with various alterations in vascular structure and function. Endothelial function can be assessed by measuring aortic stiffness (AS) using a noninvasive method. Two basic measurements are used to assess AS; pulsed wave velocity (PWV) and the augmentation index (AIx).4 Aortic PWV appears to be of prognostic importance and is the gold standard for assessing central AS. The autonomic nervous system regulates heart rate and vascular tone and, thus, may contribute to increased AS in individuals with hypertension. We aimed to contribute to the literature by presenting some early indicators of hypertensive target organ damage and to detect hypertensive children who could be at greater risk of developing CV diseases.
Assessment of heart rate variability (HRV), obtained by 24-h Holter ECG monitoring, is the most frequently used noninvasive form of assessing autonomic nervous system activity. Multiple studies have demonstrated the association between HRV and CV diseases.5,6 However, while circadian rhythm disorders and changes in HRV parameters have been found in hypertensive adults, the link between childhood-onset hypertension and HRV has not yet been defined precisely.7
The major cardiac effect of hypertension is concentric hypertrophy of the left ventricle. In a hypertensive patient, pressure overload leads to an increase in wall thickness, relative wall thickness and consequently, remodeling myocardial contraction-relaxation arrangements may occur.
The primary hypothesis of this study is to demonstrate the relationship between left ventricular (LV) diastolic dysfunction, aortic elasticity impairment and reduced HRV parameters in children with hypertension compared with normotensive children. Our secondary hypothesis is to compare the HRV indices of dipper/non-dipper status, measured based on time domains.
MethodsStudy populationThis was a retrospective case control study of subjects aged 10-18 newly diagnosed with essential hypertension, monitored at the Pediatric Cardiology Department of Adana City Education and Research Hospital, Turkey. This study was conducted between November 2016 and November 2017. Thirty patients were selected over the study period and matched to a group of 30 volunteers of a similar age and gender. To minimalize the incremental effect of the pubertal stage on BP, subjects at similar stages of the Tanner scale were selected for the control group. The duration of hypertension before the diagnosis is unknown, however all the subjects were enrolled in this study before starting antihypertensive medication. Hypertensive children were recruited to the study program after detection of raised office BP by a primary care provider.
Inclusion criteria: To be enrolled in the hypertension group, subjects required manual BP measurements >95th percentile for gender and height on at least three different occasions. In cases that met this criterion, BP was then confirmed by ambulatory blood pressure (ABP) recordings based on the recommended reference values.8 Following the diagnosis of hypertension, all subjects were assessed for secondary causes according to a routine algorithm (laboratory tests, renal ultrasonography, echocardiography) to determine essential hypertension.
Exclusion criteria: Subjects with secondary hypertension, white coat hypertension, masked hypertension and ambulatory prehypertension. Children on antihypertensive medication and children with cardiac or endocrine disorders were also excluded given that if they had been included, this could have caused changes in the afterload and LV function.
The present study was conducted at the Pediatric Cardiology Department of Adana City Education and Research Hospital between November 2016 and November 2017 and the Institutional Review Board and Ethical Committee of Adana City Education and Research Hospital approved this study. Written informed consent was obtained from all participants and their parents.
Anthropometric parametersBody weight was measured using a calibrated digital scale and standing height using a Harpenden stadiometer. We used the reference intervals from the Centers for Disease Control and Prevention growth charts (https://www.cdc.gov/growthcharts/cdc_charts.htm).9
Ambulatory blood pressure measurementABP was measured between 8 and 9 am using the IEM Mobil-O-Graph New Generation blood pressure monitor. The measurements were taken at 15-min intervals from 6 am to midnight and at 30-min intervals from midnight to 6 am. We only accepted measurements of good technical quality (at least 70% of the readings had to be good technical quality taken at regular intervals during the day). Where the first 24-h ABP recording failed due to an insufficient number of readings, a second measurement was taken in the subsequent two weeks. The subjects were asked to avoid sports but to continue other normal activities, including attending school. From each ABP recording, we calculated the 24-h SBP and 24-h SBP load (percentage of readings greater than the 95th percentile over a 24-h recording).
Children with 24-h systolic or diastolic BP readings >95th percentile or BP load >25% were counted as hypertension. Children with 24-h systolic and diastolic BP <95th percentile and BP load <25% were categorized as white coat hypertension and these subjects were excluded. Healthy controls with a normal office BP and 24-h systolic and diastolic BP <95th percentile and BP load <25% were classified as normotensive.
