Atherosclerosis is an active process and the inflammatory component appears to be particularly correlated with the development of acute coronary syndromes (ACS). C-reactive protein (CRP) is an acute phase protein that appears in the circulation in response to inflammatory cytokines. The present study investigated the association between high-sensitivity C-reactive protein (hsCRP) on admission and follow-up prognosis after an ACS.
MethodsWe included 151 consecutive patients admitted to the coronary care unit with a diagnosis of ACS (47% ST-segment elevation myocardial infarction [STEMI]). The primary endpoint was the combination of cardiac death and myocardial reinfarction during the follow-up period (median 19.8 months, interquartile range 16.3–23.7 months).
ResultsThe occurrence of follow-up events was significantly related to admission hsCRP level, which was an excellent predictor of cardiac death and reinfarction during follow-up (HR 1.091, 95% CI 1.014–1.174; p=0.019). Stratifying the population based on type of ACS, adjusted by variables associated with cardiac events in univariate analysis (hsCRP, diabetes, depressed ejection fraction and GRACE risk score), hsCRP proved to be an independent predictor of follow-up outcomes only in non-STEMI patients (HR 1.217, 95% CI: 1.093–1.356, p<0.001), not in STEMI patients. The best cutoff level of hsCRP to predict follow-up outcomes was 1.1mg/dl, with sensitivity of 77.8% and specificity of 63.2%.
ConclusionAlthough the GRACE risk score is routinely used for stratification of patients with ACS, assessment of hsCRP may provide additional prognostic value in the follow-up of non-STEMI patients.
A aterosclerose é um processo ativo e a sua componente inflamatória parece estar particularmente relacionada com o desenvolvimento de síndromes coronárias agudas (SCA). A proteína C-reativa (PCR) é uma proteína que aparece na circulação, na fase aguda do processo inflamatório. O presente estudo teve como objetivo analisar a associação entre o valor do teste de alta sensibilidade da proteína C-reativa (PCR-as) na admissão, com o prognóstico no seguimento, em doentes pós-SCA.
MétodosForam incluídos 151 doentes consecutivos, internados na unidade de cuidados coronários, com diagnóstico de SCA (47% com enfarte agudo do miocárdio com elevação do segmento ST – STEMI). O end-point estudado foi a variável composta pela morte associada a patologia cardíaca e re-enfarte miocárdio durante o período de seguimento (mediana de 19,8 meses, intervalo interquartil 16,3-23,7 meses).
ResultadosA ocorrência de eventos apresentou uma forte relação com o valor de CPR-as registado na admissão, sendo por isso considerado como um bom preditor para a ocorrência de morte associada a patologia cardíaca e a re-enfarte no período de seguimento de doentes pós-SCA (HR 1,091, CI 95% 1,014-1,174; p=0,019). Após estratificação da população pelo tipo de SCA e ajustando as variáveis associadas à ocorrência de eventos cardíacos (análise univariada das variáveis valor de PCR-as, diabetes mellitus, fração de ejeção deprimida e score de risco GRACE), o valor de PCR-as destacou-se como preditor independente no seguimento dos doentes com EAM sem elevação ST (HR 1,217, IC 95%: 1,093-1,356, p<0,001). O valor de cut-off para o nível de PCR-as preditor foi de 1,1mg/dl, com uma sensibilidade de 77,8% e uma especificidade de 63,2%.
ConclusãoApesar de o score de risco GRACE ser utilizado, por rotina, para estratificar os doentes com SCA, a medição do valor de PCR-as pode acrescentar valor prognóstico no seguimento de doentes com EAM sem elevação e ST.
acute coronary syndrome
C-reactive protein
high-sensitivity C-reactive protein
left ventricular ejection fraction
non-ST-elevation acute coronary syndrome
ST-elevation myocardial infarction
Inflammation plays a pivotal role in the pathogenesis of atherosclerosis and its complications. In particular, atherosclerosis is an active process and the inflammatory component appears to be particularly correlated with the development of acute coronary syndromes (ACS).1,2 C-reactive protein (CRP) is an acute phase protein that appears in the circulation in response to inflammatory cytokines, such as interleukin-6, and serves as a biomarker for systemic inflammation.3,4 There are also increased concentrations of acute-phase serum reactants such as CRP in patients with ACS.5
The high-sensitivity CRP (hsCRP) assay is increasingly used as a marker for cardiac risk assessment and as a prognostic tool in heart disease.6–8 The aim of this study was to analyze the prognostic value of hsCRP values to predict follow-up outcomes in ACS patients regardless of the GRACE (Global Registry of Acute Coronary Events) risk score.6
MethodsStudy populationWe included 151 consecutive patients admitted to the coronary care unit with a diagnosis of ACS. Patients with previous ACS, peripheral arterial disease and impaired renal function (estimated glomerular filtration rate by the MDRD-4 equation <60ml/min/1.73m2) were excluded. We also excluded patients under treatment with anti-inflammatory drugs and those with concomitant inflammatory diseases, cancer, or other significant heart disease. The study was approved by the ethics committee of the University Clinical Hospital of Santiago de Compostela, and all patients gave their written informed consent to participate.
