The MINERVA trial established that atrial preventive pacing and atrial antitachycardia pacing (DDDRP) in combination with managed ventricular pacing (MVP) reduces progression to permanent atrial fibrillation (AF) in patients with paroxysmal or persistent AF and bradycardia who need cardiac pacing, compared to standard dual-chamber pacing (DDDR). It was shown that AF-related health care utilization was significantly lower in the DDDRP + MVP group than in the control group. Cost analysis demonstrated significant savings related to this new algorithm, based on health care costs from the USA, Italy, Spain and the UK.
ObjectiveTo calculate the savings associated with reduced health care utilization due to enhanced pacing modalities in the Portuguese setting.
MethodsThe impact on costs was estimated based on tariffs for AF-related hospitalizations and costs for emergency department and outpatient visits in Portugal.
ResultsThe MINERVA trial showed a 42% reduction in AF-related health care utilization thanks to the new algorithm. In Portugal, this represents a potential cost saving of 2323 euros per 100 patients in the first year and 17118 euros over a 10-year period. Considering the number of patients who could benefit from this new algorithm, Portugal could save a total of 75369 euros per year and 555410 euros over 10 years. Additional savings could accrue if heart failure and stroke hospitalizations were considered.
ConclusionThe combination of atrial preventive pacing, atrial antitachycardia pacing and an algorithm to minimize the detrimental effect of right ventricular pacing reduces recurrent and permanent AF. The new DDDRP + MVP pacing mode could contribute to significant costs savings in the Portuguese health care setting.
Observamos no estudo MINERVA que a prevenção de pacing auricular e antitaquicardia (DDDRP), em combinação com algoritmos de redução de pacing ventricular (MVP), reduzem a fibrilhação auricular (FA) permanente em doentes com bradicardia, com FA permanente ou paroxística que necessitam de pacing cardíaco, quando comparado com a estimulação elétrica de dupla câmara (DDDR). De igual forma, a utilização de recursos hospitalares foi significativamente menor no grupo DDDRP+MVP comparativamente ao grupo de controlo.
ObjetivoCalcular as poupanças associadas à menor utilização de recursos hospitalares em Portugal com a utilização deste novo algoritmo.
MétodosO impacto nos custos foi estimado considerando o preço definido para a hospitalização associada à FA, o custo da urgência e das consultas em Portugal.
ResultadosFoi estimada uma redução de 42% na utilização de recursos hospitalares com o novo algoritmo. Em Portugal, este resultado representa uma poupança de 2.323€ por cada 100 doentes no primeiro ano de utilização e um total de 17.118€ ao final de dez anos. Considerando o número de doentes que podem beneficiar deste algoritmo, existe um potencial de poupança de 75.369€ por ano e de 555.410€ em dez anos. Estas poupanças poderão ser superiores se forem considerados os custos de hospitalização decorrentes da insuficiência cardíaca e AVC.
ConclusãoA combinação de prevenção de pacing auricular e antitaquicardia e algoritmos de redução de pacing ventricular reduzem a FA permanente ou recorrente. Estes novos algoritmos de pacing podem contribuir de forma significativa para a redução dos custos hospitalares relacionados com FA em Portugal.
Atrial fibrillation (AF) is the most common sustained cardiac arrhythmia encountered in clinical practice. Paroxysmal and persistent AF affect about 2.2 million individuals in North America and 4.5 million in the European Union.1,2 In Portugal, the prevalence of AF is estimated at 2.5% in individuals aged over 40 years but is higher in older age groups: 9% in those aged over 65 and 10.4% in those aged over 80 years. The condition is not identified in around 36% of these patients.3,4 Gender differences are not significant.3
Since AF occurs more frequently with age, a significant rise in the incidence of patients suffering from the condition is expected as populations age.5,6
AF is especially common among bradycardia patients, one third of whom have a history of AF or are diagnosed with AF at pacemaker implantation or during follow-up.7,8 It is estimated that 1 million pacemakers were implanted in 2009 worldwide, meaning that more than 333000 individuals with pacemakers may suffer from AF.9
AF accounts for approximately one third of hospitalizations due to cardiac rhythm disturbances, with a clear upward trend worldwide. Data from the USA demonstrate that hospitalization rates increased by 23% in patients with AF from 2000 to 2010, particularly in the elderly.10 AF also increases the risk of stroke and heart failure.11,12
A new pacemaker algorithm that includes managed ventricular pacing (MVP) and atrial preventive pacing and atrial antitachycardia pacing (DDDRP) has been developed to minimize the detrimental effect of right ventricular pacing, with the aim of reducing AF and related health care costs. The international MINERVA (MINimizE Right Ventricular pacing to prevent Atrial fibrillation and heart failure) trial13 established that the DDDRP + MVP pacing modality reduces AF. The incidence of permanent AF was considerably lower (61% risk reduction) in bradycardia patients with the new pacing algorithm than in those with standard dual-chamber pacing (DDDR).13 AF-related hospitalizations and emergency department (ED) visits also fell as a consequence.