Hypertensive subjects were also grouped based on dipping pattern. Sufficient nocturnal dipping was defined as a decrease in both the mean nighttime systolic and diastolic BP of at least 10% of the mean daytime systolic and diastolic BP.
Heart rate variabilityA three-channel 24-h Holter monitor (Risingmed, Beijing, China) was used to assess hypertensive and control groups. HRV analyzes were performed using an ECGLAB premier Holter Analyzer system and calculated automatically by the device after the manual cleaning of the artifacts. Similar to other studies, the HRV parameters were calculated during the daytime and at nighttime over 24 hours.10 The time domain analysis of HRV consisted of the standard deviation of all RR intervals (SDNN), the root mean square of the successive differences (RMSSD), and pNN50, which is the percentage of consecutive RR intervals that differ by more than 50 milliseconds.7 The frequency domain analysis of HRV consisted of the power of high frequency (0.15–0.40 Hz); low frequency (0.04–0.15 Hz).7
Pulse wave analysisMeasurement of arterial stiffness parametersArterial stiffness was measured according to international recommendations.11 Subjects who participated in this study were asked to fast for 12 hours and refrain from taking medication, drinking alcohol and caffeine for 24 hours before this study. The mean value of three consecutive measurements was calculated for each subject. Vascular measurements were taken in a supine position, in a quiet and temperature-controlled room after 15 minutes of rest (resting heart rate), using an IEM Mobil-O-Graph ARCSolver algorithm (Stolberg, Germany). This algorithm also confirms the simultaneous measurements of brachial BP, as well as AS parameters, PWV, augmentation pressure (AugP) and AIx12 PWV measurements are person-dependent and contain dynamic values. AIx is the percentage ratio of augmentation to aortic pulse pressure that represents the percentage of central pulse pressure. AIx is normalized to a recommended heart rate of 75 beats/min.
Standard echocardiographyParasternal long-axis views provided two-dimensional M-mode images and the subjects’ interventricular septum (IVS) wall thickness, LV internal diameters, and LV posterior wall thickness measurements were measured. Using the shortening fraction, we assessed LV systolic function. The Teichholz method was utilized for calculating ejection fraction. LV mass was estimated with M-mode echocardiography using Devereux's formula and indexed according to height.2,7,13 All echocardiographic measurements were taken in triplicate by the same cardiologist, who was unaware of the subject's BP. The average LV mass index values were used in the analyzes.
Statistical analysisIn cases of normal distribution, the parameters were expressed as mean ± standard deviation. Parametric (Student's t-test) and non-parametric (Mann-Whitney U) tests were performed to compare the values between the groups under examination. Comparisons between groups according to dipping patterns were calculated using the paired t-test. Statistical significance was defined as a p=<0.05. All statistical analyzes were performed using the Statistical Package for Social Sciences (version 25.0, SPSS, Inc.).14,15
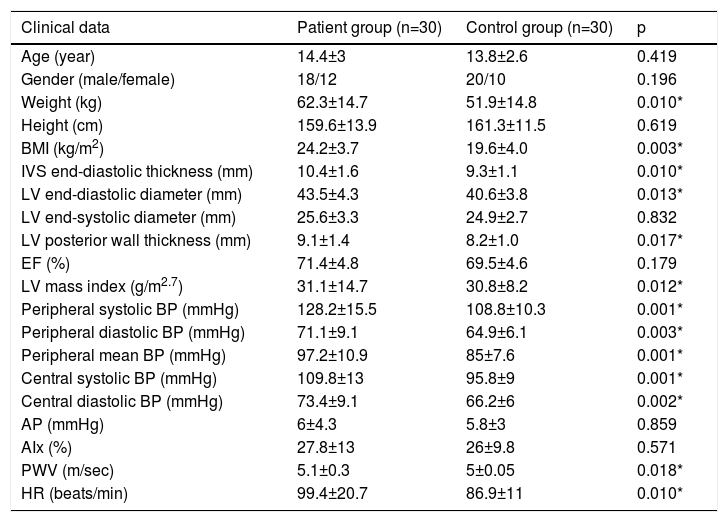
ResultsA total of 60 children with newly diagnosed essential hypertension and their healthy controls aged 10-18 years were retrospectively enrolled in the study. The 24-hour ABPM revealed 15 patients with dipper and 15 patients with non-dipper patterns. Table 1 summarizes the sample characteristics of the subjects enrolled in this study. Among the children that had office BP measurements, <95th was classified as normotensive and this was confirmed by a 24-hour ABPM. Measurements >95th were regarded as hypertensive, and this was confirmed by a 24-hour ABPM.