Study designAll patients were treated invasively by catheterization. The use of beta-adrenergic blocking agents, angiotensin-converting enzyme inhibitors, antiplatelets, diuretics and inotropic drug support was left to the discretion of the coronary care unit cardiologists according to our clinical protocols based on international guidelines. For each patient we estimated the risk of follow-up mortality and coronary events according to the 6-month mortality GRACE score.6 Complete clinical data and blood samples for laboratory measurements were collected on admission. We performed an echocardiographic evaluation of left ventricular ejection fraction (LVEF) in all subjects within 24hours of admission. Serum hsCRP levels were measured on admission.
Definitions and endpointsThe ACS diagnosis was validated if the patient met any of the following criteria: new-onset angina with cardiac biomarkers above the highest normal laboratory limit, ST-segment deviation on the electrocardiogram, in-hospital stress testing showing ischemia, or a known history of coronary disease. Patients were classified as having myocardial infarction with ST-segment elevation (STEMI) or non-ST-segment elevation ACS (NSTE-ACS) (unstable angina or non-ST elevation myocardial infarction). Diabetes was defined as increased fasting plasma glucose concentration of ≥126mg/dl, HbA1c of ≥6.5%, or treatment with insulin or hypoglycemic agents. Hypertension was defined as systolic/diastolic blood pressure>140/90mmHg or current use of any antihypertensive medication. LVEF<45% was considered to be depressed.
The primary endpoint was the combination of cardiac death and myocardial reinfarction during the follow-up period (median 19.8 months, interquartile range 16.3–23.7 months). Reinfarction was defined as the appearance of new symptoms of myocardial ischemia or electrocardiographic ischemic changes accompanied by re-elevation of cardiac biomarkers (high-sensitivity troponin I).
Determination of CRPBlood samples were stored in evacuated tubes at −20°C and were processed within 24hours by automated microparticle immunoassay (ELISA). The CRP detection range corresponds to values of 0.1–12.0mg/dl, with an interassay variation coefficient of <5% (normal values<0.3mg/dl).
Statistical analysisAll information was prospectively recorded in a database created with Microsoft Office Access 2007. The statistical analyses were performed with SPSS (Statistical Package for the Social Sciences) version 17.0. Categorical or dichotomous variables are expressed as absolute values and percentages, and were compared with Pearson's chi-square test. Continuous variables with a normal distribution are expressed as mean±standard deviation, and the Student's t test was used for comparisons between groups. Continuous variables without normal distribution are expressed as median and interquartile range. Pearson's test was used to study the correlation between quantitative variables. A multivariate logistic regression model was used to evaluate the independent contribution of hsCRP levels to the risk of new events during follow-up. Univariate predictors of potential significance and hsCRP values were included in multivariate analysis (backward stepwise Cox proportional hazard analysis). Adjusted hazard ratios and 95% confidence intervals (CI) are presented. Kaplan–Meier curves were constructed to evaluate the prognostic value of hsCRP during follow-up. A p value<0.05 was considered statistically significant.
ResultsBaseline characteristicsTable 1 describes the baseline characteristics of the population. CRP values (median and 25–75% interquartile range) on admission were 0.9 (0.3–1.9)mg/dl. Of the patients recruited, 80 had STEMI. Although hsCRP values were higher in patients with STEMI (2.6±4.2mg/dl), there was no statistically significant difference compared with NSTE-ACS patients (1.8±2.9mg/dl, p=0.161).