Following the MINERVA trial, a cost-analysis study in 2015 by Boriani et al.14 estimated the health care cost savings achievable by reductions in AF-related hospitalizations and ED visits for the USA, Italy, Spain and the UK. The purpose of the present study was to estimate current and future savings arising from this new algorithm for the Portuguese health care system, using the same cost-analysis methodology as in Boriani et al.
MethodsStudy design and patient populationMINERVA was a prospective, multicenter, randomized, single-blind, controlled trial with an international scope involving 63 cardiology centers in 15 countries enrolling 1166 patients.13,15
The inclusion criteria were standard class I or II indication for dual chamber pacing and a history of at least one documented episode of AF, atrial flutter or atrial tachycardia in the last 12 months.
The objective of the MINERVA trial was to compare standard DDDR pacing with the DDDRP + MVP combination.
Economic analysis and health care costs in PortugalThe aim of Boriani et al.’s study14 was to compare health care costs in two groups: DDDRP + MVP and DDDR (controls). Three different health care services were included in the MINERVA trial: AF-related hospitalizations, ED visits, and outpatient visits, the latter defined as follow-up visits that were not mandatory in the study. The costs related to these services were not collected in the MINERVA trial; the cost analysis was performed taking into account the number of health care services that were avoided with DDDRP + MVP and an average cost associated with each health care service.
The methods for estimating costs differ from country to country depending on the availability of data. Actual hospital costs were available in the USA, while diagnosis-related group (DRG) tariffs (Spain, Italy, Portugal) or DRG reference costs (UK) were used for European countries. Moreover, although in the USA costs can be differentiated for patients with an implanted pacemaker, this is not the case in the European countries under analysis. The methods used to estimate Portuguese costs are summarized in Table 1.
Available data for the estimation of costs of atrial fibrillation-related health care services in Portugal.
| Hospital admissions | |
| Type of data | Tariff |
| Code used to estimate costs of AF-related hospitalization | DRG for arrhythmia |
| Specific to patients with IPG? | No |
| ED visits | |
| Type of data | Hospital cost |
| Specific to AF/arrhythmia | None |
| Specific to patients with IPG? | No |
| Separate cost for ED visit when subsequently admitted? | No |
| Unscheduled outpatient visits | |
| Type of data | Hospital cost |
| Specific to AF/arrhythmia | None |
| Specific to patients with IPG? | No |
AF: atrial fibrillation; DRG: diagnosis-related group; ED: emergency department; IPG: implanted pulse generator.
Specific AF-related hospitalization costs are not available at hospital level in Portugal. Therefore, hospitalization costs were estimated on the basis of DRG tariffs, as in Boriani et al.14 for the UK, Italy and Spain.
As in Spain, Portuguese hospitals have overall budgets that are linked to DRGs. DRG tariffs are the established price for treating patients outside the coverage area and are commonly associated with the cost of hospitalization for specific diseases or procedures. The tariffs are published by the Central Administration of the National Health System (ACSS).16
Since different DRGs are available (for ablation and arrhythmia) and vary according to different levels of severity,16 a weighted average for the cost of hospitalization was estimated as in Boriani et al.14 Regarding DRG choice, it was considered that 4.5% of patients are coded for ablation (all-patient refined [APR]-DRG 175, percutaneous cardiovascular procedures without acute myocardial infarction) and the other 95.5% are coded as APR-DRG 201 (cardiac arrhythmia and conduction disorders). These percentages are based on the number of patients who underwent ablation in the MINERVA trial.13
For the choice of level of severity, MINERVA showed that 20% of these hospital admissions have complications. For this reason, in this analysis it was considered that 20% of hospital admissions are classified as severity level 3 to accommodate possible complications and the other 80% of hospital admissions were considered severity level 1.
The costs of ED and outpatient visits were collected from an ACSS database recording costs of various activities of hospitals in the Portuguese National Health System.17 In both cases the average cost was considered. These costs are not specific to AF-related visits; for outpatient visits the average cost of cardiology outpatient visits was used.
The average cost for each service (hospitalization, ED visit and outpatient visit) in Portugal is presented in Table 2. The cost of the event was assumed to be independent of the pacing modality and thus only the frequency of visits varied.