Clinical, echocardiographic, arterial stiffness of study groups according to patients with and without hypertension.
| Clinical data | Patient group (n=30) | Control group (n=30) | p |
|---|---|---|---|
| Age (year) | 14.4±3 | 13.8±2.6 | 0.419 |
| Gender (male/female) | 18/12 | 20/10 | 0.196 |
| Weight (kg) | 62.3±14.7 | 51.9±14.8 | 0.010* |
| Height (cm) | 159.6±13.9 | 161.3±11.5 | 0.619 |
| BMI (kg/m2) | 24.2±3.7 | 19.6±4.0 | 0.003* |
| IVS end-diastolic thickness (mm) | 10.4±1.6 | 9.3±1.1 | 0.010* |
| LV end-diastolic diameter (mm) | 43.5±4.3 | 40.6±3.8 | 0.013* |
| LV end-systolic diameter (mm) | 25.6±3.3 | 24.9±2.7 | 0.832 |
| LV posterior wall thickness (mm) | 9.1±1.4 | 8.2±1.0 | 0.017* |
| EF (%) | 71.4±4.8 | 69.5±4.6 | 0.179 |
| LV mass index (g/m2.7) | 31.1±14.7 | 30.8±8.2 | 0.012* |
| Peripheral systolic BP (mmHg) | 128.2±15.5 | 108.8±10.3 | 0.001* |
| Peripheral diastolic BP (mmHg) | 71.1±9.1 | 64.9±6.1 | 0.003* |
| Peripheral mean BP (mmHg) | 97.2±10.9 | 85±7.6 | 0.001* |
| Central systolic BP (mmHg) | 109.8±13 | 95.8±9 | 0.001* |
| Central diastolic BP (mmHg) | 73.4±9.1 | 66.2±6 | 0.002* |
| AP (mmHg) | 6±4.3 | 5.8±3 | 0.859 |
| AIx (%) | 27.8±13 | 26±9.8 | 0.571 |
| PWV (m/sec) | 5.1±0.3 | 5±0.05 | 0.018* |
| HR (beats/min) | 99.4±20.7 | 86.9±11 | 0.010* |
AIx: augmentation index; AP: augmentation pressure; BMI: body mass index (kg/m2); BP: blood pressure; EF: ejection fraction; HR: heart rate; IVS: interventricular septum; LV: left ventricular; PWV: pulse wave velocity.
Data are presented as the mean values ±SD.
*p <0.05 considered statistically significant.
The patients in this study were carefully screened and matched according to age, although weight and body mass index were appreciably higher in the hypertension group. There was no significant difference in LV ejection fraction in the groups. In the hypertension group, IVS diastolic diameter, LV end-diastolic diameter, LV posterior wall diastolic diameter, LV mass index values were considerably higher than the control group (Table 1). The 24-hour PWV parameters in patients with hypertension are shown in Table 1. There were statistically significant differences between the two groups relating to PWV, central systolic BP, peripheral systolic BP, peripheral diastolic BP, and peripheral mean BP, while central diastolic BP, AugP and AIx values were similar.
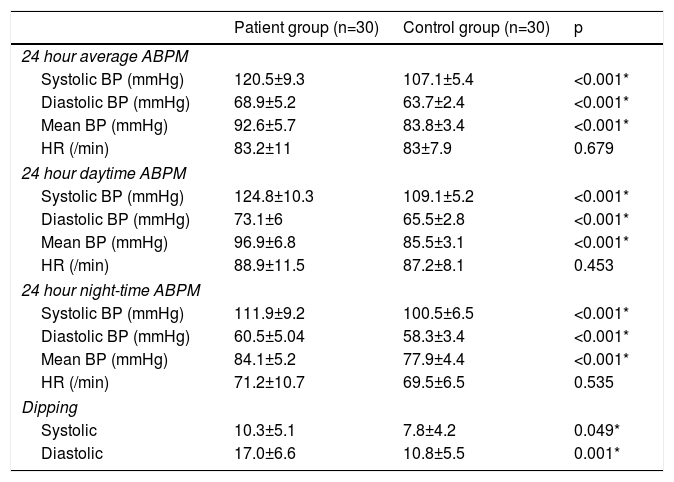
As Table 2 illustrates, mean ambulatory systolic BP, diastolic BP, mean BP and heart rate values were significantly higher in the newly diagnosed hypertension patients compared with the controls. Daytime and nighttime systolic BP, diastolic BP, mean BP and heart rate values in the hypertension patients differed compared with the normotensive group.