Baseline characteristics and comparison between groups with and without cardiac events.
| Variable | All patients | Cardiac events | Non-cardiac events | p |
| Age (years) | 62.5±13.6 | 67.6±14.6 | 61.9±13.4 | 0.095 |
| Female | 24.5 | 16.7 | 25.6 | 0.416 |
| Diabetes | 27.2 | 50.0 | 24.1 | 0.020 |
| Hypertension | 44.3 | 56.3 | 42.9 | 0.308 |
| STEMI | 47.0 | 50.0 | 46.6 | 0.787 |
| Killip>I | 11.3 | 27.8 | 9.0 | 0.018 |
| LVEF<45% | 15.9 | 50.0 | 11.3 | <0.001 |
| Multivessel disease | 49.7 | 66.7 | 47.4 | 0.124 |
| PCI | 80.8 | 83.3 | 80.5 | 0.771 |
| Troponin I (ng/dl) | 46.8±81.5 | 105.0±26.2 | 77.8±7.0 | 0.151 |
| hsCRP (mg/dl) | 2.2±3.6 | 4.3±4.7 | 1.9±3.3 | 0.008 |
| GRACE risk score | 99.3±29.4 | 116.4±32.7 | 96.9±28.3 | 0.008 |
| Discharge therapy | ||||
| Aspirin | 98.0 | 94.4 | 98.5 | 0.248 |
| Clopidogrel | 86.1 | 88.9 | 85.7 | 0.715 |
| Beta-blockers | 74.8 | 66.7 | 75.9 | 0.395 |
| ACEIs/ARBs | 72.8 | 78.2 | 72.2 | 0.549 |
| Statins | 96.4 | 100.0 | 96.0 | 0.448 |
ACEIs: angiotensin-converting enzyme inhibitors; ARBs: angiotensin receptor blockers; hsCRP: high-sensitivity C-reactive protein; LVEF: left ventricular ejection fraction; PCI: percutaneous coronary intervention; STEMI: ST-elevation myocardial infarction.
During the follow-up period, 18 (11.9%) patients presented cardiac events (six cardiac deaths, 11 re-infarctions). These patients had a higher percentage of diabetes, higher Killip functional class, greater proportion of depressed LVEF and higher GRACE risk score. The occurrence of follow-up events was significantly related to admission hsCRP level, which was an excellent predictor of cardiac death and re-infarction during follow-up (HR 1.091, 95% CI 1.014–1.174; p=0.019). Stratifying the population based on type of ACS, we found that hsCRP predicted outcome only in the NSTE-ACS group (HR 1.174, 95% CI 1.076–1.280; p=0.004), not in patients with STEMI (HR 0.999, 95% CI 0.859–1.163; p=0.990). Likewise hsCRP and GRACE risk score at discharge showed a significant positive correlation (r=0.226, p=0.005) (Figure 1).
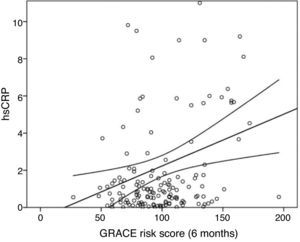
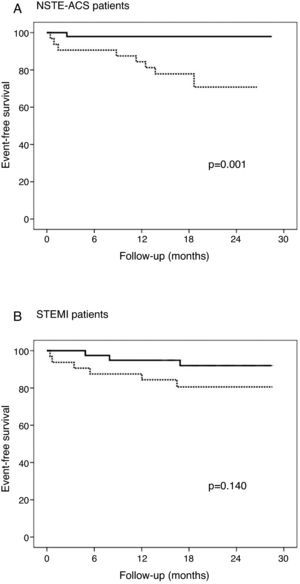
In ROC analysis, the area under the curve for hsCRP in predicting follow-up outcomes was 0.75±0.05. The best cutoff level of hsCRP was 1.1mg/dl, with sensitivity of 77.8% and specificity of 63.2% (Figure 2). Figure 3 shows the Kaplan–Meier survival curves according to hsCRP levels above and below this cutoff (1.1mg/dl).
In our model (Table 2), adjusted by variables associated with cardiac events (hsCRP, diabetes, depressed LVEF and GRACE risk score), hsCRP (as a continuous variable) was an independent predictor of follow-up outcomes only in NSTE-ACS patients (HR 1.217, 95% CI: 1.093–1.356, p<0.001).
Multivariate analysis.
| Variable | NSTE-ACS | STEMI | ||
| OR (95% CI) | p | OR (95% CI) | p | |
| Diabetes | 1.134 (0.231–5.567) | 0.877 | 5.079 (1.407–22.914) | 0.015 |
| LVEF<45% | 1.514 (0.287–7.899) | 0.625 | 7.177 (1.787–28.826) | 0.005 |
| GRACE risk score | 1.028 (1.008–1.048) | <0.001 | 1.014 (0.994–1.033) | 0.366 |
| hsCRP | 1.217 (1.093–1.350) | 0.007 | 0.934 (0.806–1.083) | 0.166 |
hsCRP: high-sensitivity C-reactive protein; LVEF: left ventricular ejection fraction; NSTE-ACS: non-ST-elevation acute coronary syndrome; STEMI: ST-elevation myocardial infarction.