Tariffs and provider costs of atrial fibrillation-related health care services in Portugal (values in euros).
| Hospitalization (a) | 1175.92 |
| Arrhythmia – APR-DRG 201 | |
| Severity level 1 | 776.44 |
| Severity level 2 | 1231.62 |
| Severity level 3 | 2169.61 |
| Severity level 4 | 5233.34 |
| Ablation – APR-DRG 175 | |
| Severity level 1 | 2103.80 |
| Severity level 2 | 2770.33 |
| Severity level 3 | 5012.60 |
| Severity level 4 | 11435.74 |
| Emergency visits | 150.34 |
| Outpatient visits | 110.22 |
APR-DRG 201: cardiac arrhythmia and conduction disorders; APR-DRG 175: percutaneous cardiovascular procedures without acute myocardial infarction.
Weighted average assuming 4.5% of hospitalizations are coded as DRG 175 (the other 95.5% are coded as DRG 201) and that 80% of hospitalizations are classified as severity level 1 while the other 20% are classified as severity level 3.
Data sources: hospitalization: Order in Council 234/201516; emergency visits and outpatient visits: average cost from ACSS.17
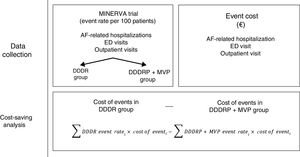
To estimate the savings from the DDDRP + MVP pacing algorithm, the same methodology as in Boriani et al.14 was used: the number of events reported was estimated as event rates per 100 patients and the costs per event were multiplied by the event rate, giving the costs of AF-related hospitalizations for both groups. The difference between the groups represents the cost savings per year (Figure 1).
The cost savings over a 10-year period were calculated to reflect the total saving over the lifetime of the device. Event rates were assumed to be constant over the device's lifetime. As AF is a progressive disease, it is unlikely to improve during a longer follow-up period and the frequency of hospital care is thus unlikely to fall. The discount rate considered was 5% per year, which is the discount rate suggested by the Portuguese methodological guidelines.18 A mortality rate of 2.3% was assumed, in line with the MINERVA trial results.13
An additional analysis was performed considering the total number of patients who could benefit from this pacing modality in Portugal. According to the White Book of the European Heart Rhythm Association, in 2014 there were 8830 pacemakers implanted in Portugal.19 The European Society of Cardiology attributes 36% of pacing indications to AF plus atrioventricular block and sinus node dysfunction, which is the percentage of patients who could benefit from the DDDRP + MVP pacing modality.20 This suggests that 3179 patients per year in Portugal could benefit from the new pacing algorithm.
ResultsIn the MINERVA trial (Table 3), the 383 patients assigned to the DDDRP + MVP pacing modality had a significantly reduced event rate, and 42% fewer AF-related hospitalizations and 68% fewer ED visits, compared to the 385 patients in the control group (DDDR).13 The difference in outpatient visits between the two groups was not significant. Table 3 reports the results of the MINERVA trial.
Health care event rates stratified by group in the MINERVA trial.
| Event rate per 100 patients per year | IRR | Difference | Reduction | p | ||
|---|---|---|---|---|---|---|
| DDDR (controls) | DDDRP + MVP | |||||
| Hospitalization | 4.3 (3.0 to 6.1) | 2.5 (1.5 to 4.0) | 0.58a | 1.8 (1.0 to 3.2) | 42% | 0.003 |
| ED visit | 2.7 (1.7 to 4.2) | 0.9 (0.4 to 1.9) | 0.32a | 1.8 (0.9 to 3.2) | 68% | <0.001 |
| Outpatient visit | 2.4 (1.5 to 3.9) | 2.9 (1.8 to 4.5) | 1.2 | −0.5 (−1.3 to 0.1) | NS | 0.310 |
DDDR: dual-chamber pacing; DDDRP: atrial preventive pacing and atrial antitachycardia pacing; ED: emergency department; IRR: incidence rate ratio; MVP: manged ventricular pacing; NS: not significant.
Costs were calculated for each group as the event rates reported multiplied by the respective costs. Table 4 presents the costs per year for each group and savings (the difference in costs between the two groups).
Cost savings calculated for the Portuguese health care setting (values in euros).
| Average tariff/ costs per episode | Costs per 100 patients per year | Cost savings per 100 patients | |||
|---|---|---|---|---|---|
| DDDR (controls) | DDDRP + MVP | Per year | 10-year period | ||
| AF-related hospitalization | 1176 | 5056 | 2905 | 2152 | 15858 |
| AF-related ED visit | 150 | 406 | 131 | 275 | 2027 |
| Outpatient visit | 110 | 265 | 321 | −56 | −414 |
| Total | 5727 | 3356 | 2371 | 17471 | |
AF: atrial fibrillation; DDDR: dual-chamber pacing; DDDRP: atrial preventive pacing and atrial antitachycardia pacing; ED: emergency department; MVP: managed ventricular pacing.