Ambulatory blood pressure parameters of hypertensive children and control group.
| Patient group (n=30) | Control group (n=30) | p | |
|---|---|---|---|
| 24 hour average ABPM | |||
| Systolic BP (mmHg) | 120.5±9.3 | 107.1±5.4 | <0.001* |
| Diastolic BP (mmHg) | 68.9±5.2 | 63.7±2.4 | <0.001* |
| Mean BP (mmHg) | 92.6±5.7 | 83.8±3.4 | <0.001* |
| HR (/min) | 83.2±11 | 83±7.9 | 0.679 |
| 24 hour daytime ABPM | |||
| Systolic BP (mmHg) | 124.8±10.3 | 109.1±5.2 | <0.001* |
| Diastolic BP (mmHg) | 73.1±6 | 65.5±2.8 | <0.001* |
| Mean BP (mmHg) | 96.9±6.8 | 85.5±3.1 | <0.001* |
| HR (/min) | 88.9±11.5 | 87.2±8.1 | 0.453 |
| 24 hour night-time ABPM | |||
| Systolic BP (mmHg) | 111.9±9.2 | 100.5±6.5 | <0.001* |
| Diastolic BP (mmHg) | 60.5±5.04 | 58.3±3.4 | <0.001* |
| Mean BP (mmHg) | 84.1±5.2 | 77.9±4.4 | <0.001* |
| HR (/min) | 71.2±10.7 | 69.5±6.5 | 0.535 |
| Dipping | |||
| Systolic | 10.3±5.1 | 7.8±4.2 | 0.049* |
| Diastolic | 17.0±6.6 | 10.8±5.5 | 0.001* |
ABPM: ambulatory blood pressure monitoring; BP: blood pressure; HR: heart rate.
Data are presented as the mean values ±SD.
*p <0.05 considered statistically significant.
Of the time domain measures, only the daytime SDNN values were substantially lower in the hypertension subjects compared with the normotensive subjects. The hypertensive subjects had higher time domain measurements compared with the controls, but the differences were not statistically significant. The values analyzed from the frequency domain measures included the power of low frequency, high frequency, in ms2 and normalized units (nu), and the low frequency to high frequency ratio. Only the daytime low frequency power (ms2) was significantly lower in the hypertensive subjects, whereas high frequency power (ms2), high frequency (nu), low frequency (nu) and the low frequency to high frequency ratio were comparable between the groups.
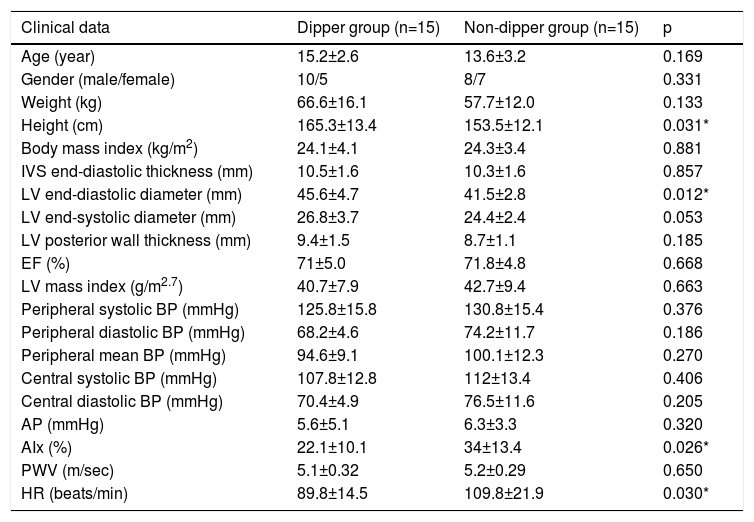
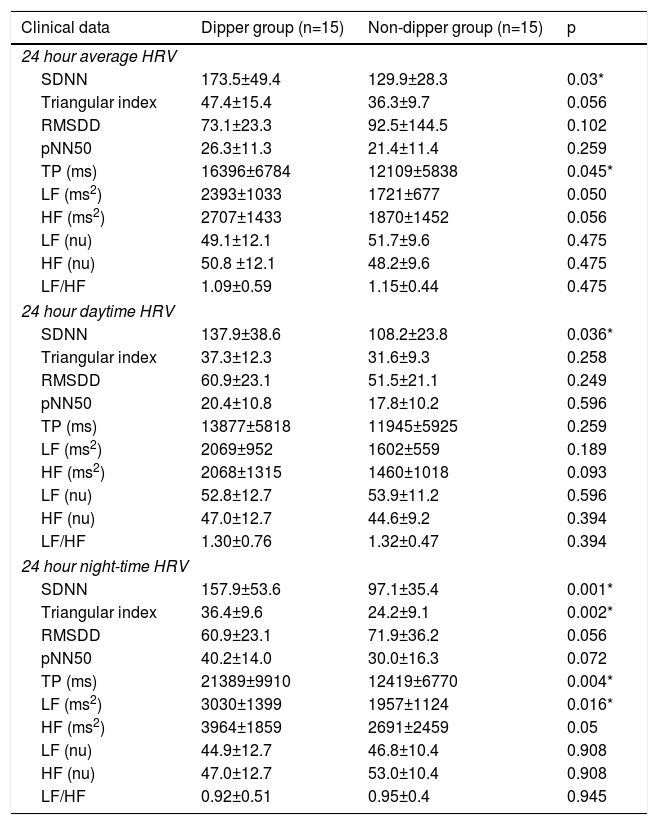
