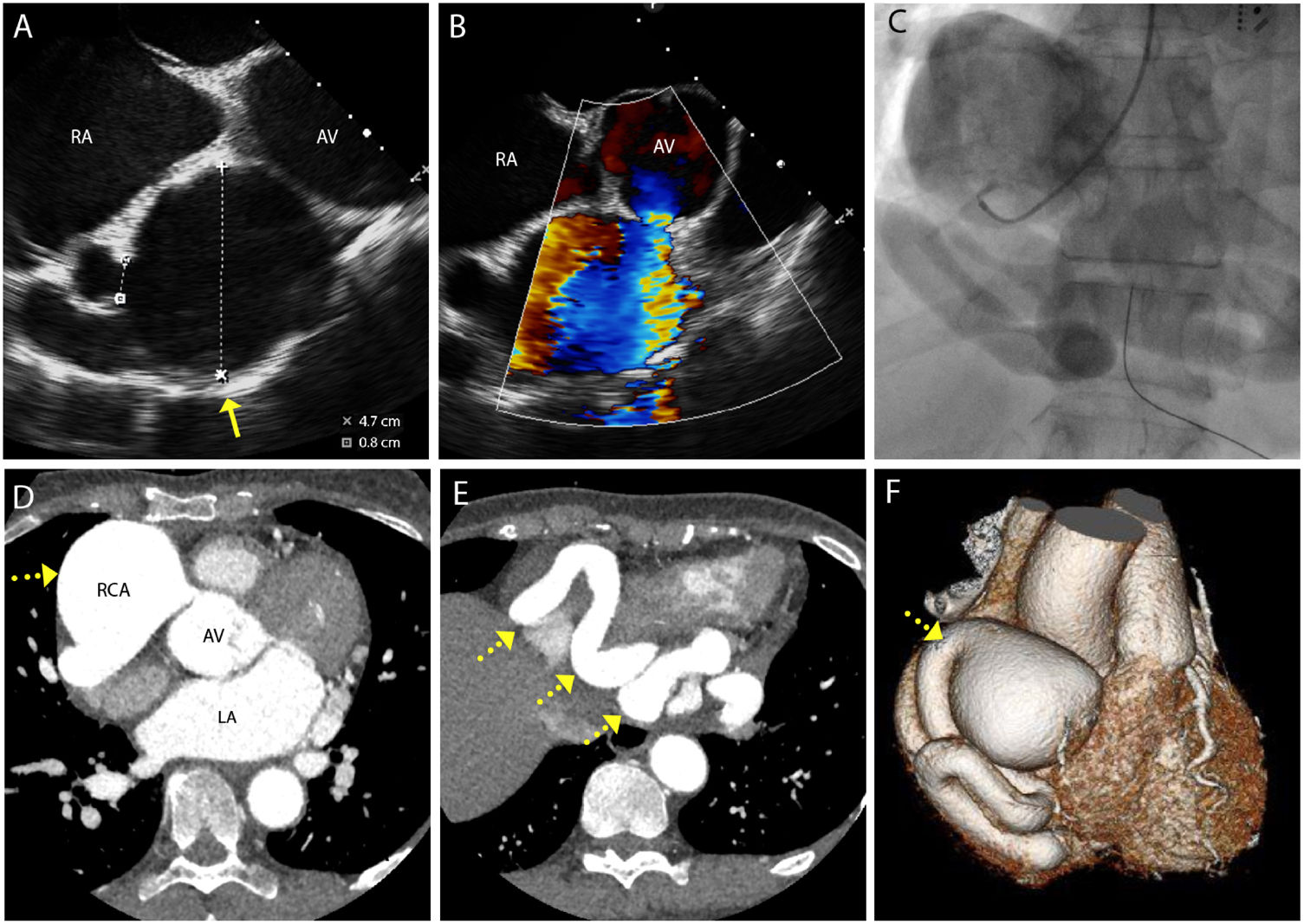
A 61-year-old-woman with paroxysmal atrial fibrillation and symptomatic palpitations, particularly when lying flat, was referred for catheter ablation. Pre-procedure transesophageal echocardiography revealed a 47 mm aneurysmal structure adjacent to the right atrium (RA) and aortic root with turbulent inflow from the right coronary artery (RCA) (Figure 1, Panels A-B, video S1). It also showed several abnormal vessels in the atrioventricular groove and high velocity jets entering a dilated RA. These findings were considered as suspicious for an RCA aneurysm with arterial shunting into the RA via the coronary sinus (CS). Catheter ablation was therefore abandoned, and additional imaging obtained. Coronary angiography demonstrated a large RCA aneurysm with the remainder of the vessel grossly ectatic and appearing to drain into a dilated CS (Figure 1, Panel C, video S2). Right heart catheterization demonstrated a significant left to right shunt (Qp:Qs ratio of 1.50). Computed tomography coronary angiography (CTCA) confirmed a large saccular RCA aneurysm (58×56 mm) with CS fistulation. It also demonstrated enlarged right heart and main pulmonary artery suggestive of significant volume overload (Figure 1, Panels D-F). Following a multidisciplinary team discussion, the patient underwent a successful RCA ostial repair with a pericardial patch and aneurysm decompression. The postoperative recovery was uneventful. At one-year follow-up, the patient remained asymptomatic.
(A) Transesophageal echocardiogram shows a large aneurysmal structure (yellow arrow) adjacent to the right atrium and aorta valve (measuring 47 mm in diameter with (B) turbulent flow on color flow doppler. (C) Coronary angiography demonstrates a large right coronary artery aneurysm proximally and a grossly ectatic vessel. (D-E) Computed tomography coronary angiography confirms a large proximal right coronary artery aneurysm (yellow interrupted arrow) with the remainder of the vessels ectatic and with a tortuous course (yellow interrupted arrow). (F) Computed tomography coronary angiography 3D reconstruction of right coronary artery aneurysm (yellow interrupted arrow).
Most coronary fistulae are small and an incidental finding; however, close monitoring is warranted as they are prone to enlargement and eventually become symptomatic. CTCA has excellent spatial and temporal resolution and is the preferred imaging modality to inform decisions on percutaneous closure or open surgical ligation. Treatment remains controversial and should be guided by an experienced multidisciplinary team. Most would advocate intervention in symptomatic patients and in large aneurysmal fistulae with significant shunts.
Video S1. Transesophageal echocardiogram
Video S2. Coronary angiography
Statement of consentThe authors confirm that written consent for submission and publication of this case report including image(s) and associated text has been obtained from the patient in line with COPE guidance.
ContributionABG, ML and MTBP conception and drafting of the manuscript. AK performed and reported the cross-sectional imaging. AK and YB reviewed and edited the manuscript. All authors gave final approval prior to submission.
Conflicts of interestThe authors have no conflicts of interest to declare.