Opting for the DDDRP + MVP pacing algorithm results in savings of 2371 euros per 100 patients per year and 17471 euros over a 10-year period. The MINERVA pacing algorithm could reduce health care costs in this patient group in Portugal by 41%. The sensitivity analysis (Table 5) presents confidence intervals for the cost savings estimated using the confidence intervals of event rates. The lower bounds still represent a reduction of 19% in health care utilization costs.
Sensitivity analysis of cost savings for Portugal (values in euros).
| Per year | 95% CI | 10-year period | 95% CI | |||
|---|---|---|---|---|---|---|
| Lower bound | Upper bound | Lower bound | Upper bound | |||
| AF-related hospitalization | 2152 | 1764 | 2469 | 15858 | 15470 | 16176 |
| AF-related ED visit | 275 | 195 | 346 | 2027 | 1948 | 2098 |
| Outpatient visit | −56 | −33 | −66 | −414 | −391 | −424 |
| Total | 2371 | 1926 | 2749 | 17471 | 17027 | 17849 |
AF: atrial fibrillation; CI: confidence interval; ED: emergency department.
Considering the number of patients who could potentially benefit from this pacing modality each year – around 3179 patients – Portugal could save 75369 euros a year. These same 3179 patients would represent savings of around 555410 euros by the end of a 10-year period (Table 6).
DiscussionThe benefits of the DDDRP + MVP algorithm were established in the MINERVA trial. In Portugal, these benefits represent a potential cost saving of 2371 euros per 100 patients in the first year and 17471 euros over a 10-year period, and a total of 75369 euros per year and 555410 euros over 10 years if all potential patients were considered.
Compared to the estimated cost savings for other countries in Boriani et al.,14 the savings for Portugal are substantially lower. Two main factors contribute to this difference. Firstly, costs are lower in Portugal; and secondly, a conservative approach was taken regarding the costs of hospitalizations and ablation. It was assumed that 80% of hospital admissions were not severe, and were therefore classified as the lowest severity level (out of 4). The 20% of hospital admissions with complications were considered to be classified as severity level 3. This represents the lowest cost-saving scenario, meaning that the savings could potentially be higher. Moreover, the Portuguese methodological guidelines for health care cost analysis suggest the use of a 5% discount rate, which is a more conservative rate than that used by Boriani et al.14 (3.5%). Using a lower discount rate would lead to higher cost savings over a 10-year period.
The cost-saving analysis only took AF-related hospitalizations into account. Optimization of the algorithm could, however, potentially reduce other hospitalizations related to heart failure and stroke. This also means that savings could be higher than those estimated in this analysis.
A data collection limitation arises directly from the MINERVA trial, in which only two years of health care utilization data were collected, on which the trial's results depend. The benefits of the algorithm are applicable to the lifetime of the device and thus differences in the number of hospital admissions and ED visits are expected to remain at least the same between the treatment and control groups.
As this cost-savings analysis focuses on reduction of health care utilization, the price difference of devices with the new algorithm was not taken into consideration. This study was not intended to analyze the relative cost-effectiveness of devices but to determine the potential of the new algorithm. The main reason for this choice is the characteristics of the medical devices market, in which prices tend to decline and converge. In this context, any analysis in which assumptions are made about pricing is liable to become rapidly outdated.
ConclusionThe combination of atrial preventive pacing, a new generation of atrial antitachycardia pacing, and an algorithm to minimize the detrimental effect of right ventricular pacing reduces recurrent and permanent AF. This results in a fall in AF-related health care utilizations. The new DDDRP + MVP pacing mode could contribute to significant costs savings in the Portuguese health care setting.
Conflicts of interestDr. João de Sousa, Dr. Pedro Marques, Dr. Vítor Martins, Dr. Hipólito Reis and Dr. Luís Duarte participated in and received investigator fees for the MINERVA trial from Medtronic. Dr. Giuseppe Boriani received modest speaker fees from Boston Scientific and Medtronic for the initial MINERVA trial. Dr. Luigi Padeletti received modest research grants and/or consultant/advisory board grants from Boston Scientific, Medtronic and St Jude Medical for the initial MINERVA trial. Inês Joaquim, Diogo Monteiro, Claudia Wolff and Andrea Grammatico are employees of Medtronic.