Table 3 illustrates the clinical characteristics of the hypertensive children according to dipping patterns. In the dipper group, only LV end-diastolic diameter was markedly increased (Table 3). In comparison with the dipper group, only the nighttime heart rate values were notably higher in non-dipper patients, while the other parameters of the 24-hour ABPM were similar. Only the AIx values were significantly higher in the non-dipper patients while the other parameters of the pulse wave analysis were similar (Table 3). SDNN (total, day, night), Triangular index (night), total power (TP) (total, night), low frequency ms (night) values were lower in the non-dipper group (Table 4) compared with the dipper group.
Clinical, echocardiographic, arterial stiffness features of study groups according to according to dipping pattern.
| Clinical data | Dipper group (n=15) | Non-dipper group (n=15) | p |
|---|---|---|---|
| Age (year) | 15.2±2.6 | 13.6±3.2 | 0.169 |
| Gender (male/female) | 10/5 | 8/7 | 0.331 |
| Weight (kg) | 66.6±16.1 | 57.7±12.0 | 0.133 |
| Height (cm) | 165.3±13.4 | 153.5±12.1 | 0.031* |
| Body mass index (kg/m2) | 24.1±4.1 | 24.3±3.4 | 0.881 |
| IVS end-diastolic thickness (mm) | 10.5±1.6 | 10.3±1.6 | 0.857 |
| LV end-diastolic diameter (mm) | 45.6±4.7 | 41.5±2.8 | 0.012* |
| LV end-systolic diameter (mm) | 26.8±3.7 | 24.4±2.4 | 0.053 |
| LV posterior wall thickness (mm) | 9.4±1.5 | 8.7±1.1 | 0.185 |
| EF (%) | 71±5.0 | 71.8±4.8 | 0.668 |
| LV mass index (g/m2.7) | 40.7±7.9 | 42.7±9.4 | 0.663 |
| Peripheral systolic BP (mmHg) | 125.8±15.8 | 130.8±15.4 | 0.376 |
| Peripheral diastolic BP (mmHg) | 68.2±4.6 | 74.2±11.7 | 0.186 |
| Peripheral mean BP (mmHg) | 94.6±9.1 | 100.1±12.3 | 0.270 |
| Central systolic BP (mmHg) | 107.8±12.8 | 112±13.4 | 0.406 |
| Central diastolic BP (mmHg) | 70.4±4.9 | 76.5±11.6 | 0.205 |
| AP (mmHg) | 5.6±5.1 | 6.3±3.3 | 0.320 |
| AIx (%) | 22.1±10.1 | 34±13.4 | 0.026* |
| PWV (m/sec) | 5.1±0.32 | 5.2±0.29 | 0.650 |
| HR (beats/min) | 89.8±14.5 | 109.8±21.9 | 0.030* |
AIx: augmentation index; AP: augmentation pressure; BMI: body mass index (kg/m2); BP: blood pressure; EF: ejection fraction; HR: heart rate; IVS: interventricular septum; LV: left ventricular; PWV: pulse wave velocity.
