In Portugal, the first heart transplantation (HT) was performed in 1986 by Prof. Queiroz e Melo, and the first kidney transplantation (KT) dates back to 1969 (Prof. Linhares Furtado). By September 2019, a total of 13 811 KTs and 838 HTs had been performed in this country. Despite significant advances in transplantation, allograft failure remains one of the most frequent causes of death after HT, and only a selected few undergo heart retransplantation (HrT) – 2-3% of HTs performed yearly worldwide are HrTs1 – in part due to the organ donor shortage and suboptimal results. Chronic kidney disease (CKD) is another frequent and late complication, which independently predicts all-cause death.2 In this letter, we present the first case of HrT with KT performed in Portugal.
A 34-year-old Portuguese male with Becker muscular dystrophy, presenting with mild proximal muscular weakness and dilated cardiomyopathy, underwent HT at our center in 2001. He developed cardiac allograft vasculopathy (CAV) and had an anterior myocardial infarction not amenable to revascularization in 2018. Over the next year, severe allograft failure and advanced heart failure (HF) ensued (Interagency Registry for Mechanically Assisted Circulatory Support [INTERMACS] profile 4), and progressive CKD rendered him dialysis-dependent. A cardioverter-defibrillator was implanted for primary prevention of sudden cardiac death, after maximally tolerated guideline-directed medical therapy failed to improve left ventricular ejection fraction and HF symptoms.
Given his young age at the time (52 years) and advanced HF (no late rejection International Society for Heart and Lung Transplantation [ISHLT] grade>1R) he was assessed for HrT. Low pulmonary vascular resistance (2 Wood units), low cardiac output (1.7 l/min/m2) and VO2 max of 6.8 ml/kg/min on maximum effort were noted. The Seattle Heart Failure Model predicted a one-year survival of <50%. Cancer screening testing was negative, and no peripheral arterial disease was documented on carotid and proximal inferior limb ultrasound. The patient maintained a socially active life and there were no findings of progressive dystrophinopathy-related musculoskeletal impairment. Following multidisciplinary discussion, he was listed for double organ transplantation in September 2019.
In January 2020, he underwent successful HT and KT, receiving both organs from a single donor. He was discharged home one month later on a prednisolone tapering regimen, tacrolimus and mycophenolate mofetil, plus antimicrobial prophylaxis, as per transplantation protocol. By the three-month follow-up, he had resumed normal daily activities. Serial heart biopsies showed no signs of rejection, while normal biventricular and renal function was sustained (creatinine 0.84 mg/dl).
HrT may be considered for patients with CAV and refractory allograft failure, without ongoing rejection (class IIa recommendation, level of evidence C).2 While one-year outcomes were comparable to a matched cohort of first-time recipients,3 registries have suggested lower long-term survival in those listed for HrT (median 8.2 vs. 11.6 years for first HT4). Moreover, a registry revealed numerically more rejections (although not statistically significant) in HrT compared to primary HT.1 However, while irreversible severe CKD (estimated glomerular filtration rate <30 ml/min/m2) is a relative contraindication for isolated HT (class IIa recommendation, level of evidence C),2 double organ heart-kidney transplantation could be a life-saving option for these patients. A retrospective cohort of 1660 HrT patients, 116 of whom received KT, showed improved survival in the latter, especially in cases of severe CKD at baseline.5
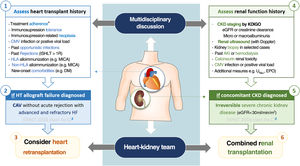
Here we report the first case of HrT combined with KT performed in Portugal. HrT may be considered in well-selected cases (Figure 1), particularly in patients with CAV and few comorbidities. Combined heart-kidney transplantation may be considered in those with concurrent severe CKD.
Candidate selection for heart retransplantation combined with renal allograft. AKI: acute kidney injury; CAV: coronary artery vasculopathy; CKD: chronic kidney disease; CMV: cytomegalovirus; DM: diabetes mellitus; eGFR: estimated glomerular filtration rate; EPO: erythropoietin; HF: heart failure; ISHLT: International Society for Heart and Lung Transplantation; HLA: human leukocyte antigen; KDIGO: Kidney Disease Improving Global Outcomes; MICA: MHC class I-related chain A; UNa+: urinary sodium. * includes both pharmacological and non-pharmacological (e.g. smoking and/or alcohol cessation) treatment.
BR wrote the first draft of this article; BR, CB, GC, CS and CA incorporated feedback in subsequent drafts and revisions; SR, AT, DS, AW, MSU, MA, DM, AM, MM and JPN contributed to revisions and reviewed the final draft; BR and GC composed the figure; BR submitted the final version of this article, on behalf of all the authors.
Informed consent and ethics statementThe patient consented verbally to the publication of his medical case in the Portuguese Journal of Cardiology. Members of the transplant team (BR, CB, GC, CS, SR, AW, and CA) obtained the informed consent. This investigation was conducted in accordance with the World Medical Association's Declaration of Helsinki (seventh revision, Fortaleza, 2013) and the Declaration of Istanbul (2008). Furthermore, the authors declare that the figure within this article (algorithm for heart retransplantation combined with renal transplantation) does not enable identification of the patient. Dates were specified as month and year, days being omitted to further comply with patient confidentiality. This case report was exempt from ethics committee approval.
Conflicts of interestThe authors have no conflicts of interest to declare.