In this single-center study we showed that hsCRP was significantly associated with adverse follow-up outcomes in patients with NSTE-ACS, independently of GRACE risk score, but not in patients with STEMI.
Many studies have assessed the prognostic value of CRP in the hospital phase of ACS.9–12 However, fewer studies have examined its prognostic value in follow-up, and very few have investigated its prognostic role over the entire spectrum of ACS patients, classified as NSTE-ACS or non-STEMI.
The hypothesis that inflammatory reactions promote plaque fissuring, erosion, ulceration, and rupture of the plaque surface should in most cases be applicable to both settings of ACS.13,14 They may share the same underlying pathophysiologic processes, with coronary plaque disruption and consequent platelet aggregation and thrombosis. However, the differences found in our study between the two types of ACS were in agreement with previous studies in which hsCRP was a predictor of negative outcome, especially in patients with unstable angina and non-STEMI. Kuch et al.15 reported data on an unselected sample of patients with myocardial infarction admitted to a community hospital, showing that CRP was significantly associated with adverse short-term outcome. Their multivariate analysis showed that both troponin positivity and CRP positivity were associated with a 2-fold increased risk of dying within 28 days after the acute event for all patients with myocardial infarction. Stratifying by myocardial infarction type showed that in patients with STEMI, troponin positivity, but not CRP positivity, independently predicted 28-day case fatality, while in patients with non-STEMI, CRP positivity, but not troponin positivity, predicted outcome. They concluded that admission CRP is a powerful parameter for risk stratification of patients with myocardial infraction, with better stratification in patients with non-STEMI.
Morrow et al., using a cutoff of 1.5mg/dl (similar to ours), observed that elevated CRP at admission was associated with higher mortality at 14 days. Schoos et al.16 demonstrated that preprocedure hsCRP is an independent and strong predictor of a composite endpoint of death, nonfatal recurrent myocardial infarction, and stent thrombosis after percutaneous intervention with coronary stent implantation. Abbate et al. confirmed the prognostic value of CRP in predicting short- and long-term outcomes after ACS. Our group has shown that hsCRP was a predictor of adverse outcomes in the in-hospital phase of ACS independently of GRACE risk score. However, to date, no studies have analyzed the follow-up prognostic value of hsCRP regardless of GRACE risk score at discharge.
There is an intracardiac inflammatory response in ACS that appears to be the result of the evolution of myocardial necrosis, as shown by higher CRP, TNFα and IL-6 levels in patients with major adverse cardiac events. Patients with ACS and higher CRP may represent a group with hyperresponsiveness of the inflammatory system, which might exaggerate the acute-phase reaction and increase immune system activation, which may in turn mediate myocardial damage and promote cardiac complications.17–20 This may be more pronounced in patients with NSTE-ACS than in those with STEMI, due to a higher atherosclerotic burden.
hsCRP measurement, as a marker of inflammatory activity, has several advantages. Firstly, it is a stable compound and secondly, it can be measured at any time of day without regard for the biological clock, since unlike measurements of cytokines such as IL-6, no circadian variation appears to exist for hsCRP.
ConclusionsAlthough the GRACE risk score is routinely used for stratification of patients with acute coronary syndrome, assessment of hsCRP may provide additional prognostic value. High hsCRP values were an independent and strong predictor of a composite endpoint of death and nonfatal recurrent myocardial infarction. These findings highlight the importance of determining levels of this biomarker for risk stratification of these patients during follow-up.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors have no conflicts of interest to declare.
We thank the medical residents and nurses of the coronary cardiac unit of the University Clinical Hospital of Santiago de Compostela for their assistance in this study.








 hsCRP: high-sensitivity C-reactive protein.'/>
hsCRP: high-sensitivity C-reactive protein.'/>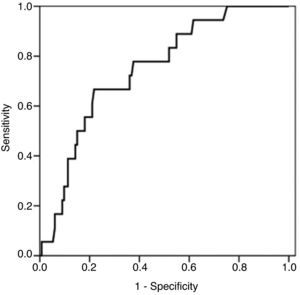
 NSTE-ACS: non-ST-elevation acute coronary syndrome;
NSTE-ACS: non-ST-elevation acute coronary syndrome; 