Data are presented as the mean values ±SD.
*p <0.05 considered statistically significant.
Comparison of heart rate variability parameters between dipper and non-dipper hypertensive patients.
| Clinical data | Dipper group (n=15) | Non-dipper group (n=15) | p |
|---|---|---|---|
| 24 hour average HRV | |||
| SDNN | 173.5±49.4 | 129.9±28.3 | 0.03* |
| Triangular index | 47.4±15.4 | 36.3±9.7 | 0.056 |
| RMSDD | 73.1±23.3 | 92.5±144.5 | 0.102 |
| pNN50 | 26.3±11.3 | 21.4±11.4 | 0.259 |
| TP (ms) | 16396±6784 | 12109±5838 | 0.045* |
| LF (ms2) | 2393±1033 | 1721±677 | 0.050 |
| HF (ms2) | 2707±1433 | 1870±1452 | 0.056 |
| LF (nu) | 49.1±12.1 | 51.7±9.6 | 0.475 |
| HF (nu) | 50.8 ±12.1 | 48.2±9.6 | 0.475 |
| LF/HF | 1.09±0.59 | 1.15±0.44 | 0.475 |
| 24 hour daytime HRV | |||
| SDNN | 137.9±38.6 | 108.2±23.8 | 0.036* |
| Triangular index | 37.3±12.3 | 31.6±9.3 | 0.258 |
| RMSDD | 60.9±23.1 | 51.5±21.1 | 0.249 |
| pNN50 | 20.4±10.8 | 17.8±10.2 | 0.596 |
| TP (ms) | 13877±5818 | 11945±5925 | 0.259 |
| LF (ms2) | 2069±952 | 1602±559 | 0.189 |
| HF (ms2) | 2068±1315 | 1460±1018 | 0.093 |
| LF (nu) | 52.8±12.7 | 53.9±11.2 | 0.596 |
| HF (nu) | 47.0±12.7 | 44.6±9.2 | 0.394 |
| LF/HF | 1.30±0.76 | 1.32±0.47 | 0.394 |
| 24 hour night-time HRV | |||
| SDNN | 157.9±53.6 | 97.1±35.4 | 0.001* |
| Triangular index | 36.4±9.6 | 24.2±9.1 | 0.002* |
| RMSDD | 60.9±23.1 | 71.9±36.2 | 0.056 |
| pNN50 | 40.2±14.0 | 30.0±16.3 | 0.072 |
| TP (ms) | 21389±9910 | 12419±6770 | 0.004* |
| LF (ms2) | 3030±1399 | 1957±1124 | 0.016* |
| HF (ms2) | 3964±1859 | 2691±2459 | 0.05 |
| LF (nu) | 44.9±12.7 | 46.8±10.4 | 0.908 |
| HF (nu) | 47.0±12.7 | 53.0±10.4 | 0.908 |
| LF/HF | 0.92±0.51 | 0.95±0.4 | 0.945 |
HF: high frequency; HRV: heart rate variability, LF: low frequency; RMSSD: adjacent RR intervals; SDNN: standard deviation of all RR intervals; TP: total power.
Data are presented as the mean values ±SD.
*p <0.05 considered statistically significant.
Essential hypertension is one of the major predictors of atherosclerosis and a risk factor for CV disease in both children and adults. The present study aims to show some of the early changes in hypertensive CV indices to detect clinical significance. Body weight, lipid disorders, diet and life style all play an important role in hypertension. Cardiac hypertrophy, observed in adults with hypertension, have also been detected in children. LV posterior wall and septal hypertrophy, as well as diastolic LV enlargement, are thought to exist in children with hypertension. In our study, similar to previous reports, M-mode echocardiography in the hypertensive group revealed an increase in diastolic septal, posterior wall and LV internal diameters.16 LV hypertrophy is the most significant factor in target organ damage among hypertensive children and has a prevalence of 10% to 38%.17
Reduced arterial stiffness or arterial compliance is an important factor in high BP. Therefore, we investigated whether PWV was higher in our hypertensive children compared with the controls. PWV measurements were higher in the hypertensive group, demonstrating statistical significance. These results corroborate the findings of some published studies.4
This study was designed to demonstrate whether there was any variation in the cardiovascular autonomic function of children with newly diagnosed hypertension. Huikuri et al. were the first to demonstrate the circadian rhythm of HRV parameters in healthy subjects.18 A comparison between the hypertension and control group showed that the SDNN (total-day-night), RMSDD (total-day-night), PN50 (total-day-night) parameters were all reduced, however only the SDNN daytime value from the time domain variables was statistically lower in hypertensive children. From the time domain analysis, the strongest prognostic parameter for heart disease is reported to be SDNN.19 The findings in the time domain parameters can be explained due to healthy subjects having higher fluctuations in heart rate. Thus, the time domain analysis of HRV showed decreased parasympathetic activity in hypertension children.
Frequency domain measures revealed that low frequency power (ms2) (total-day-night) and high frequency power (ms2) (total-day-night) parameters were reduced, but only daytime low frequency power (ms2) values were considerably lower in hypertensive children. However, there was no statistical significance between high frequency (ms2), low frequency (nu), high frequency (nu) and low frequency/high frequency values between the groups. Our findings show the loss of parasympathetic tone in subjects with newly diagnosed essential hypertension, as demonstrated by previous reports on the matter.7,10,20
This study aims to evaluate the HRV parameters between the dipper and non-dipper groups. An insufficient lowering of nocturnal BP is related to CV mortality, and the existence of non-dipping patterns is associated with CV damage in most patients. In essential hypertension, as well as LV hypertrophy and early LV dysfunction, patients with non-dipper patterns are at a high risk of end-organ damage, which is relevant to adverse cardiac remodeling.21
The absolute power of the low frequency component (ms2) decreased slightly during the daytime in the hypertension group and according to dipper patterns, low frequency (night) decreased in the non-dipper group, while the normalized units of low frequency (nu) were similar. Normalization serves to attenuate the effect on the values of low frequency and high frequency component of the changes in TP.22 Low frequency appears to be affected by both the vagal and the sympathetic nerves. The low frequency/high frequency ratio is thought to indicate sympathovagal balance and functions as a marker of sympathetic nerve activity. Low frequency (nu) is also considered to be a sign of sympathetic nerve function.18 Concerning the frequency domain analysis, it has been observed that children with hypertension have decreased cardiac parasympathetic activity but not sympathetic activity. There is also some evidence in the literature of a decreasing low frequency trend in untreated non-dipper hypertensive subjects.23 A comparison of the dipping patterns seems relevant as its role in n the decrease in nighttime BP has been demonstrated. There are, however, few studies comparing the two groups.
A comparison of the daytime and nighttime low frequency, SDNN and TP values between dipping groups, reveals there is a significant difference in the dipper group, while this difference is absent in the non-dipper group. These important data show the deactivation of the parasympathetic system during the night period in the non-dipper group.
The differences between hypertensive and normotensive children are similar to previous reports on HRV.24 In our study, it appears that parasympathetic withdrawal is primarily responsible for these results, rather than sympathetic overdrive. As a supporting factor, the lack of significant alteration in the sympathetic system parameters is also an important finding. Although the non-significant results on the sympathetic system have previously been interpreted as being due to antihypertensive therapy, our subjects did not receive medical treatment.25 Although it is not routinely used to evaluate sympathovagal balance in clinical assessment, HRV may lead to an early autonomic assessment of the disorder at the time of diagnosis. However, we have no idea whether the ongoing period with higher BP and HRV parameters, which demonstrates alterations in the autonomic nervous system, may help to predict this period in newly diagnosed hypertension patients. Further studies are required to determine this prognosis in hypertension patients.
ConclusionAs CV disease is clinically silent in the early stages, essential hypertension is often asymptomatic. However, cardiovascular hypertrophy begins to develop in the early stages of hypertension. To reduce CV morbidity, early echocardiographic screening is required in hypertensive adolescents before the progression to CV disease. The circadian patterns of HRV could be useful in medical management and for assessing treatment response. Our study highlights the need for a more extensive model of central autonomic control.
FundingThis research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of interestThe author has no conflicts of interest to declare.